Thymidylate Synthase Predicts Response to Chemo in NSCLC
A new study suggests that expression of the enzyme thymidylate synthase can be used as a predictive marker for lung cancer patients undergoing chemotherapy.
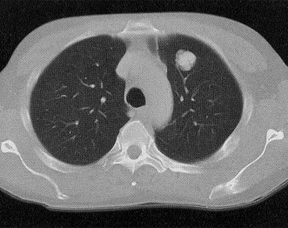
Single CT slice of a 3-cm left upper lobe adenocarcinoma of the lung
A new phase II study suggests that expression of the enzyme thymidylate synthase (TS) can be used as a predictive marker for patients with non-squamous non–small-cell lung cancer undergoing chemotherapy. Benefits of cisplatin plus pemetrexed over cisplatin plus gemcitabine were more pronounced in TS-negative patients than in TS-positive patients.
“Thymidylate synthase,” said Myung-Ju Ahn, MD, of Sungkyunkwan University School of Medicine in Seoul, in a press release, “is targeted by pemetrexed, which is the most widely used chemotherapeutic regimen in the treatment of non-squamous NSCLC.” Previous work has shown that the cisplatin/pemetrexed combination is superior to cisplatin/gemcitabine in non-squamous NSCLC, but levels of TS could predict the level of response.
In this study, 315 non-squamous NSCLC patients were first stratified as either TS-positive (more than 10% of tumor cells express TS) or TS-negative, and then randomized to cisplatin plus either pemetrexed or gemcitabine. Results were presented at the European Society of Medical Oncology (ESMO) 2014 Congress in Madrid.
The objective response rate in the cisplatin/pemetrexed patients who were TS-negative was 47%, compared with 21.1% in the cisplatin/gemcitabine group. In the TS-positive patients, meanwhile, the objective response rates were 40.3% for cisplatin/pemetrexed patients and 39.2% for cisplatin/gemcitabine patients (P = .008).
The median progression-free survival of the TS-negative cisplatin/pemetrexed group was 6.4 months; for TS-negative cisplatin/gemcitabine patients, the median progression-free survival was 5.5 months (P = .013). In the TS-positive patients, progression-free survival was 5.9 months and 5.3 months, respectively, a much smaller difference (P = .64). Overall survival analysis did not yield significant differences between the groups, though TS-negativity was an independent prognostic factor for overall survival with a hazard ratio of 0.64 (95% CI, 0.45-0.90).
“In non-squamous cell NSCLC, TS-negative patients get more clinical benefit from pemetrexed/cisplatin combination therapy,” Ahn said. The multivariate analysis that showed the correlation with overall survival-along with younger age and EGFR mutation status-suggests that TS could indeed be used as a predictive biomarker.
“This study opens the gates for thymidylate synthase-customized chemotherapy in advanced NSCLC,” said Rafael Rosell, MD, PhD, of the Catalan Institute of Oncology in Spain, who was the discussant for the study. “Over-expression of TS could behave as an oncogene and therefore TS could be not only a predictive marker of response to antimetabolite drugs, but also a prognostic marker. Therefore, it could be of interest to see what the relevance of using TS as an overall biomarker could be for [predicting chemotherapy outcomes].”