60 Racial Disparities in Hospitalization Outcomes Among Women With Metastatic Breast Cancer in the United States by Palliative Care Utilization
Background
While studies have reported that members of racial and minority populations hospitalized with metastatic breast cancer (MBC) have lower palliative care use than non-Hispanic White women, disparities in hospital-associated outcomes among inpatients have not been explored in this population. We examined the racial disparities in hospitalization outcomes among adult women with a diagnosis of MBC, stratified by receipt of palliative care.
Methods
Retrospective cohort analyses were conducted using the Agency for Healthcare Research and Quality (AHRQ)–sponsored Healthcare Cost and Utilization Project, National Inpatient Sample (HCUP–NIS) database from 2016 to 2020. Multivariable logistic and linear regression models were used to examine the association between race/ethnicity and in-hospital mortality, length of stay, and total hospital charges. Multinomial logistic regression models were used to evaluate the association between race/ethnicity and discharge disposition. Stratified analyses were conducted by palliative care use. Results were reported as adjusted odds ratios (AOR).
Results
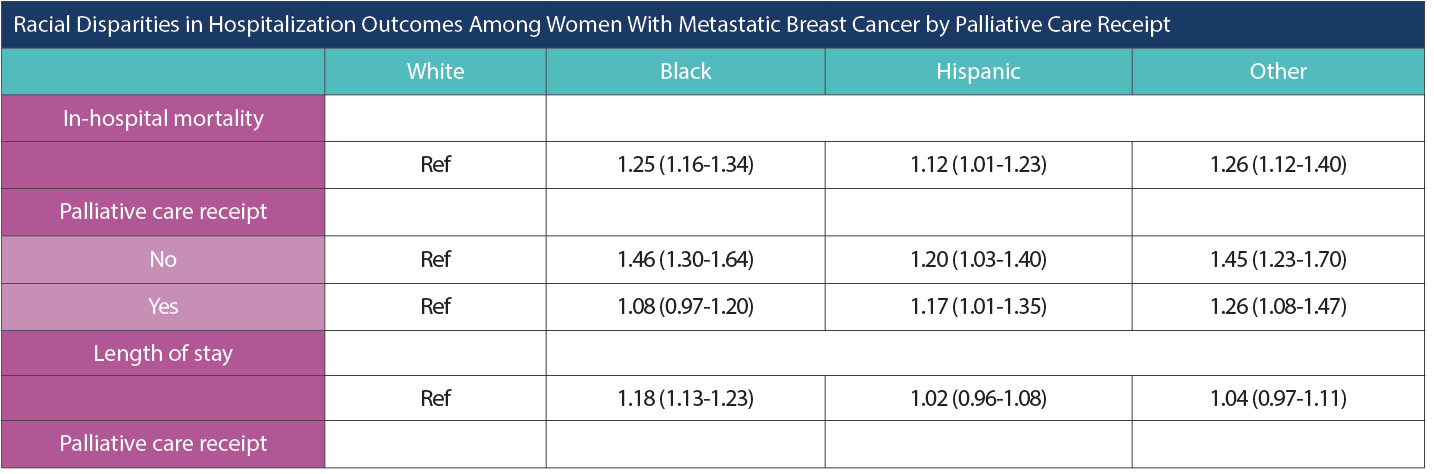
Racial Disparities in Hospitalization Outcomes Among Women With Metastatic Breast Cancer by Palliative Care Receipt
Racial Disparities in Hospitalization Outcomes Among Women With Metastatic Breast Cancer by Palliative Care Receipt (cont.)
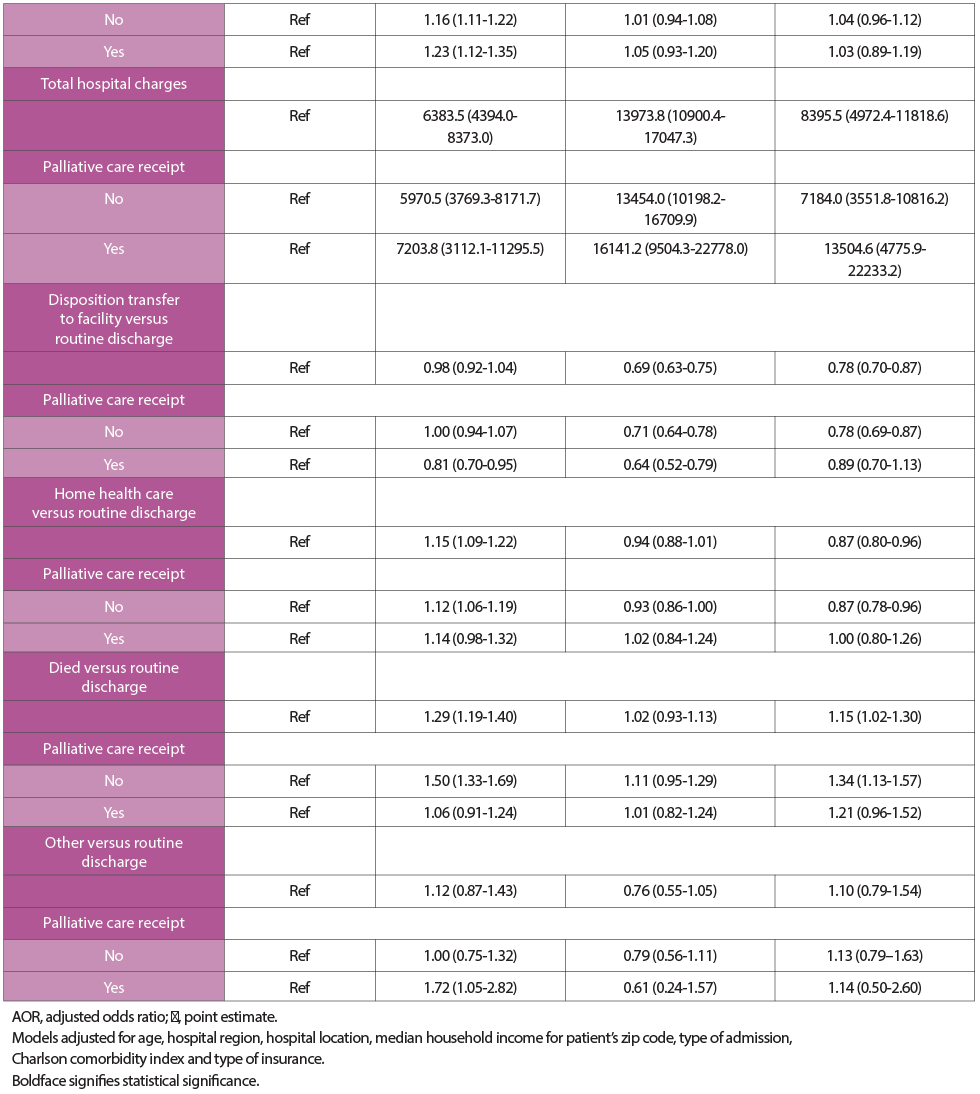
In the adjusted analyses, Black (AOR, 1.25; 95% CI, 1.16-1.34), Hispanic (AOR, 1.12; 95% CI, 1.01-1.23), and other (AOR, 1.26; 95% CI, 1.12-1.40) MBC patients had higher in-hospital mortality compared to the White patients. After stratifying by palliative care use, Black women who received palliative care had similar odds (AOR, 1.08; 95% CI, 0.97-1.20) of in-hospital mortality while those without palliative care use had 46% higher odds (95% CI, 1.30-1.64) of mortality when compared to White women. Black women were more likely (AOR, 1.18; 95% CI, 1.13-1.23) to have a length of stay greater than 5 days compared to 5 days or less relative to White women. Furthermore, Black, Hispanic, and other women had higher total hospital charges when compared with patients who are White. While women who were Black had similar odds (AOR, 0.98; 95% CI, 0.92-1.04) of being discharged to a short-term/skilled nursing facility vs routine discharge compared with women who were White, women who were Black who received palliative care had 19% (95% CI, 0.70-0.95) lower odds of being discharged to a facility. Hispanic and other MBC patients were less likely to be discharged to a facility relative to routine discharge when compared with women who were White.
Conclusions
Despite the improvement in palliative care use over the years, members of racial minority populations continue to have poorer outcomes. However, patients who are Black with MBC who received palliative care had similar in-hospital mortality and were less likely to be discharged to a facility when compared with their White counterparts. Our findings emphasize the importance of palliative care use among MBC patients and highlight the need to continue to raise awareness of its benefits, especially in minority populations. Further studies are needed to explore ways to narrow the gap in existing disparities and to test these interventions on care metrics and patient outcomes.
