
Psychology intervention service may improve gratitude, anxiety, and physical function when a hematopoietic stem cell transplant is conducted vs standard of care.
%20May%20Benefit%20From%20Venetoclax%3ASelinexor%20Combo.jpg?fit=crop&auto=format)
Patient-reported outcomes support the clinical benefits of ide-cel among patients with relapsed/refractory multiple myeloma.
A retrospective analysis of more than 17,000 patients with hematologic malignancies identified a difference in median survival between patients who received palliative care in addition to hematopoietic stem cell transplantation and those who didn’t.
Findings from a nested case-control study may enable individualized colorectal cancer risk estimations for Hodgkin lymphoma survivors who receive radiotherapy plus procarbazine.
In older patients with hematologic malignancies undergoing hematopoietic stem cell transplantation, psychological distress at baseline was associated with worse quality of life outcomes.
.jpg?fit=crop&auto=format)
An expert from the Georgia Cancer Center underscores the need to proactively address socioeconomic challenges in survivors of hematologic cancer.
Patients who are set to undergo autologous hematopoietic stem cell transplant following induction chemotherapy may have poor mobility across several domains vs an age-matched control group.

Numerous renal and cardiac indices as well as quality-of-life measures were improved with a comprehensive vs routine nursing care model.
A real-world study using a voluntary questionnaire found an association between increased pain severity and decreased health-related quality of life for patients with multiple myeloma.
Survival among patients with multiple myeloma appears to be influenced by factors such as socioeconomic status and treatment facility type.
Younger survivors of B-cell non-Hodgkin lymphoma appeared to have an increased risk of adverse health outcomes 5 or more years after diagnosis compared with older survivors.
It is important to tap into interventions that can mitigate a fear of cancer recurrence in the partners of multiple myeloma survivors in addition to improving family hardiness and social support in order to aid in patients' psychological adjustment and wellbeing.
.jpeg?fit=crop&auto=format)
Close monitoring for neurologic toxicity resulted in no long-term effects in a patient cohort treated with ciltacabtagene autoleucel for relapsed/refractory multiple myeloma.
Further investigation will determine if initial results regarding the use of anakinra as prophylaxis for orvacabtagene autoleucel in multiple myeloma is efficacious enough for use in the real-world setting.
Research in the Journal of Clinical Oncology found an association between the combination of daratumumab, lenalidomide, and dexamethasone with improved patient-reported outcomes versus lenalidomide and dexamethasone alone.
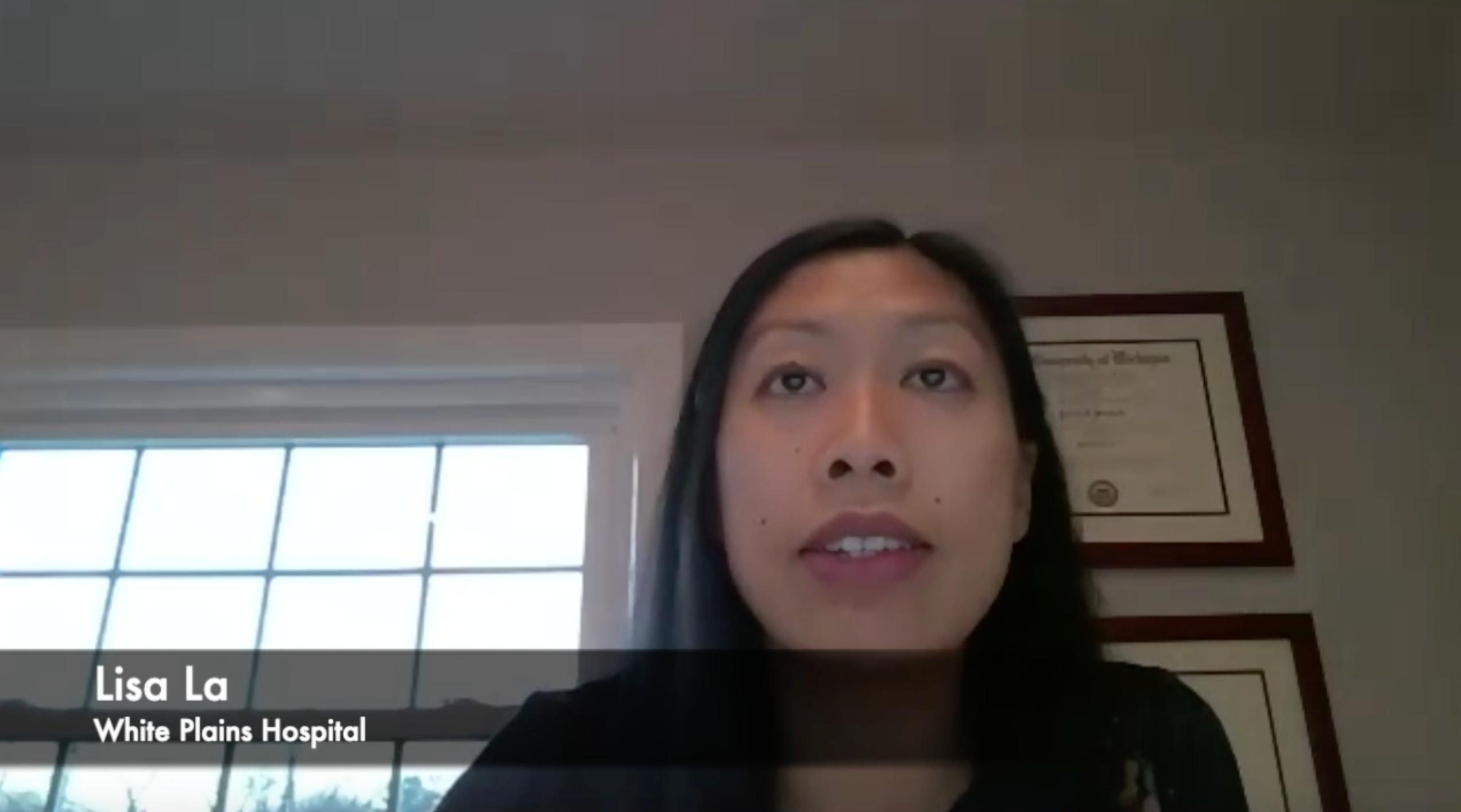
The director of clinical research in the Center for Cancer Care at White Plains Hospital spoke about what she intends to evaluate for a patient population with multiple myeloma and diabetes moving forward.

The director of clinical research in the Center for Cancer Care at White Plains Hospital spoke about the implications of a study which evaluated the impact of diabetes in patients with multiple myeloma.
Clinician Lisa La sought to evaluate differences in baseline characteristics, treatment patterns, and survival outcomes in patients with diabetes versus those without who were enrolled in the CONNECT MM Registry.

The director of clinical research in the Center for Cancer Care at White Plains Hospital explained the design of the study which evaluated diabetic versus nondiabetic patients enrolled in the CONNECT Multiple Myeloma Registry.
Patients with hematologic malignancies were found to be at increased risk for significant morbidity and mortality from COVID-19, and the risk of death appeared to be greatest in those who were older, had more severe infection, a poorer prognosis, or who decided to forego intensive treatment.

Patients with hematologic disease and a symptomatic COVID-19 infection were found to have a significantly worse prognosis than patients who were nonhematologic with COVID-19.