49 The Influence of Race on Complications in Breast Conservation Surgery: A Single Institution Study
Background
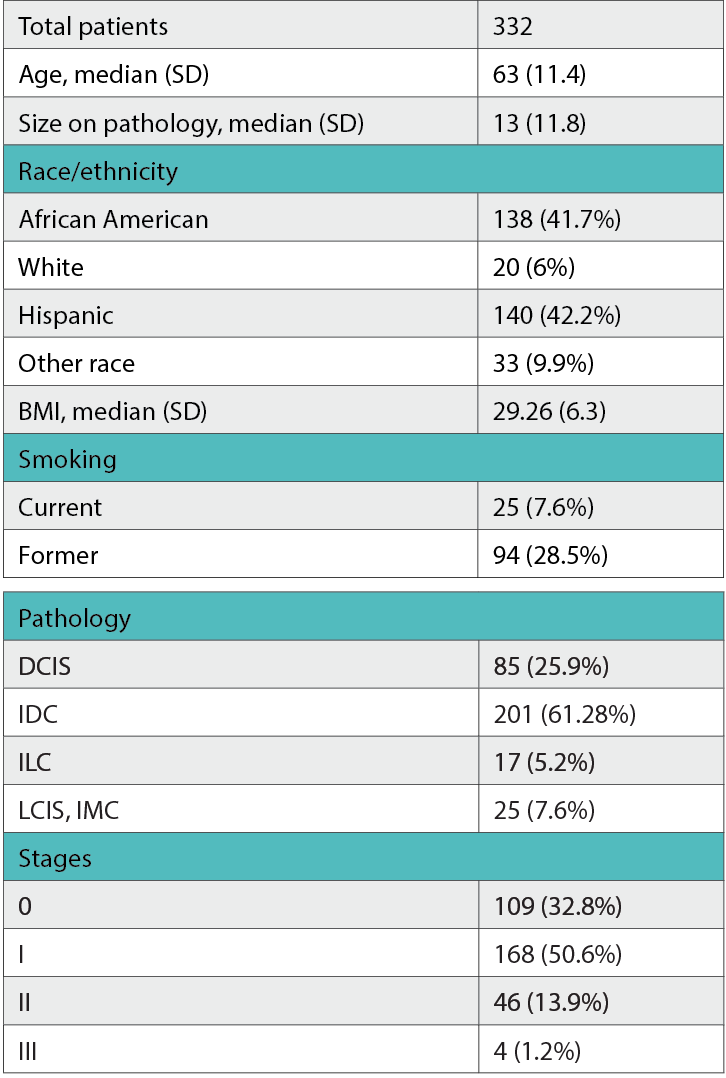
Table
Breast conservation surgery (BCS) is a low-morbidity procedure, yet its complications can impact the patient’s quality of life. Due to a paucity of literature on the social factors affecting BCS outcomes, our study aimed to assess the impact of racial factors on postoperative complications.
Methods
A retrospective chart review was conducted between 2015 and 2019 on patients undergoing BCS.
Results
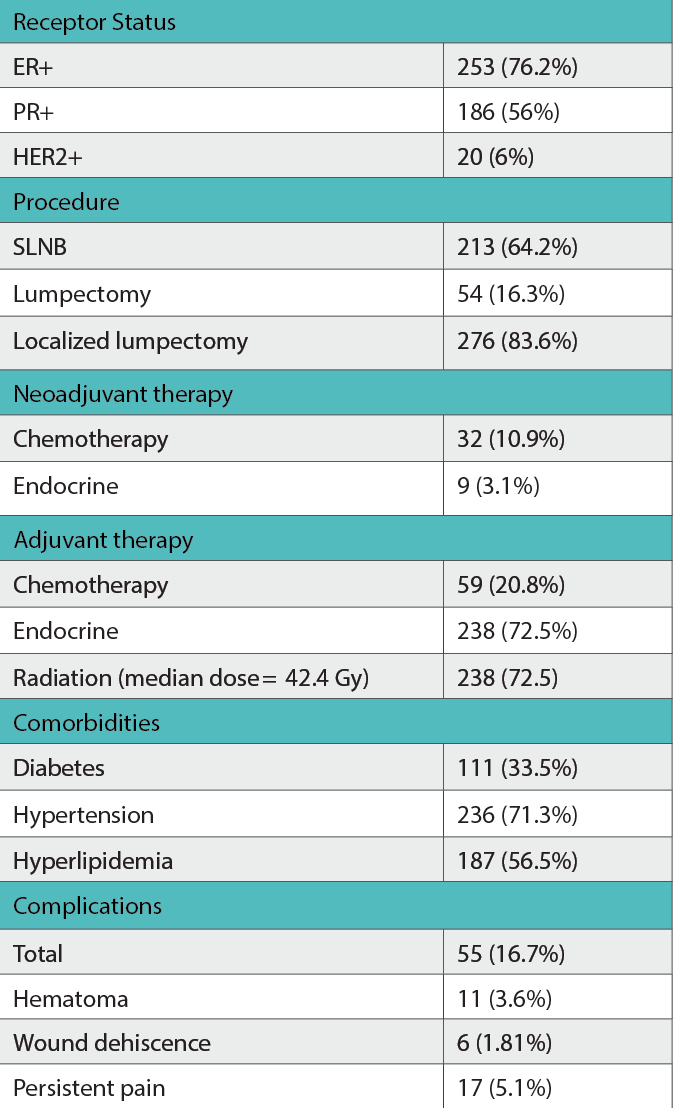
A total of 332 patients fit the criteria. Fifty-five (16.7%) had complications, of which 11 (3.6%) had hematoma, 27 (8.2%) had wound infection, 6 (1.8%) had wound dehiscence, and 17 (5.13%) had persistent pain. A total of 68 patients (20.6%) had seroma. Adjuvant therapy was delayed for 25 (7.8%) patients. Patients with normal body mass index (BMI) developed more hematomas (P = .042).
In African American (AA) patients, those with normal BMI had more complications (P = .003), hematomas (P < .001), and persistent pain (P = .011) than those with higher BMI. Additionally, AA patients with hyperlipidemia had more wound infections (P = .018).
Hispanic patients undergoing standard lumpectomy developed more infections than localized lumpectomy (P = .009). Standard lumpectomy had a higher wound infection risk than localized lumpectomy for patients 50 years or older, but this was not statistically significant (P = .054).
Table (cont.)
Conclusion
BCS is generally safe, but complications may delay adjuvant therapy. In our study, there were strong associations within race, but we did not find strong correlations between races. Nonetheless, future studies with larger sample sizes are warranted.
