Two Chemo Agents May Thwart Immune Response to Cancer
A new study shows two chemotherapy drugs prevalent in the clinic-gemcitabine and 5-fluorouracil-may influence the immune response in a way that facilitates tumor growth.
A new study shows two chemotherapy drugs prevalent in the clinic-gemcitabine and 5-fluorouracil-influence the immune response in a way that facilitates tumor growth. The research, conducted in mice, is published in Nature Medicine.
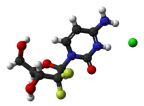
Chemical structure of gemcitabine
Franois Ghiringhelli, MD, PhD, and Lionel Apetoh, PhD, of the Institut National de la Sant et de la Recherche Mdicale and Centre Georges-Franois Leclerc in Dijon, France, and colleagues have uncovered a novel mechanism by which two chemotherapy agents activate the NLRP3 inflammasome complex within myeloid-derived suppressor cells that results in production of the cytokine interleukin (IL)-1β. This was shown by the study researchers to prevent a robust immune response against the tumor.
The experiments also showed that higher IL-1β levels led to secretion of another cytokine, IL-17, a pro-inflammatory cytokine, by CD4+ T-cells. The presence of IL-17 limited the antitumor effect of 5-fluorouracil and enhanced growth of mouse tumors. IL-17 has previously been shown to promote cancer growth and tumor progression.
“These results unravel the ambivalent effect of gemcitabine and 5-fluorouracil in the antitumor immune response,” conclude the authors in the publication.
According to Jeff Weber, MD, PhD, of the Moffitt Cancer Center in Tampa, Florida, while this study is well done and highlights the complexity of the potential counteracting effects of frequently used chemotherapy, there are also limitations. The study focused more on 5-fluorouracil than gemcitabine, and there is only modest human evidence that confirms the hypothesis.
A concern about the clinical application of this research, according to Weber, is that 5-fluorouracil is given in along with leucovorin, which enhances the activity of the chemotherapy, and is often given in combination with bevacizumab and oxaliplatin, which “may counteract some of the immune suppressive mechanism noted in [the study],” said Weber.
Whether chemotherapy promotes or prevents the patient’s immune system from acting on his or her cancer is a subject for debate. There has been recent evidence showing chemotherapy can systemically facilitate immunosuppression. However, there is also evidence that certain chemotherapies enhance an antitumor response by the immune system. The challenge, said Ghiringhelli, is to dissect the immune effect of different drugs in order to design better combinations to enhance the immune response.
Weber agrees. “Further studies are necessary, including expanding work with gemcitabine, to further understand the clinical implications of this outstanding work.” Because there is evidence that certain chemotherapies have a positive effect on a patient’s immunity, understanding which treatments and under which circumstances is crucial.
As a gastrointestinal cancer specialist, Ghiringhelli sought to understand the effect of these two chemotherapies, which are effective but never lead to a cure for patients. 5-fluorouracil in particular is often used to treat metastatic colon cancer. “We believe that it is important to determine the effect of this treatment on the immune system, and if it could be combined with immunotherapy to enhance its effect,” said Ghiringhelli.
The new study suggests ways to bypass the protumor growth activity of gemcitabine and 5-fluorouracil. Mice in the study that did not express integral factors of the inflammasome complex, either NLRP3 or CASP1, had a more robust antitumor effect following treatment with either chemotherapy. While the wild-type mice treated with chemotherapy died by day 30 post-treatment, 30% to 42% of the mutant mice were alive and tumor free at day 60 post-treatment. A recombinant IL-1 antagonist also enhanced the antitumor response to either chemotherapy agent in mice.
According to Ghiringhelli, this new mechanism is dependent on the type of chemotherapy, suggesting that those “that target thymidylate synthetase could mediate this effect.” 5-fluorouracil is an antimetabolite that inhibits the thymidylate synthetase required for DNA synthesis.
Chronic inflammation has been previously linked to cancer initiation and progression, including over-activation of IL-1β. The differences in the response of the immune system to different chemotherapies may have to do with the mechanism of the therapy. The authors cite previous studies which show another type of chemotherapy, anthracycline, can facilitate an anticancer immune response through activation of acute inflammation and immunogenic cell death, a specific type of tumor cell death that results in an immune response.
An increase in IL-1β has also been shown in colorectal patients treated with 5-fluorouracil, according to the authors. This hints that combining inhibitors of either the inflammasome or IL-1β with either gemcitabine or 5-fluorouracil could enhance the antitumor effect. “The inhibition of this pathway could be useful to enhance the efficacy of this [chemotherapy],” said Ghiringhelli.
A phase I trial to show if an inhibitor of IL-1β can reverse the resistance to 5-fluorouracil in patients with metastatic colon cancer is currently ongoing. “That an IL-1β antagonist, already used in clinical practice, may improve the effects of existing chemotherapy regimens by reducing the immune suppression detected in this work, is compelling but depends on further experiments using drugs like 5-fluorouracil in situations as they are used in patients,” said Weber.