Veterinary Salve Relieves Hand-Foot Syndrome
SAN FRANCISCO-An inexpensive over-the-counter veterinary preparation known as Bag Balm can curtail palmar-plantar erythrodysesthesia (hand-foot syndrome) and so eliminate the need to reduce chemotherapy dosages. Nadine Tchen, MD, reported that 8 of 12 patients treated with Bag Balm after developing hand-foot syndrome either had improvement or stabilization of symptoms, and were able to continue chemotherapy without changes in dose or schedule, following treatment with Bag Balm. Dr. Tchen is a clinical fellow in the Department of Medical Oncology and Hematology, Princess Margaret Hospital, Toronto, Ontario, Canada.
SAN FRANCISCOAn inexpensive over-the-counter veterinary preparation known as Bag Balm can curtail palmar-plantar erythrodysesthesia (hand-foot syndrome) and so eliminate the need to reduce chemotherapy dosages. Nadine Tchen, MD, reported that 8 of 12 patients treated with Bag Balm after developing hand-foot syndrome either had improvement or stabilization of symptoms, and were able to continue chemotherapy without changes in dose or schedule, following treatment with Bag Balm. Dr. Tchen is a clinical fellow in the Department of Medical Oncology and Hematology, Princess Margaret Hospital, Toronto, Ontario, Canada.
The compound, sold in familiar square green tins in most North American feed stores, is an antiseptic salve of 0.3% hydroxyquinoline sulfate in a petroleum-lanolin base. "Quinoline is the antiseptic portion of this ointment that is derived from coal tar," Dr. Tchen explained. "It keeps superficial tissue soft and provides an analgesic effect. The lanolin ointment base aids in absorbing water. The petroleum part of the base retains the water, providing temporary relief of drying of the epithelial tissues. The sulfate component of this salve inhibits bacterial growth."
Study Design
The researchers conducted a pilot study that enrolled 67 cancer patients who were scheduled for treatment with chemotherapeutic agents associated with palmar-plantar-erythrodysesthesia (PPE). Treatment regimens included liposomal doxorubicin, troxacitabine, capecitabine (Xeloda), or infusional fluorouracil.
All patients were given baseline quality-of-life questionnaires and had baseline photographs of hands and feet taken. After each course of chemotherapy patients were evaluated for any signs or symptoms of PPE. If symptoms were present, patients were again given quality-of-life and PPE self-report questionnaires, underwent objective assessment for PPE using the National Cancer Institute of Canada common toxicity criteria, and had repeat photos of hands and feet taken.
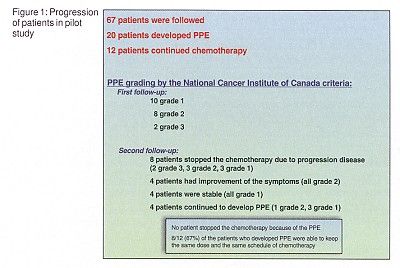
Twenty of the 67 patients developed PPE. Eight of the 20 patients with PPE stopped chemotherapy due to disease progression. The remaining 12 continued chemotherapy and were started on Bag Balm, massaged in 3 times daily after hands and feet were washed and thoroughly dried. Although four patients continued to develop PPE, four had improvement of symptoms, and four remained stable. All were able to continue chemotherapy at the same doses and schedule. No patients discontinued chemotherapy due to PPE (See Figure 1).
Clinical Trial Considered
PPE appears first as edema and discomfort of the pads of the fingers and toes, progressing within a few days to erythema, swelling, and tenderness. This is typically followed by desquamation, fissuring, and ulceration. Dr. Tchen told ONI that her group decided to try Bag Balm because of its known efficacy in relieving irritation and cracking on the udders of dairy cows and because there is no effective treatment of PPE except discontinuation of the chemotherapy.
Based on the promising results of the pilot study, chemotherapy patients at Princess Margaret Hospital are being advised to call their physicians as soon as they note any degree of pain or redness in hands or feet. Those who have such symptoms are being offered 8 to 10 days of adjuvant Bag Balm (not paid for by the Canadian national health system).
"For patients who developed PPE on the first round of chemotherapy, we don’t wait. We start Bag Balm immediately with the beginning of second and subsequent cycles," Dr. Tchen said. Her group is considering a randomized clinical trial of the salve.
How Supportive Care Methods Can Improve Oncology Outcomes
Experts discussed supportive care and why it should be integrated into standard oncology care.