16 A Miami Hospital’s Infrastructure to Help Decrease Late-Stage Breast Cancer Diagnosis and Improve Health Equity
16 A Miami Hospital’s Infrastructure to Help Decrease Late-Stage Breast Cancer Diagnosis and Improve Health Equity

Background/Significance
We previously demonstrated, using the National Cancer Database, that lower income and education levels are associated with a higher stage at diagnosis of breast cancer. Expanding on this work, we analyzed publicly available data in mortality rate, focusing on Homestead Hospital’s service area in Miami-Dade County where predominantly Hispanic and Black neighborhoods face significant socioeconomic challenges.
Design and Methods
Using Miami-Dade Matters and US Census data, we evaluated the age-adjusted death rate in Miami-Dade County ZIP codes while analyzing hospital baseline data to identify opportunities to enhance screening rates. A ZIP code in Homestead Hospital’s service area has the county’s highest age-adjusted breast cancer mortality rate at 39.1 deaths per 100,000 females. In addition, the lowest percentage of high school graduates (65.5%), lowest percentage of bachelor’s degree (6.6%), highest percentage of health uninsurance (33.3%), and highest percentage of people living in poverty (32.6%) compared with the rest of Miami-Dade County. In Fiscal Year1 (FY1) 24, only 23% of Homestead Hospital’s screening mammograms were performed in Black, Hispanic, and multiracial women, despite these groups comprising 93% of the local female population. In FY1 24, there were a total of 4336 screening mammograms and diagnostic mammograms at Homestead Hospital. Of these, 16.5% (n = 716) needed additional work-up. While White had 77% of the total tests, they represented 19.6% of the tests that needed additional work-up. Minority demographic groups had 23% of the total tests but represented 80.4% of those in need of additional work-up.
Status
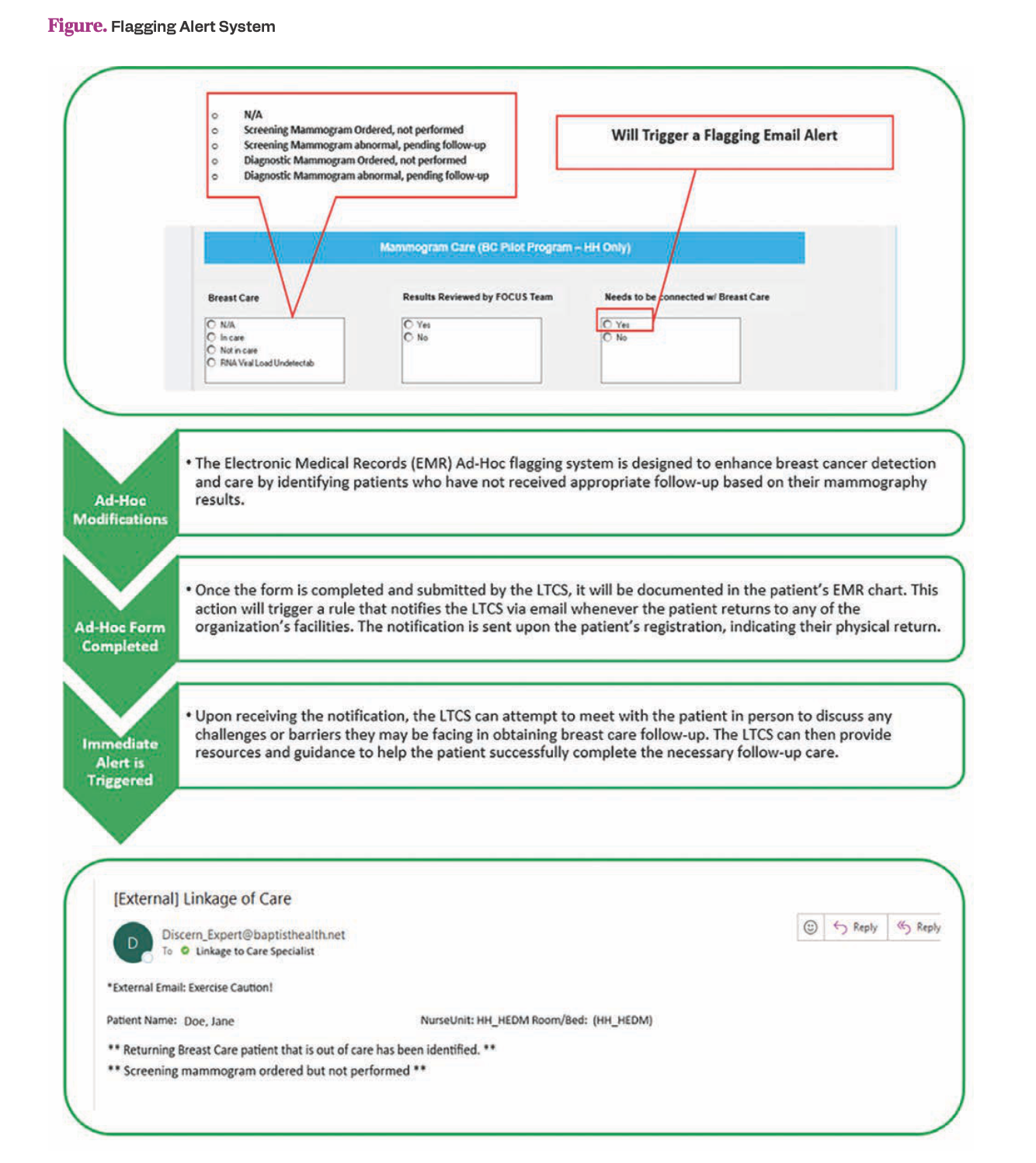
Our findings highlight significant disparities in breast cancer screening and diagnostic follow-up among minority populations in Miami-Dade County. We are developing an infrastructure to improve screening rates and a safety net for our patient population to mitigate barriers for accessing care. We educated providers at a local federally qualified health center on identifying high-risk patients. We are integrating a prediagnostic Linkage Navigator to enhance diagnostic test completion by addressing barriers and ensuring seamless linkage. We are enhancing an existing electronic flagging alert system as a safeguard, building on lessons from infectious disease screening, to identify patients needing follow-up in real-time upon returning within the health system (Figure). We are developing a dashboard to track the impact of our interventions, displaying early data from our health system transformation to reduce late-stage breast cancer diagnoses in our community.
Figure. Flagging Alert System