Addressing Psychological Challenges After Cancer: A Guide for Clinical Practice
The person diagnosed with cancer typically is confronted with a variety of difficult challenges. Treatment for cancer can be physically arduous, it generally disrupts patients’ social and work life, and it may even limit their ability to care for themselves or live independently for some period of time. In addition to these physical and functional burdens, cancer patients often face fears of death or disability, and may be prone to feelings of isolation or depression.
The person diagnosed with cancer typically is confronted with a variety of difficult challenges. Treatment for cancer can be physically arduous, it generally disrupts patients’ social and work life, and it may even limit their ability to care for themselves or live independently for some period of time. In addition to these physical and functional burdens, cancer patients often face fears of death or disability, and may be prone to feelings of isolation or depression.
Not surprisingly, many patients show signs of depressed mood or acute stress reactions at some point during their diagnosis and treatment.[1,2] Given the physical, economic, and psychological burdens experienced by cancer patients during treatment, it is perhaps a testament to human resilience and the quality of care and social support that patients receive that most adapt to these challenges and have a positive psychological outcome. Studies of long-term cancer survivors indicate that the majority do not suffer from significant psychological distress, though they may be at higher risk for depression than people never affected by cancer.[1]
While most long-term survivors will not have significant psychological distress related to their cancer, there is a sizable minority of cancer survivors who will. This article focuses on understanding the psychological challenges cancer survivors may face, and how nurses and other medical providers can recognize and respond to these issues. With more than 12 million cancer survivors in the US,[3] the enormous variety of survivor experiences and associated psychological issues must be acknowledged.
The “cancer survivors” we write about may have been treated for dozens of different types of cancer, at many different points in their lives, and with any of hundreds of different treatments. After completion of therapy they may be left healthy and disease-free, or with any of a variety of ongoing medical issues. Here we will address the most common psychological challenges cancer survivors face following completion of active therapy. We choose this focus not because other issues or phases of care are less important, but because patients who have completed active treatment have fewer visits with their medical providers, making it more difficult for providers to monitor psychological adjustment even as new issues of “life after cancer” emerge. After considering how psychological challenges may emerge following cancer treatment, we briefly discuss anxiety, depression, fatigue, and sexual function. Finally, we review methods for addressing these issues in the context of a medical visit and provide information on appropriate follow-up resources.
Psychological Complications After Cancer
Psychological challenges are part of life. As Erikson wisely demonstrated in tracing the “crises of development” from infancy to adulthood, the specific challenges change and change us as individuals, but they are ongoing as long as we are.[4] Challenges provide opportunities for reworking past unresolved issues as well as the risk that an unresolved challenge may end in maladaptation. Cancer, though not an expected challenge, may similarly result in psychological growth as well as maladjustment. Understanding why some survivors develop ongoing emotional problems while others do not is important in identifying survivors in need of additional support and treatment. Generalizing across cancers can be difficult, but research and clinical experience suggest that several factors may predispose a cancer survivor to ongoing psychological problems[1,2] (also see Table 1). Perhaps most important are health and functional status after completion of treatment. Physical and mental health are typically strongly associated, and survivors who have chronic conditions (eg, heart disease, diabetes), and especially those with multiple chronic conditions or chronic pain, may be particularly vulnerable to problems in psychological adaptation. Similarly, those who cannot return to work or are limited in their ability to care for themselves independently may be at risk.
The list of psychological challenges potentially facing cancer survivors is extensive, but among the most common are fatigue, depression, anxiety, and sexual problems. As with all patients, emotional concerns or sexual difficulties should be evaluated in the context of any medical conditions or medications that may be contributing to the development of symptoms. This is particularly important in working with cancer survivors because cancer treatments may have medical late effects on pulmonary, cardiac, hormonal, and other physiological systems that can contribute to a variety of psychological symptoms.[5,6] Similarly, many commonly prescribed medications may cause psychological symptoms or interfere with sexual functioning.
Common Psychological Challenges Experienced by Survivors
Fatigue
One of the most commonly reported effects that persist after cancer treatment is fatigue.[7] This fatigue is characterized by the subjective feeling of tiredness and anergia that does not subside with rest, and may be severe enough to impair life functioning.[5] As many as 34% of breast cancer survivors report fatigue even many years after the end of treatment.[7]
Answering Survivors’ Questions About Mental Health Services
Why would I need a Mental Health Professional?
Many people who experience problems in their lives seek a mental health professional for some kind of therapy or counseling. They may look for treatment of a specific symptom such as panic attacks, or they may want to learn a new way to manage problems in a relationship or at work. Cancer survivors may look for a mental health provider for these same reasons, as well as for issues related to their cancer.
What can I expect if I see a Mental Health Professional?
There are several kinds of mental health providers and many kinds of treatments. Your experience will depend on the provider you see and the problem for which you want help. You can expect the provider to listen to your experiences and ask questions about your personal history. You will need to talk about your difficulties and your goals for treatment. Most therapists see patients once a week for 45–50 minutes. Some types of therapy will last only a few sessions, while other therapy may continue for months or longer.
Finding the right Mental Health Professional
1. Mental health services can be expensive, often $90–$200 a visit, so most people use insurance to help pay for therapy. Contact your insurance provider for information about mental health services. Find out:
• What services are covered, if you have a co-pay, and how many sessions are covered.
• If you can use your insurance with any mental health provider, or instead need to see a provider who is part of the insurance network.
• If the insurance plan has a list of providers in your area. Some insurers will fax you a list or let you search a web site of affiliated providers.
2. Talk with your primary care provider (PCP) about your concerns and ask about mental health professionals in your area. If your insurer provides a list, ask if your PCP recommends any of the listed professionals. You may want to ask your PCP about possible medical causes of your current symptoms.
3. You may get helpful recommendations from trusted sources in your community. Friends and family, clergy, and
local hospitals or community centers may be able to recommend a mental health professional.
4. When you find the names of two or three providers, contact them by telephone. When you call:
• You will typically need to leave a message and ask the provider to return your call.
• Tell them about your concerns and ask about their experience helping people with similar issues.
• Ask about availability, fees, insurance, and if they are licensed. You may want to ask about their education, expertise, and years in practice.
• If you are satisfied with the answers, make an appointment.
5. During your first visit, plan to describe the reasons that led you to seek help. The provider may ask you detailed questions about your personal and medical history. Ask the provider what kind of treatment s/he recommends, and what other kinds of treatment might be available. Ask about expected benefits, length of treatment, and any side effects you might expect.
6. It is important to find someone with whom you have rapport, and feel you can trust. It may take a few visits to be sure you have a good “fit” with the provider and for him/her to get to know you. Talk to the provider about your questions or concerns. If you don’t feel you have a good fit with the provider talk to her/him about that, too.
Be honest-it is your treatment and the provider’s job is to help you. The provider may be able to change the approach to your therapy, or help you find a therapist who is a better match for you. Recontact your insurer or PCP if you need further assistance.
Fatigue may be particularly likely in survivors who are younger; have lower income; and experience pain, menopausal symptoms, and certain medical conditions such as arthritis and high blood pressure.[8] Reduced levels of physical activity during cancer treatment may be one source of fatigue after treatment completion, and chemotherapy treatments have been associated with lingering fatigue.[5]
Types of Mental Health Providers
Clinical Social Workers have a master’s degree (MSW) in social work and are trained to make diagnoses and provide therapy.
Clinical Psychologists have a doctoral degree (PhD) in psychology and are trained to make diagnoses and provide psychological testing and therapy.
Psychiatrists are medical doctors (MD) who have specialized training in mental illness and treatment. Psychiatrists can prescribe medications, and may also provide therapy.
Psychiatric Nurse Specialists are nurses with a master’s degree in mental health nursing who may prescribe medications as well as provide therapy.
Certified Alcohol and Drug Abuse Counselors are counselors with a variety of educational backgrounds who have specialized training in substance abuse.
Types of Treatment
Medication can be used to treat emotional disorders and symptoms of distress. Treatment usually involves identifying some target symptoms and trying a medication to improve them. Some medications take several days or even weeks to take effect, and the provider may need to see you several times to adjust the medication. Medication is often combined with psychotherapy.
Psychotherapy involves talking face-to-face with a therapist to help understand and resolve problems. The following are the most common types of psychotherapy available:
Behavior therapy focuses on trying to change patterns of problem behavior. Treatment often includes keeping records of problems or symptoms, learning new behaviors, and learning relaxation and stress management.
Behavior therapy may be used with cognitive therapy.
Cognitive therapy focuses on identifying thought patterns that lead to troublesome feelings and behaviors.
Treatment often involves recording problematic thoughts, and developing new thought patterns.
Psychodynamic therapy focuses on understanding how past experiences influence present behaviors and feelings. Treatment involves talking about problems in detail to better understand the motivations and emotions involved, and to develop better ways of expressing those feelings.
Family or couples therapy involves treating the couple or family to help resolve problems that arise in family relationships. The therapy often involves family members discussing problems together to develop better communication, and identify problem interactions.
Group therapy brings together individuals with similar problems to work together for change. Treatment often includes group members discussing their problems and getting feedback and support from each other.
Recent neuroscience research indicates that lingering fatigue also could be the result of a “long-term alteration in inflammatory biology” that may arise as a consequence of chemotherapy and radiation treatment.[9]
In assessing the survivor with fatigue it is important to differentiate between fatigue and depression. This can be difficult given that lack of energy often can be a sign of depression. However, it has been found that depression alone does not entirely explain feelings of fatigue in survivors.[8] Addressing physical conditions, medication effects, and depression will improve fatigue symptoms in many survivors.
For those whose fatigue persists after these causes are addressed, treatment may include a combination of efforts to manage fatigue (activity and rest scheduling) and to build endurance. Regularly scheduled exercise training has been proven to target aerobic capacity and muscle strength that might be compromised by cancer treatment.[5,10] Psychoeducational interventions have also proven to be beneficial for survivors, and pharmacologic treatments with psychostimulants show some promise for the future treatment of cancer-related fatigue.[11]
Depression
Talking with survivors about depression can be complicated, because the very word “depression” can describe a normal variation in mood, a more lasting and troubling mood state, or a psychiatric disorder characterized by mood disturbance and other associated symptoms. It is important to acknowledge to survivors that everyone experiences normal variation in mood but that the focus of assessment is to look for mood changes that are lasting, cause distress or impaired functioning, or are associated with other symptoms like poor sleep, or feelings of hopelessness.
When depressed mood lasts more than 2 weeks and is associated with impaired functioning and other symptoms, it may be a sign of a psychiatric condition known as major depressive episode. In the general population the lifetime risk for Major Depressive Disorder varies from 10% to 25% in women and from 5% to 12% in men,[12,13] making it likely that a number of cancer survivors would be expected to suffer from depression. Risk factors for depression in cancer survivors may include younger age, poor social functioning, prior depression, and significant pain.[14,15]
A referral to a mental health professional for evaluation and treatment should be recommended for survivors with depression symptoms that are not transient or are associated with significant subjective distress, impairment in function, or somatic symptoms not explained by a medical condition.[15] The majority of survivors reporting depressed mood are likely to report transient symptoms, or symptoms not associated with significant impairment in their work, home, or social functioning.
For these survivors, educational and support group interventions should be beneficial,[15] and even for survivors with depression requiring psychiatric treatment, survivor-oriented support programs can be a very useful adjunct. For survivors presenting with even mild symptoms of depression it may be prudent to refer them to a primary care provider for a more thorough evaluation.
A psychiatric diagnosis of depression can be characterized by the presence of somatic symptoms (eg, fatigue, sleep disturbance), making this differential diagnosis particularly challenging.[14]
Anxiety
Similar to depression, anxiety should be understood as existing along a continuum from expected mild responses to life circumstances, to symptoms that can be a source of ongoing distress, and psychiatric conditions defined by a specific constellation of enduring symptoms that impair functioning. Certain periods in the survivorship trajectory, such as the end of treatment and follow-up visits, are particularly stressful.[16] Anxiety symptoms are not rare, with close to 30% lifetime prevalence of any anxiety disorder in the general population.[13]
Several survivor characteristics have been associated with anxiety symptoms, including younger age, economic difficulties, lack of social support, alcoholism, and premorbid psychiatric conditions.[17] Because medical visits can be a source of anxiety, it is important that providers distinguish between anxiety related to a follow-up visit versus anxiety that is more lasting and potentially impairing a survivor’s ability to function. It is also important to note both the quality and the intensity of the anxiety experienced by the survivor.
All individuals experience some symptoms of general anxiety or worry, usually in the form of fear or anticipation of some negative situation. In individuals with significant worry, this can be associated with feelings of agitation and can be a source of subjective discomfort and impaired functioning. For cancer survivors, recurrence or other medical worries can be a source of significant worry. Mild symptoms of worry, especially health-related worry, may be addressed with referral to education resources, support groups, or survivor-specific support resources.
Some individuals will experience periodic uncomfortable reminders of their cancer or its treatment, such as intrusive thoughts, memories, or nightmares suggesting post-traumatic stress disorder. This diagnosis requires the presence of a trauma, which triggers a response of fear, helplessness, or horror. Symptoms stemming from the trauma and horror are the re-experiencing of the event, avoidance of situations that are reminders of the trauma, and physiological hyperarousal. While most survivors with these symptoms will not meet psychiatric diagnostic criteria for post-traumatic stress disorder,[1] these symptoms can be disconcerting and uncomfortable.
Individuals with mild symptoms of post-traumatic stress may benefit from educational and supportive services, but providers may want to refer survivors with any of these symptoms to mental health providers for more specialized assessment and treatment. Survivors with more significant distress or impairment associated with anxiety, as well as those with panic attacks, should be referred to a mental health professional. Panic attacks are a distinct type of anxiety characterized by a sudden intense “attack” of several physical symptoms such as shortness of breath, tachycardia, and sweating palms.
Panic attacks are frequently mistaken for signs of medical illness and these individuals may make several emergency department visits before being properly diagnosed. Panic attacks can be successfully treated with cognitive-behavior therapy or medication.
Sexuality
A common challenge after cancer is the impact of cancer treatment on sexual functioning.[18] A majority of cancer survivors, of all ages, are sexually active soon after cancer treatment ends.[19] Sexual functioning is a crucial quality-of-life issue for survivors, and they may be unprepared for sexual problems because treatment consequences to sexuality may be minimized or not fully addressed in communication with the patient during routine oncology care.[20] The sexual difficulties experienced by survivors vary depending on gender and treatments received.
Common sexual problems after cancer treatment include low desire, changes in body image and self-esteem, pain during sex, and decreased physical responsiveness. In addition, loss of body integrity, scars, and surgical reconstructions can all have a profound effect on how survivors feel about their bodies and how they experience physical pleasure. Treatment with pelvic radiation as well as hormonal therapies such as use of aromatase inhibitors for women after breast cancer or antiandrogen therapies for men with prostate cancer, for example, can have a significant negative impact on sexual functioning and desire.
For women, a primary concern is premature menopause caused by any cancer treatment that disrupts ovarian functioning. The symptoms of an abrupt treatment-induced menopause are often dramatic and can lead to severe vaginal dryness, painful intercourse, decreased arousal, and reduced desire. Erectile dysfunction (ED) is the most common sexual problem for men after cancer treatment. Men who are treated for prostate, bladder, or rectal cancer are at significant risk for ED. Although techniques have been pioneered to try to spare nerves that control blood flow to the penis, the rates of ED after radical prostatectomy remain high.[18]
Almost all survivors with sexual functioning difficulties will benefit from information and support resources, as well as reassurance that sexual problems are often related to very treatable problems. For example, for women, optimal use of appropriate lubricants and bioadhesive gels can make an enormous impact on vaginal dryness, tissue atrophy, and sexual functioning.
For men with ED, a variety of treatments such as penile injections, vacuum devices, and prosthetics, as well as PDE5 inhibitor drugs such as Viagra (sildenafil citrate) may be effective, and affected men should be made aware of these options.
Start the Conversation: Talking With Survivors About Their Psychological Challenges
Ganga Stone entitled her book advocating open discussion of death and dying “Start the Conversation,”[21] and these three words may also be the best advice for providers talking with cancer survivors about their psychological well being. Research shows that cancer patients are interested in talking about psychosocial issues, but they typically wait for providers to “start the conversation.”[1] Finding time for this discussion during a busy medical visit can be a challenge.

The simplest approach to a conversation may include a self-report assessment addressing emotional health, economic, social, and functional status, completed by survivors at the time of their office visit. Self-report assessment has the advantage of being simple to incorporate into each visit. It also ensures that these topics are addressed, and “primes” survivors to think about and discuss these issues with their providers. Whatever formal assessment is used, follow-up, including reviewing these responses and discussing them directly with the survivor, is essential. A brief guide to discussing these issues is presented in Table 2.
Frank discussion of sexual and emotional health after cancer is often uncomfortable for clinicians and patients. Typically, however, it is an enormous relief to patients when they are asked about these important aspects of their functioning. One useful framework for guiding discussion with cancer patients and survivors is that of self-determination theory (SDT).
Inherent to this perspective is the principle that individuals have an innate tendency toward competence, autonomy, and relatedness, all elements that can be facilitated in a social context. In particular, the experience of autonomy support (ie, helping individuals see how they can exercise choice regarding their behavior) is related to greater persistence of behavior change and improved psychological and physical health.[22]
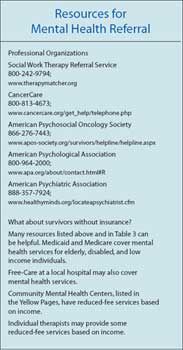
Follow-up Resources for Survivors With Psychological Concerns
The benefit of assessing cancer survivors for psychological concerns is realized only if arrangements are made for appropriate follow-up care. Unfortunately, arranging these services can be time-consuming and complicated as survivors’ needs will vary, and many resources may not be easy to identify or access. In hospitals or cancer centers, resource specialists or social workers may be available to help assess survivors’ needs and identify appropriate referral resources. Teaching sheets about medical conditions and coping with cancer therapies are often available, and many of these will be appropriate for survivors.
In some settings a staff social worker or psychologist may be available to consult with the medical team, make referral recommendations, or even see survivors for individual assessment. More commonly, nurses and other providers in general medical and oncology settings will be called upon to offer referral resources to survivors in their practice. Information about support groups as well as internet and telephone-based support services is available in a 2007 report by the Institute of Medicine (IOM) on psychosocial needs of cancer patients,[23] and these resources can be supplemented with local listings. For mental health concerns, additional resources may need to be developed, including educational materials and contact information for advocacy organizations, support groups, and local mental health professionals. Educational materials about conditions like anxiety and depression are available from the National of Institute of Mental Health.[24]
Survivors benefit most when referrals match their interests and they feel personally invested in pursuing them. Some survivors may be reticent to accept follow-up recommendations, and it is important to give individuals a sense of what is being offered and why it is being recommended. Providers who expect survivors to make significant changes after a brief conversation will tend to be frustrated and ineffective, as changes in behavior (exercising more, joining a support group) are the result of processes of change.[25]
Providers should aim to increase the likelihood of these changes happening over time, rather than trying to get them quickly adopted. It is appropriate for providers to indicate to the survivor that a symptom or concern requires some particular kind of follow-up treatment, but it is also important that the provider recognizes and respects the survivor’s wishes.
Reluctant survivors who are unsure whether they really need a referral may sometimes agree to revisit the issue in a follow-up appointment, or even to discuss the issue after several weeks’ time in a follow-up conversation by telephone. One strategy can be to ask survivors how long they think they should wait before initiating some follow-up for a particular problem, and then arrange for follow-up contact at that time. Some survivors will need to have the same recommendation made on several occasions or from several sources before being comfortable initiating follow-up.
The nature and severity of the survivor’s symptoms or concerns will determine what follow-up resources are appropriate. Table 3 gives examples of the kinds of resources that may be useful for different psychosocial challenges facing survivors. Specific resources and organizations are included only as examples, and readers looking for a detailed list of services and organizations should refer to the IOM report.[23] Need for information about medical conditions or symptoms may be addressed with teaching sheets, or referral to internet-based resources.
For emotional or psychological issues, some educational resources also may be useful, but counseling or support groups are more likely to be recommended. Most survivors who acknowledge feelings of anxiety and depression, for example, will not have a psychiatric diagnosis, but rather have a small number of mild symptoms which do not interfere with their functioning and are not a source of significant subjective distress.
For these individuals, educational materials about their medical and emotional symptoms may be helpful in raising their awareness and decreasing feelings of stigma. A support group for cancer survivors, for relevant chronic conditions or for emotional issues, also may be appropriate. Support groups or some survivor counseling may be available through the internet or by telephone, through groups such as CancerCare or the Lance Armstrong Foundation.
Some individuals already seeing a mental health professional may seek out support groups or condition-specific resources as an addition to their mental health treatment. Referral to a mental health provider will be important for individuals who have any kind of complicated presentation requiring more extensive evaluation, as well as anyone whose symptoms are associated with more than mild distress, or limitations in their ability to function (ie, associated with problems in work, social function, or self-care). Barriers to obtaining mental health services are well known to most practitioners, and survivors seeking mental health treatment may face numerous obstacles.
Patients seen in specialty medical clinics may need to be referred back to their primary care practitioners for assistance with a mental health referral, or for psychopharmacological treatments available from a primary care provider. We have developed a mental health referral information sheet specifically to educate cancer survivors about mental health services and assist them in finding appropriate referrals. (Excerpts have been reproduced in sidebars of this article. Copies are available at http://cancernetwork.com/Recklitis- Mental-Health-Teaching-Sheet.pdf and may be freely used and adapted without permission.)
This article is reviewed here:
The Recklitis et al Article Reviewed
References:
References
1. Stanton AL: Psychosocial concerns and interventions for cancer survivors. J Clin Oncol 24:5132â5137, 2006.
2. Kornblith AB: Psychosocial adaptation of cancer survivors, in Holland JC (ed): Psycho-Oncology. New York, NY, Oxford University Press, 1998, pp 223â254.
3. National Cancer Institute: The nation’s investment in cancer research, in Connecting the cancer community: An annual plan and budget proposal for FY2009. National Institutes of Health, US Department of Health and Human Services, 2008.
4. Erikson EH: Identity: Youth and Crisis. New York, NY, W.W. Norton and Company, Inc, 1968.
5. van Weert E, Hoekstra-Weebers J, Otter R, et al: Cancer-related fatigue: Predictors and effects of rehabilitation. Oncologist 11:184â196, 2006.
6. Sadock BJ, Sadock VA: Kaplan and Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (Synopsis of Psychiatry). 10th ed, Philadelphia, PA, Lippincott Williams & Wilkins, 2007.
7. Bower JE, Ganz PA, Desmond KA, et al: Fatigue in long-term breast carcinoma survivors: A longitudinal investigation. Cancer 106:751â758, 2006.
8. Bower JE, Ganz PA, Desmond KA, et al: Fatigue in breast cancer survivors: Occurrence, correlates, and impact on quality of life. J Clin Oncol 18:743â753, 2000.
9. Collado-Hidalgo A, Bower JE, Ganz PA, et al: Inflammatory biomarkers for persistent fatigue in breast cancer survivors. Clin Cancer Res 12:2759â2766, 2006.
10. Pinto BM, Maruyama NC: Exercise in the rehabilitation of breast cancer survivors. Psychooncology 8:191â206, 1999.
11. Bower JE: Fatigue in cancer patients and survivors: Mechanisms and treatment. Psychiatry Weekly, 2008. Available at:
www.psychweekly.com/aspx/article/ArticleDetail.aspx?articleid=60
12. American Psychological Association: Diagnostic and Statistical Manual of Mental Disorders. 4th ed (text revision), Washington, DC, American Psychiatric Association, 2000.
13. Harvard School of Medicine: The National Comorbidity Survey (NCS) and the National Comorbidity Survey Replication (NCS-R), 2005.
14. Deshields T, Tibbs T, Fan MY, et al: Differences in patterns of depression after treatment for breast cancer. Psychooncology 15:398â406, 2006.
15. Bower JE: Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol 26:768â777, 2008.
16. Knobf MT: Psychosocial responses in breast cancer survivors. Semin Oncol Nurs 23:71â83, 2007.
17. Dahl AA, Haaland CF, Mykletun A, et al: Study of anxiety disorder and depression in long-term survivors of testicular cancer. J Clin Oncol 23:2389â2395, 2005.
18. Schover LR: Sexuality and fertility after cancer. Hematology Am Soc Hematol Educ Program 523â527, 2005.
19. Ganz PA, Desmond KA, Leedham B, et al: Quality of life in long-term, disease-free survivors of breast cancer: A follow-up study. J Natl Cancer Inst 94:39â49, 2002.
20. Gallo-Silver L: The sexual rehabilitation of persons with cancer. Cancer Practice 8:10â15, 2000.
21. Stone G: Start the Conversation: The Book about Death You Were Hoping to Find. New York, NY, Warner Books, Inc, 1996.
22. Deci EL, Ryan RM: The support of autonomy and the control of behavior. J Personality Social Psychol 53:1024â1037, 1987.
23. Institute of Medicine: Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC, The National Academies Press, 2007.
24. National Institute of Mental Health: Mental Health Topics, 2008. Available at:
www:nimh.nih.gov/health/topics/index.shtml
.
25. Prochaska JO, DiClemente CC: Stages of Change in the Modification of Problem Behaviors. Newbury Park, CA, Sage Publishing, 1992.