5 Predictors of Axillary Complete Pathologic Response in Hormone Receptor–Positive, HER2-Negative, Clinically Node-Positive Breast Cancer
Background
Neoadjuvant therapy can downstage the axilla, reducing the need for an axillary dissection. In addition, obtaining a complete pathologic response in the axilla is associated with a better 10-year overall survival. Our institution previously reported axillary response rates in patients with hormone receptor–positive, HER2-negative (HR+/HER2–), clinically node-positive breast cancer undergoing neoadjuvant therapy in a small cohort of patients. The cohort, however, was too small for a deeper dive into potential predictors of response. In this current study, we sought to expand this cohort of patients until 2022—almost doubling the number of patients—to better evaluate for potential predictors of response.
Methods
A single-institution, retrospective cohort study included patients with HR+/HER2–, clinically node-positive breast cancer treated with neoadjuvant therapy, either endocrine or chemotherapy, between January 2011 and December 2022.
The data were divided into patients with confirmed partial response (cPR) and no cPR in the axilla. The primary outcome was to identify demographic and clinicopathologic parameters that corelated to cPR in the axilla. The χ2 test or Fisher exact test for categorical variables and the t test for continuous variables were performed. Logistic regression analysis was performed to assess clinical factors associated with the number of complications.
Results
The Demographic Profile of Patients, Tumor Characteristics, and Treatment
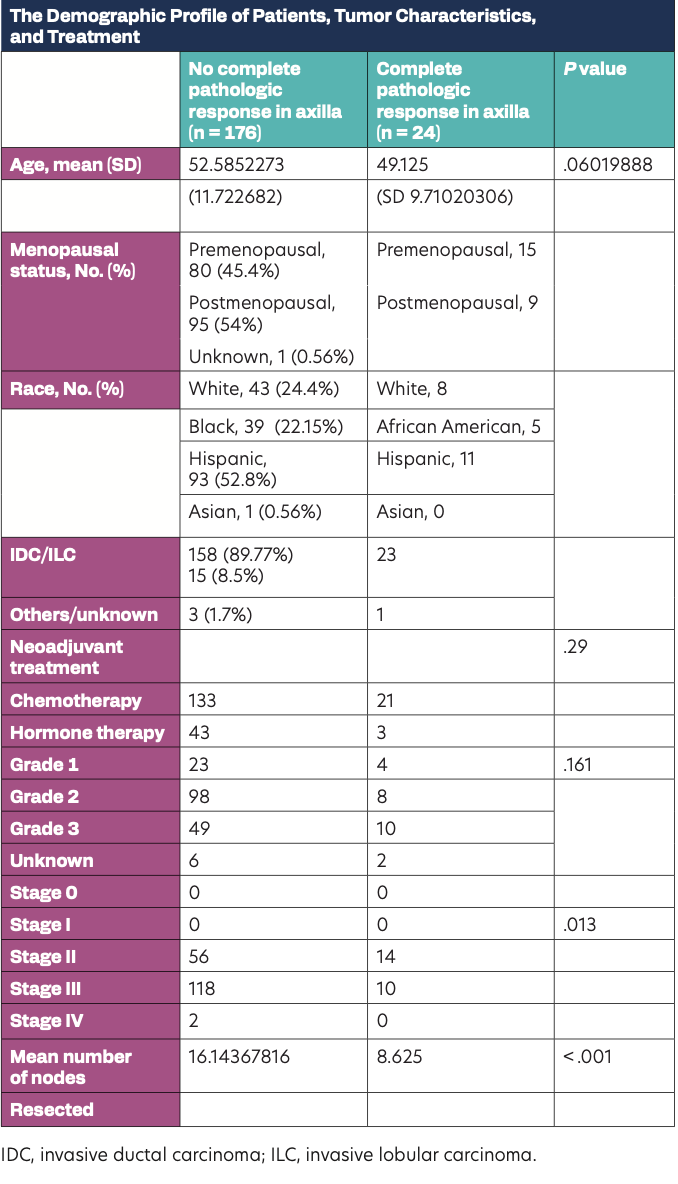
In all, 200 patients with breast cancer met the inclusion criteria. They were divided into 2 cohorts: patients with an axillary cPR rate of 12% (n = 24) and no axillary cPR 88% (n = 176). The mean (SD) age was 52.17 (11.5) years. The demographic profile of patients, tumor characteristics, and treatment are described in the Table. Among patients who underwent genomic profiling (n = 25), 76% (n = 19) had MammaPrint done, whereas 24% (n = 6) had Oncotype testing. MammaPrint was performed in2 patients found to have cPR in the axilla; it was high risk in both patients. For patients who underwent chemotherapy, approximately 13.6% achieved axillary cPR. For patients who underwent hormone therapy, approximately 6.5 % achieved axillary cPR (P = .29). A significantly higher axillary cPR rate was identified in patients with clinical stage II disease at diagnosis (14/70 patients [20%]) compared with those having stage III disease (10/128 patients [7.8%]; P = .013). Patients with axillary cPR had fewer lymph nodes removed at the time of surgery compared with those having no cPR (8 vs 16 lymph nodes; P = .001).
Conclusions
An axillary cPR in patients with HR+/HER2–, clinically node-positive breast cancer was higher in those with a lower clinical stage (stage II). Patients with a cPR were able to avoid an axillary dissection. A larger cohort of patients is necessary to define more possible predictors of axillary response rate to neoadjuvant therapy.
