UGN-102 Shows Durable Responses, Tolerability in Recurrent Low-Grade NMIBC
Results from the phase 3 ENVISION trial suggest UGN-102 could be a non-surgical alternative to TURBT for recurrent low-grade intermediate-risk NMIBC.
Results from the phase 3 ENVISION trial suggest UGN-102 could be a non-surgical alternative to TURBT for recurrent low-grade intermediate-risk NMIBC.
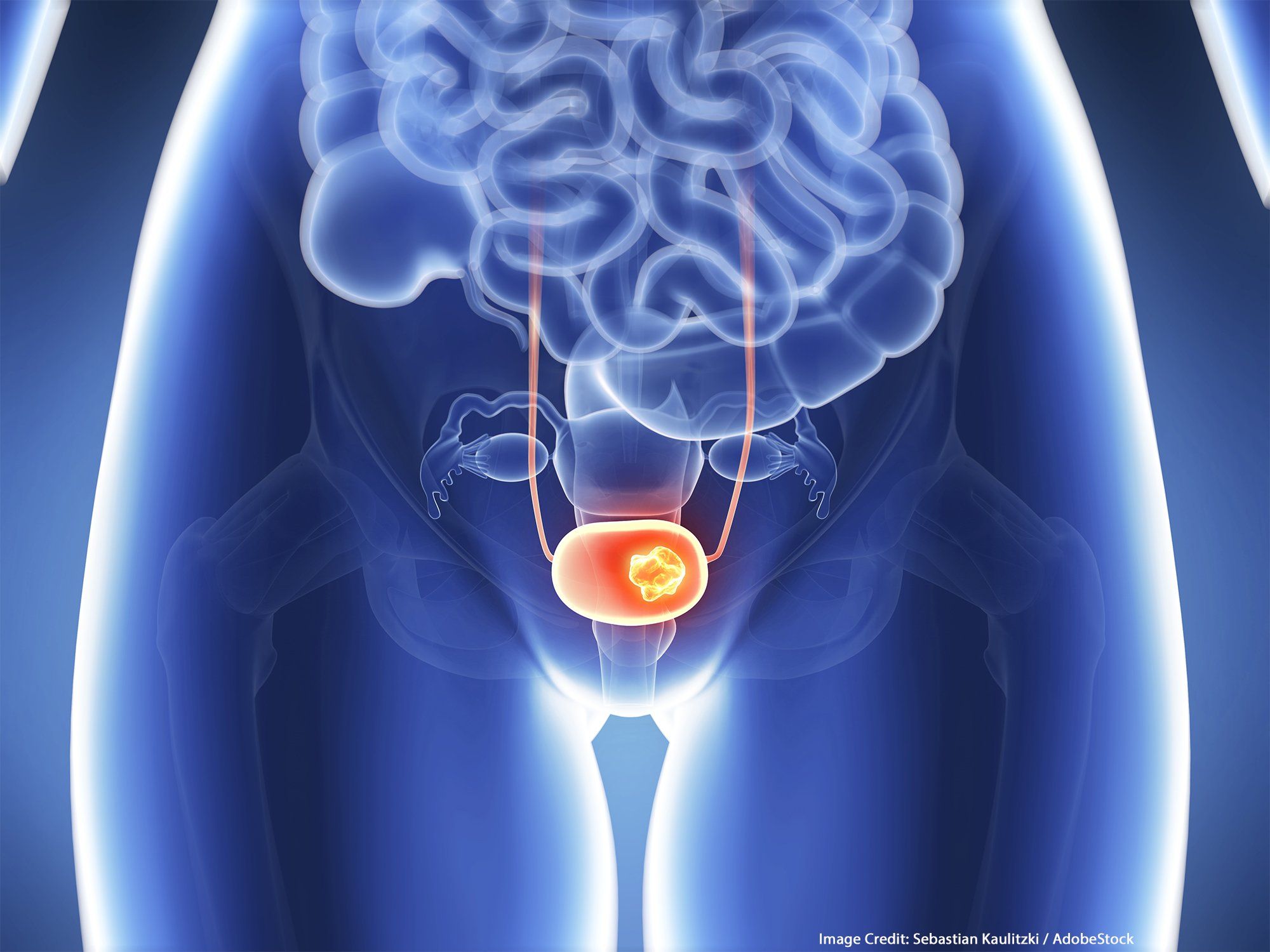
For patients with recurrent low-grade intermediate-risk non–muscle-invasive bladder cancer (NMIBC), UGN-102 elicited a complete response (CR) rates, as well as positive tolerability, according to 18-month follow-up data from the phase 3 ENVISION trial (NCT05243550) presented at the 2025 American Urological Association Annual Meeting.1
Previously, it was reported that the primary end point of CR at 3 months was achieved by 79.6% (95% CI, 73.9%-84.5%) of those who received UGN-102 (n = 191/240).2 Updated findings showed that those who achieved a CR had a high probability of remaining disease free 18 months later.1 Specifically, the Kaplan-Meier estimate of remaining a complete responder was 80.6% (95% CI, 74.0%-85.7%).
“This is very unusual. I think the most notable aspect of this study is that we’re seeing durability of response that exceeds what we typically know for TURBT, and this makes sense based on the treatment. When we do TURBT, we have to resect what we can see, and we know…we have limitations in how well we do [this],” Sandip M. Prasad, MD, MPhil, of Morristown Medical Center/Atlantic Health System in New Jersey, said in a presentation of the data. “The gel coats the entirety of the urinary lining, and some of the recurrences that we probably see at 3, 6, or 9 months are just tiny tumors we didn’t see initially. But the gel would treat those, because you don’t have to see anything; it coats every part of it. Therefore, the durability makes sense from the mechanism of how this drug works.”
Low-grade, intermediate-risk NMIBC is a highly recurrent, persistent cancer that recurs despite treatment with TURBT, the current standard of care. “TURBT, with or without adjuvant treatment, remains inadequate treatment for this,” Prasad said. UGN-102 is a reverse thermal gel. He explained that when the compound is placed on ice, it becomes a liquid and can subsequently be instilled into the body. Once it reaches body temperature, it will form a gel that coats the entire lining of the urinary surface. “It will maintain contact time for up to 6 hours; really, that’s the secret sauce of this agent, and the active chemical is mitomycin.” He underscored that UGN-102 is primary, nonsurgical chemoablation, representing a novel approach.
The prospective, multinational, single-arm, phase 3 study enrolled patients with low-grade NMIBC who had intermediate-risk disease, defined as having 1 or 2 of the following: multiple tumors, solitary tumor greater than 3 cm, or early or frequent recurrence.3 Patients needed to have negative voiding cytology for high-grade disease within 8 weeks prior to screening; acceptable organ and bone marrow function; and an anticipated life expectancy of at least the duration of the study.
The mean size of the tumors was 2.5 cm, and 83% of the tumors were multifocal, according to Prasad.1 “So, when we asked investigators on the study, how would you typically manage these types of tumors?...Most…responded that these patients would be managed by TURBT, and I would generally agree for larger, multifocal tumors,” he said. On the study, 95% of patients (n = 240) received all 6 once weekly intravesical instillations. He added that for the 5% of patients who did not receive all 6 doses, most received 5.
The primary end point was CR at the 3-month visit, with those who achieved CR entering the follow-up period. Those who did not achieve a CR were offered standard of care. The key secondary end point was duration of response, and safety outcomes were also examined.
Regarding safety, 57.1% of patients experienced any treatment-emergent adverse effect (TEAE). The most common TEAEs with an incidence of at least 5% included dysuria (grade 1, 18.3%; grade 2, 3.8%; grade 3, 0.4%), hematuria (6.3%; 2.1%; 0%), urinary tract infection (2.5%; 4.2%; 0.4%), pollakiuria (5.0%; 1.7%; 0%), and fatigue (3.8%; 1.7%; 0%). “Grade 3, 4, and 5 AEs were extraordinarily uncommon,” Prasad said. Two patients experienced any treatment-related serious AEs: one experienced urethral stenosis and one experienced urinary retention.
References
- Prasad SM, Shishkov D, Vmihaylov N, et al. Treatment of recurrent low-grade intermediate-risk non-muscle invasive bladder cancer with UGN-102: ongoing results from a single-arm, open-label, phase 3 trial (ENVISION). J Urol. Published online April 26, 2025. doi:10.1097/01.JU.0001109848.00748.9e.01
- Prasad SM, Shishkov D, Mihaylov NV, et al. Primary chemoablation of recurrent low-grade intermediate-risk nonmuscle-invasive bladder cancer with UGN-102: a single-arm, open-label, phase 3 trial (ENVISION). J Urol. 2025;213(2):205-216. doi:10.1097/JU.0000000000004296
- A phase 3 single-arm study of UGN-102 for treatment of low-grade intermediate-risk non-muscle invasive bladder cancer (ENVISION). ClinicalTrials.gov. Updated November 4, 2024. Accessed April 27, 2025. https://clinicaltrials.gov/study/NCT05243550