66 A Comparative Analysis of Changes in Treatment Recommendation for Black and White Patients With Ductal Carcinoma In Situ Using a 7-Gene Predictive Biosignature: Analysis of the PREDICT Study
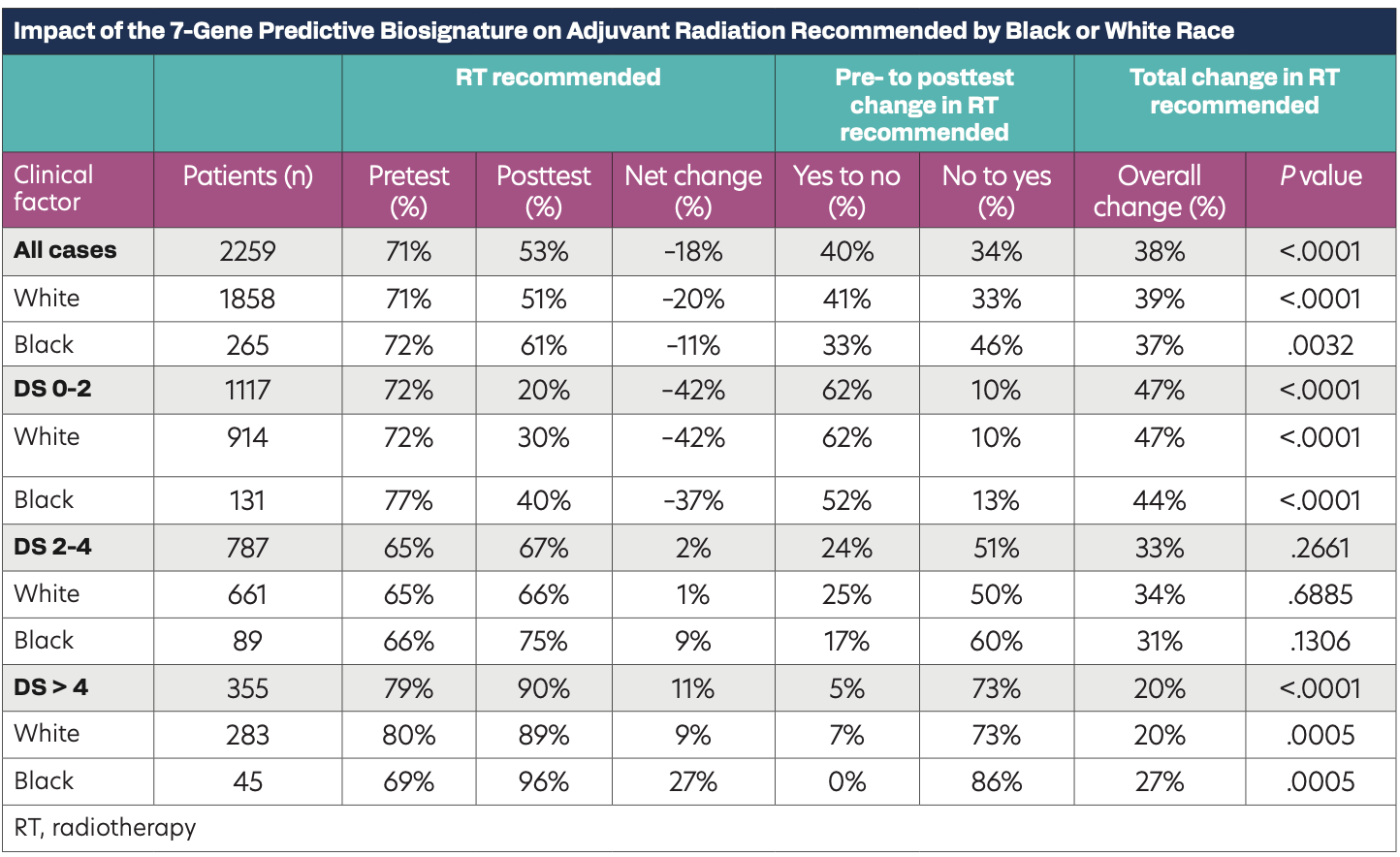
Impact of the 7-Gene Predictive Biosignature on Adjuvant Radiation Recommended by Black or White Race
Background
Previous studies have demonstrated that compared with White women, Black women are more likely to have second tumors (invasive and noninvasive) in either breast or die of invasive breast cancer (IBC) after ductal carcinoma in situ (DCIS). Although multiple studies have presented results on the treatment of IBC, there are very few studies examining the impact of race/ethnicity on the treatment of DCIS. Thus, there is a need to further determine whether biologic or clinicopathologic factors are associated with the recommendation of therapy for DCIS in patients from different races/ethnicities. In this study, we evaluated the decision impact for radiotherapy (RT) recommendations incorporating the 7-gene predictive biosignature by race (White vs Black) in women with DCIS enrolled in the PREDICT study.
Methods
The PREDICT study was a prospective, multi-institutional registry for patients who received DCISionRT testing as part of their routine care. The registry included females, age 26 and older, who were diagnosed with DCIS and were candidates for BCS and eligible for adjuvant RT or systemic therapy. Treating physicians completed treatment recommendation forms before and after receiving test reports to capture surgical, radiation, and endocrine therapy treatment recommendations and patient preferences. The primary end point was to identify the proportion of patients in whom testing led to a change in RT recommendation. Additional analyses included changes in recommendations in patient subgroups based on race/ethnicity. Changes in RT recommendation were analyzed by McNemar test.
Results
Analysis was performed in 2305 patients treated at 63 clinical sites. Overall, 81% of the patients were White and 11% of patients were Black. No significant differences were observed in the distribution of Black and White in clinicopathological factors where the median age was 63 in White patients and 62 in Black pateints, with 34% of Whites and 28% of Blacks having nuclear grade 3. Overall, RT recommendations were changed significantly in 39% and 37% of White (P <.0001) and Black patients (P = .0032), respectively. Pretest the rates of RT recommendation were not different between the Black and White patients (P = .8). Posttesting, there was a significant difference in the net change of RT recommendation in Black (P = .01) and White (P <.001) patients, where Black patients had a 10% higher rate of RT recommendation when compared with White patients (P = .004). Furthermore, 33% of the Black women and 41% of White women who were recommended to receive RT pretesting were not recommended to receive RT post-testing (P = .10). In addition, 46% of Black women who were initially not recommended to receive RT pretesting were recommended to receive RT posttesting in contrast to 33% of White women (P = .04). In contrast, there were no significant differences observed in proportion in the DS groups 0-2, 2-4, and > 4 by Black vs White (P = .7).
Conclusions
This analysis demonstrates significant changes in recommendations to add or omit RT based on the 7-gene predictive biosignature in 2305 patients. Black patients had significantly higher rates of RT recommendation compared with White women with similar biosignature scores, suggesting that clinicians may be influenced by prior reports of greater risk in the Black population.
