Trouble Sleeping During Breast Cancer Adjuvant Chemotherapy Treatments
The patient, “TB,” is a 44-year-old Caucasian, married woman with three daughters, 21, 18, and 10 years of age.
The patient, “TB,” is a 44-year-old Caucasian, married woman with three daughters, 21, 18, and 10 years of age. The family lives in a small rural town. TB works full-time on a night shift (10:00 PM–6:30 AM) unloading trucks and restocking shelves at a store. She has been a 1 pack/day smoker for 20 years and was premenopausal at diagnosis. Diagnosed with hypothyroidism in 2006, TB takes Synthroid (levothyroxine) at 100 mcg daily. Her husband, a self-employed construction worker, recently had a heart attack and is at home during the day.
TREATMENT SUMMARY
In summer 2009, TB noted a lump in the upper outer quadrant of her right breast and was diagnosed with stage II infiltrating ductal carcinoma (T2, N0, M0, ER positive, PR positive, HER2/neu negative). Three weeks after lumpectomy surgery, she began four cycles of dose-dense chemotherapy with Adriamycin (doxorubicin)/Cytoxan (cyclophosphamide) and her menstrual periods stopped. She started Taxol (paclitaxel) chemotherapy shortly thereafter and developed severe hand-and-foot syndrome after the first dose, which led to both dose reduction and delay. She is currently taking Neurontin (gabapentin) at a dosage of 300 mg twice a day for neuropathic pain. Her paclitaxel treatments were switched to weekly doses and she resumed her treatments 3 weeks after the first dose.
NURSING MANAGEMENT
At the clinic appointment before her first weekly paclitaxel treatment, the nurse practitioner screened TB for sleep disturbances, and she screened positive. The nurse practitioner referred TB to the Oncology Clinical Nurse Specialist (CNS), who assessed TB's sleep using the Insomnia Severity Index (ISI).[1] TB's ISI score of 14 indicated that she was experiencing subthreshold insomnia (normal value, 7) and could benefit from treatment. TB agreed to have the CNS, who had been trained by a sleep psychologist, assist her to improve her sleep over a 6-week period.
During their first session at the infusion center before her treatment, the CNS interviewed TB regarding her current sleep using the Brief Sleep History.[2] TB's sleep history was complicated by her schedule of working Monday through Friday from late in the evening through early morning, and sleeping during the day. She sleeps until noon on Saturday and then sleeps on Saturday and Sunday nights. When she gets out of bed on Monday morning, she does not return to bed until she returns home from work on Tuesday morning, 25 hours later. TB scheduled her paclitaxel treatments for Saturday mornings.
After TB drives 12 miles home from work, she or her daughter drives 30 miles to the infusion center. She stated that she hopes to nap while waiting for laboratory results and during her scheduled infusions. TB reported no problem falling asleep in the morning, but stated that she wakes up two to three times during the day, usually to go to the bathroom. She said that she usually spends 7 hours in bed but reported that she believes her body needs 7½ hours of sleep. Her biggest issue was that she feels her sleeping problems are “very noticeable” to others in terms of impairing her quality of life.
After obtaining TB's sleep history, the CNS coached TB to develop an individual behavioral therapy plan.[3,4] Her plan included techniques that have been demonstrated to improve sleep in adults with chronic insomnia: sleep restriction, stimulus control, relaxation therapy, and sleep hygiene.[5,6] These techniques have been found to improve sleep in cancer survivors who have completed treatment.[7,8] TB chose the sleep hygiene strategies of stopping ingestion of liquids by 6:00 AM, using the bathroom before going to bed, and taking her Synthroid and Neurontin medications as prescribed.
The CNS taught TB how to document each morning her adherence to the techniques on her plan. The CNS also instructed TB to wear a wrist actigraph on her nondominant wrist (see Figure 1). Wrist actigraphs are portable devices the size of a large wristwatch that record movement over time in the form of activity counts. Actigraphs have gained acceptance as a sensitive tool for evaluating sleep–wake and activity–rest patterns.
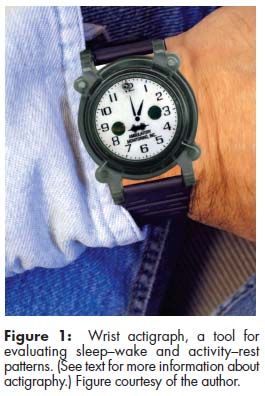
TB was also shown how to fill out a daily sleep diary that includes items such as time she went to bed, number and length of time of awakenings, and time spent awake at the end of the sleep period. Based on TB's adherence and diary, the CNS helped TB identify barriers and reinforced adherence to the plan weekly. This occurred in person after the first, fourth, and fifth weeks and by telephone consultation after the second and third weeks. Her plan was revised to include the sleep hygiene technique of wearing ear plugs, because she heard sounds from dogs and television noise when she woke during the day. TB wore the actigraph for an entire week (9:00 AM on Saturday to 9:00 AM the following Saturday) during the first and sixth weeks and repeated the ISI on the last day of the sixth week.
OUTCOME
The desired outcomes were improved subjective sleep (per ISI score) and improved objective sleep parameters (per actigraph) (Table 1). The ISI score on the first day of Week 1 was 14; when TB was assessed 6 weeks later it was 19, reflecting clinical insomnia. Despite coaching, all her sleep parameters reflected poorer sleep during TB's sixth week of paclitaxel treatments. The most remarkable finding was that TB only scheduled herself to sleep six times per week and she only slept 6 hours on those nights. The time she spent awake while she was in bed was excessive, and her sleep efficiency was 10% to 15 % lower than normal.
DISCUSSION
This case illustrates poor sleep during chemotherapy in a young wife and mother who is employed in a physically demanding job full-time on a night shift. When assessed, the patient reported that her sleeping problems were very noticeable to others in terms of impairing her quality of life. More than 50% of shift workers have reported severely reduced sleep or alertness.[9] Likewise, approximately 50% of cancer patients with a variety of diagnoses have reported sleep problems; insomnia is the most common disorder.[10,11] Sleep–wake disturbances are under-reported and under-treated in cancer patients during and after treatment. TB had not volunteered to report problems sleeping during the dose-dense chemotherapy treatments despite a high likelihood that she was experiencing problems.
The strongest evidence for managing poor sleep that is comorbid with chronic illnesses such as cancer is cognitive behavioral therapy (CBT)/behavioral therapy (BT).[12,13] CBT/BT is usually delivered by a psychologist trained to deliver behavioral sleep therapy. However, nurses trained by psychologists have delivered BT interventions effectively.[3,8] Nurses can teach patients receiving chemotherapy treatments the basic strategies to promote good sleep: go to bed when sleepy and at approximately the same time each night; get out of bed and go to another room whenever unable to fall asleep; return to bed only when sleepy again; use the bedroom for sleep and sex only; maintain a regular rising time each day; and avoid daytime napping. If needed, limit naps to 30–45 minutes.[13] Sleep hygiene techniques to promote sleep include creating a bedtime routine by winding down using a relaxation technique within 2 hours of bedtime; avoiding stimulants such as caffeine for at least 6 hours before bedtime; and creating a comfortable sleep environment by keeping the bedroom cool, dark, and quiet.
Repeating the Insomnia Severity Index 6 to 8 weeks later is recommended. If the ISI score is 8 or higher, the nurse should discuss with the oncology healthcare team referral of the patient to a CNS, social worker/psychologist, primary physician, or a sleep center. Sleep disorders including obstructive sleep apnea, restless leg syndrome, and periodic limb movement disorder need to be ruled out before assuming that the patient is experiencing insomnia. Neuropathic pain management also needs to be reassessed, as treatment for trouble sleeping has been shown to improve pain management in cancer patients.[14] TB was encouraged to continue to follow her sleep therapy plan, and her sleep will be reassessed after she completes her chemotherapy treatments.
All shift workers need to be educated about strategies to promote sleep and reduce fatigue.[15] The CNS taught TB to schedule her sleep time to include a 4-hour anchor period (ie, 9:00 AM–1:00 PM) seven nights a week regardless of whether she is working or not.[16] When she works, she should schedule her sleep from 9:00 AM–4 PM; on weekends, she should schedule her sleep from 3:00 AM–1:00 PM. The CNS also encouraged TB to take a nap on Mondays and Fridays before work to reduce the risk of falling asleep at the wheel when driving home and to the clinic.[17,18] The final recommendation was for TB to take responsibility for obtaining the sleep her body needs every day. Six hours are the minimum, but 7 to 8 hours are recommended.[19] Taking responsibility for adequate time to sleep was the hardest for TB who, like many women, was accustomed to putting her family's needs before her own.
References:
References
1. Bastien CH, Vallieres A, Morin CM: Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2(4):297â307, 2001.
2. Libbus K, Baker JL, Osgood JM, et al: Persistent fatigue in well women. Women Health 23(1):57â72, 1995.
3. Berger AM, Kuhn BR, Farr LA, et al: Behavioral therapy intervention trial to improve sleep quality and cancer-related fatigue. Psychooncology 18(6):634â646, 2009.
4. Berger AM, Kuhn BR, Farr LA, et al: One-year outcomes of a behavioral therapy intervention trial on sleep quality and cancer-related fatigue. J Clin Oncol 27(35):6033â6040, 2009.
5. Morin C, Espie C: Insomnia: A Clinical Guide to Assessment and Treatment. New York, Kluwer Academic, 2003.
6. Perlis ML, Jungquist C, Smith MT, et al: Cognitive Behavioral Treatment of Insomnia. New York, Springer, 2008.
7. Epstein DR, Dirksen SR: Randomized trial of a cognitive-
behavioral intervention for insomnia in breast cancer survivors. Oncol Nurs Forum 34(5):E51âE59, 2007.
8. Espie CA, Fleming L, Cassidy J, et al: Randomized controlled clinical effectiveness trial of cognitive behavioral therapy compared with treatment as usual for persistent insomnia in patients with cancer. J Clin Oncol 26(28):4651â4658, 2008.
9. Akerstedt T: Shift work and sleep disorders. Sleep 28(1):9â11, 2005.
10. Palesh OG, Roscoe JA, Mustian KM, et al: Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester Cancer Center-Community Clinical Oncology Program. J Clin Oncol 28(2):292â298, 2010.
11. Janz NK, Mujahid M, Chung LK, et al: Symptom experience and quality of life of women following breast cancer treatment.
J Womens Health (Larchmt) 16(9):1348â1361, 2007.
12. National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology: Cancer-Related Fatigue V.1.2010. 2010. Available at: http://www.nccn.org/professionals/physician_gls/PDF/fatigue.pdf. Accessed on March 14, 2010.
13. Page MS, Berger AM, Eaton LH: Sleep-Wake Disturbances, in Eaton LH, Tipton JM (eds): Putting Evidence into Practice. Pittsburgh, Pennsylvania, Oncology Nursing Society, 2009, pp 285â297.
14. Stepanski EJ, Walker MS, Schwartzberg LS, et al: The relation of trouble sleeping, depressed mood, pain, and fatigue in patients with cancer. J Clin Sleep Med 5(2):132â136, 2009.
15. Berger AM, Hobbs BB: Impact of shift work on the health and safety of nurses and patients. Clin J Oncol Nurs 10(4):465â471, 2006.
16. Gold D, Rogacz S, Bock N, et al: Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Public Health 82(7):1011â1014, 1992.
17. Rogers A, Holmes S, Spencer M: The effect of shiftwork on driving to and from work. J Hum Ergol (Tokyo) 30(1-2):131â136, 2001.
18. Garbarino S, De Carli F, Nobili L, et al: Sleepiness and sleep disorders in shift workers: A study on a group of Italian police officers. Sleep 25(6):648â653, 2002.
19. National Sleep Foundation: 2008 Sleep in America Poll: Summary of Findings. 2008. Available at: http://www.sleepfoundation.org/sites/default/files/2008%20POLL%20SOF.PDF Accessed on March 14, 2010.