Two Regimens Yield Similar Survival in Advanced NSCLC
An analysis showed that etoposide-cisplatin or carboplatin-paclitaxel with RT yielded similar survival in patients with stage III non-small-cell lung cancer.
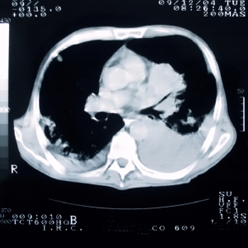
Lung cancer on CT
An analysis of Veterans Health Administration patients showed that etoposide/cisplatin (EP) and carboplatin/paclitaxel (CP) yielded similar overall survival along with radiotherapy in patients with stage III non–small-cell lung cancer (NSCLC), but EP was associated with increased morbidity. Prospective studies are still needed to determine the optimal treatment in these patients.
“There is considerable concern that CP, although better tolerated than EP, may be inferior in terms of disease control,” wrote study authors led by Rafael Santana-Davila, MD, of the University of Washington in Seattle. To better understand the differences between the regimens, researchers looked into outcomes of patients in the VA Central Cancer Registry.
The study included a total of 1,842 patients treated with concurrent radiotherapy and either EP or CP between 2001 and 2010. EP was used in 27% of the full cohort.
EP was not associated with a survival advantage over CP using any of three models used; with a propensity score adjusted model, the hazard ratio (HR) was 0.97 (95% CI, 0.85-1.10). Results were similar with a propensity score matched cohort and a Cox proportional hazards model. There was also no survival advantage seen in centers where EP was used more than 50% of the time compared with those centers where EP was used in less than 10% of patients, with an HR of 1.07 (95% CI, 0.90-1.26).
The number of hospitalizations was greater in EP patients, with a mean of 2.4 vs 1.7 for CP patients (P < .001). Outpatient visits were also increased with EP, at 17.6 vs 12.6 (P < .001). EP patients were more likely to have at least one VA encounter for an infectious complication (47% vs 39.4%; P = .0022), acute kidney injury/dehydration (30.5% vs 21.2%; P < .001), nausea/vomiting (13% vs 8.2%; P = .0017), and mucositis/esophagitis (18.6% vs 14.4%; P = .0246).
Though the similar survival and increased morbidity with EP suggest CP may be the preferred treatment, Santana-Davila said in an email that “the study is not able to provide a firm recommendation. It has many limitations, and although we tried to adjust for confounders with several techniques, it is still a retrospective study.”
Those limitations include a lack of data on dose or duration of therapy, and there were treatment differences such as an increased rate of consolidation chemotherapy with CP patients. The reliance on coded administrative data to identify toxicities is also less reliable than methods used in clinical trials.
“The only way we could provide firm recommendations would be with a phase III randomized trial,” Santana-Davila said. In the meantime, the authors concluded that these results may simply help guide treatment decisions in stage III NSCLC patients.