Advising Women at High Risk of Breast Cancer
Women with any family history of breast cancer assume a high probabilityof risk. Counseling women involves ascertainment of an accuratefamily history and use of the best predictive models to assess boththe risk of a known mutation and the risk of breast cancer. This riskmust then be considered in the contexts of both the woman’s lifetimeand the next decade, in each instance carefully separating the risk ofdeveloping cancer from the risk of mortality. These two risks are oftenemotionally melded in women who have watched a loved one die ofcancer. The options for a woman at significantly increased risk of breastcancer include optimal surveillance, chemoprevention, and prophylacticsurgery. This entire field is in continuing evolution as better methodsof diagnosis, screening, and chemoprevention continue to enter clinicalpractice.
ABSTRACT: Women with any family history of breast cancer assume a high probability of risk. Counseling women involves ascertainment of an accurate family history and use of the best predictive models to assess both the risk of a known mutation and the risk of breast cancer. This risk must then be considered in the contexts of both the woman’s lifetime and the next decade, in each instance carefully separating the risk of developing cancer from the risk of mortality. These two risks are often emotionally melded in women who have watched a loved one die of cancer. The options for a woman at significantly increased risk of breast cancer include optimal surveillance, chemoprevention, and prophylactic surgery. This entire field is in continuing evolution as better methods of diagnosis, screening, and chemoprevention continue to enter clinical practice.
Awareness of inherited predilections for the development of breast cancer has been coupled with an information explosion in the lay literature about the subject of breast cancer screening techniques and methods of therapy, creating an anxious public. In the last decade, BRCA1 and BRCA2 were identified as high-risk mutation genes in relationship to breast cancer. PTEN mutation associated with Cowden syndrome is also clearly related to a moderate risk for breast cancer. It was anticipated that a host of other genetic mutations related to high or moderate penetrance breast cancer association in families would follow. To date, no other dramatic breast cancer-related gene has been identified, despite many other families with an apparent pattern of dominant transmission (Table 1).[1]
TABLE 1
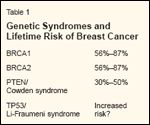
Genetic Syndromes and Lifetime Risk of Breast Cancer
Women with any family history of breast cancer assume a very high risk of developing the disease themselves. Counseling such women begins with a three-or four-generation family history. With a large family, such a history may be quite informative; with sparse families, it is less so. The Gail model has been validated as a reasonable instrument for assessing population risk, but it is of limited value in hereditary cancer families. The Claus model is more accurate in families at high risk but underestimates paternal transmission. Two models that are specifically directed toward the identification of high-risk families are available on the Internet from Myriad Genetics[ 2] and Johns Hopkins University (BRCAPRO).[3]
Three Patient Groups
In clinical consultation, three populations of women present with concerns about high risk of breast cancer. The first group are those who have had genetic testing and have been identified as expressing a mutated gene associated with high-penetrance breast cancer. Although we are unable to assign a risk specific to any individual, this population of women has a clearly defined risk of breast cancer development between 55% and 85% in the case of BRCA1 and BRCA2 mutation carriers, depending somewhat upon the specific mutation. These mutations are not only associated with high risk, they are associated with a much earlier risk of breast cancer than is seen in the sporadic pattern.
The second population comprises women who present with a strong family history suggestive of inheritable breast cancer but test negative for BRCA1 and BRCA2. They are clearly at increased risk, but it is impossible at present to quantitate the magnitude of this increase.
The third population are those who have a strong family history but have not been tested. This last group is of particular concern when they seek a major intervention (eg, prophylactic mastectomy). If a family member with early breast or ovarian cancer is alive and can be tested for the presence of a gene mutation, such testing should always be encouraged. Such a mutation has only a 50% likelihood of being inherited by the proband in consultation. Being able to identify which woman has not inherited the mutated gene and has only a normal population risk of breast cancer spares not only the possibility of prophylactic surgery but great anxiety, both at present and in the years to come.
Three Major Questions
Three major questions dominate a consultation with a woman who is not aware of having breast cancer but is concerned about her family history.
Optimal Surveillance?
The first question focuses on the best method of surveillance in order to detect breast cancer, should it arise, as early as possible. Several recent studies suggest that magnetic resonance imaging is better than screening mammography at the early detection of breast cancer in young women who are at high risk.[4,5] The concordance of these published trials gives more weight to this finding than the numbers or statistical strength of any of the studies, singly or additively.
Whether magnetic resonance imaging or, indeed, mammography should be performed more often than annually and at what age it should be initiated have not been clearly answered. The old recommendation of Dr. Henry Lynch that 10 years prior to the age at which a mother or sibling developed breast cancer is when to start radiographic screening appears prescient as anecdotal and series data continue to accumulate.
Clinical breast examination remains important, as many cancers in this sensitized population continue to be detected by patients themselves. Although it is not clear that earlier patient detection affects mortality, it may limit the mode and extent of therapy required for treatment.
A final important aspect of surveillance involves the immediate biopsy of suspicious lesions. This can be accomplished by fine-needle aspiration on the day that a lesion is first identified, rather than waiting a month or two to see if it is a physiologic abnormality that will regress spontaneously. The latter approach is to be decried in these women at increased risk. The role of real-time ultrasound in screening this high-risk population remains uncertain.
Although surveillance is very important in women at increased risk, its sensitivity clearly varies with the individual.[6] Whether breasts are soft, hard or nodular, radiolucent or mammographically dense, of average size vs very large or very small, and if the subject is compliant vs noncompliant with a regular screening program are all factors that clearly influence the efficacy of surveillance.
No prospective, well-defined surveillance program in a genetically defined population has clearly delineated the role of a specific screening protocol in this population. A series of small studies are under way, and interim reports are now appearing. Nevertheless, previous retrospective evaluations of surveillance outcome in "high-risk" women (variously defined) do raise alarm by showing that from 20% to more than 30% of the patients in such programs have lymph node involvement at the time of tumor detection.
Approaches to Prevention?
The second major question that arises is concerned with the prevention of breast cancer in women at high risk. Lifestyle changes have often been instituted by these women themselves. Some become vegetarians, others increase their athletic activities, and some adapt techniques alleged to diminish stress and tension. At present, there are no data to suggest that any of these approaches diminishes the risk of breast cancer or the rate of its progression.
Activity has been associated with a lower incidence of breast carcinoma in the general population, but only at the extremes. Women who have an extremely sedentary lifestyle and are overweight have an increased risk of breast cancer, and those who exercise- particularly to the point of ovarian suppression (eg, marathon runners)-have a diminished risk of breast cancer. Such data are not available in mutation-positive high-risk women.
The only dietary factor that appears repeatedly in cohort studies as a risk modifier is the use of alcohol. One glass of wine daily produces no demonstrable increased risk. Two glasses are associated with a 20% to 30% increase in baseline risk, and three or more glasses, with an increase of roughly 50%. Whether these increases apply to the population of genetically defined high-risk women is unproven.
• Hormonal Therapy-Tamoxifen has been shown to prevent contralateral breast cancer by roughly 50% when taken for 5 years.[7,8] The limited data available suggest that this is true in BRCA2 mutation carriers, but it is not clear that it is true in BRCA1 patients. This distinction has arisen because the majority of sporadically arising breast cancers are hormone receptor-positive, as are most BRCA2-related breast cancers. A minority of BRCA1 mutation breast cancers are hormone receptor-positive. The fact that oophorectomy for women with hereditary breast/ovarian syndrome (BRCA1/BRCA2) appears to prevent breast cancer in BRCA1 as well as BRCA2 mutation carriers suggests that more data are needed before tamoxifen can be considered ineffective in the BRCA1 population.
The current Study of Tamoxifen and Raloxifene (STAR) trial is comparing tamoxifen with raloxifene (Evista) to prevent breast cancer. European trials are evaluating the efficacy of aromatase inhibitors in this setting. Early data from the Arimidex, Tamoxifen Alone or in Combination (ATAC) trial suggesting that anastrozole (Arimidex) reduces the incidence of contralateral breast cancer even more effectively than does tamoxifen have been encouraging in this respect. The actual utility of these alternative agents outside of a clinical trial remains to be established.
• Oophorectomy-At least three reports of oophorectomy in BRCA1 and BRCA2 mutation carriers are associated with a reduction to half the rate of subsequent breast cancer development.[ 9,10] Although the numbers in these trials are small, the effect is consistent among them. This is particularly appealing prophylactic surgery because the risk of ovarian cancer causes such concern in women with BRCA1 or BRCA2 mutations.[11] Although the risk of ovarian cancer is lower than that of breast cancer, our ability to detect it at an early stage is almost nonexistent. The possibility of proteomic diagnosis in the near future would be a bright hope to that end.
Role of Prophylactic Mastectomy?
Many women worried about their risk for breast cancer, whether it is greatly increased or not, raise the topic of prophylactic mastectomy. There are three situations in which these women inquire about the procedure. The first involves women who are concerned about their risk of breast cancer but have not actually been diagnosed. The second scenario includes those who are facing mastectomy for the treatment of breast cancer or diffuse ductal carcinoma in situ and are concerned about the contralateral breast. (This is a separate topic, but the risk of contralateral cancer needs to be estimated using modern population-based, age-adjusted data.) The third situation involves women who are eligible for breastconserving therapy but, because they are at high risk, are considering the more extreme course of action instead. In discussing prophylactic mastectomy with the patient, several issues need to be addressed: (1) the individual risk of breast cancer, as carefully defined and quantitated as possible; (2) the effectiveness of surveillance in this particular woman; (3) her quality of life with surgical vs nonsurgical management, and (4) the availability of reconstructive options. There has been no randomized trial or even prospective study of a defined high-risk population with a defined prophylactic mastectomy and sufficient follow-up to fully assess the strengths and weaknesses of each approach.[12]
• Key Data-When we consider prophylactic mastectomy, there are several sources of information that influence our thinking. The first is the finding that in virtually all animal models of breast cancer development, removing the breast tissue will not eliminate the risk.[13-15] On the other hand, in clinical studies of reduction mammoplasty, although this procedure spares a significant amount of breast tissue, it is associated with a decreased lifetime risk of breast cancer compared with that seen in the sisters of the cohort undergoing reduction. In fact, the drop in risk associated with mammoplasty approaches 40%.[16]
Large series of subcutaneous mastectomy (nipple-sparing) procedures have been associated with only a few subsequent breast cancers. Unfortunately, the risk of the women undergoing these subcutaneous mastectomies was never defined in a way consistent with a contemporary understanding of risk. Dr. Lynn Hartman has reviewed Dr. John Wood's series of subcutaneous mastectomies at Mayo Clinic. She has contacted the women involved when possible and obtained a complete family history. Her analysis suggests that there is a greater than 90% prevention of subsequent breast cancer by such mastectomies.[17]
Schrag et al cast assumptions and created simple computer models of prophylactic mastectomy that have suggested the gains in life expectancy at standard population risk are less than 1 year, regardless of how early in life the procedure is performed.[18] At a 60% risk, roughly 4 years might be gained in life expectancy if prophylactic mastectomy is performed at age 30, as compared with 4 months if it is delayed until age 60. This general principle- the earlier the mastectomy is performed and the greater the risk of cancer, the greater the improvement in life expectancy-is defined in the model itself.
• Decisions and Goals-For the woman who elects prophylactic mastectomy, several decisions must be made, relating to the type of mastectomy and the method of reconstructive surgery. For women undergoing prophylactic mastectomy, immediate reconstruction is assumed but clearly not required. The assumption is based on the superior cosmetic result that can be obtained with mastectomy techniques that are coupled with immediate reconstruction.
The goal of prophylactic mastectomy is total removal of all breast tissue. In an absolute sense, that is never accomplished. One must settle for the removal of all apparent breast tissue, and even that is subject to various definitions. There is no less-pleased patient than a woman who has undergone prophylactic mastectomy and later develops breast cancer in grossly residual breast tissue. Although breast cancer arising in a woman at high risk after prophylactic mastectomy is a very uncommon occurrence, it is certainly not unheard of. I have personally never seen this happen in a patient without apparent residual breast tissue on physical examination when she was referred with breast cancer.
• Types of Mastectomy-Modified radical mastectomy is inappropriate in this setting, as there is no reason to perform an axillary dissection as part of prophylactic mastectomy. On the other hand, "total" mastectomy has replaced "simple" mastectomy as the defining term, largely to emphasize that the entire breast parenchyma is removed as completely as possible, including the axillary extension of breast tissue that is generally present.
Historically, total mastectomy entailed the simultaneous removal of a generous ellipse of skin, including the nipple and areola, sufficient that the closed flaps were held with the same tension as surrounding skin, for optimal cosmesis in the absence of reconstruction. When such women underwent breast reconstruction at a later time, it was virtually impossible to insert a new ellipse of skin that recreated the natural lilt of a woman's breast. The reconstructions performed in this staged manner tended to recreate an adolescent breast shape.
The initial immediate reconstructions were done with subcutaneous mastectomies. This operation spares the nipple and areola and sufficient underlying subareolar tissue to maintain the shape of the nipple-areola complex; it often failed to completely remove the axillary tail as well. This operation was commonly performed as a prophylactic mastectomy, together with immediate reconstruction by plastic surgeons. It has been shown that the procedure was actually quite effective in lowering the risk of subsequent breast cancer in women with variable degrees of high-risk genetic profiles.[19]
If these women later developed breast cancer, it usually arose in the subareolar tissue of the nipple. This led to general condemnation of this procedure by the surgical oncology community, which advocated total mastectomy. That recommendation was based on the judgment that a woman giving up her breasts to prevent breast cancer would be better served with the operation leaving the least residual risk.
• Three Specific Approaches-Today, three varieties of total mastectomy and immediate reconstruction are written about for women undergoing prophylactic mastectomy. The first and by far most commonly used procedure is skin-sparing mastectomy.[ 20] In this operation, the nippleareola complex and all breast tissue are removed via a circumareolar incision. The overlying skin envelope is spared, as is the inframammary fold. If the breast is generous and the nipple small, it may be necessary to extend the circumareolar incision laterally in a "racket handle" for a couple of centimeters in order to complete the procedure and remove the specimen. Preservation of the skin envelope makes possible a reconstruction that superbly mimics the natural breast.
One modification of the skin-sparing mastectomy is called a nipple-sparing mastectomy. This is actually the old subcutaneous mastectomy with a new name, the old name having been vilified. The third procedure that is often listed but rarely performed, and for which there are no mature followup data, is the areola-sparing mastectomy. This is a cross between the first two strategies, in which the nipple is removed with the specimen but the areola is spared. On first principles, it seems a perfectly reasonable approach, but definitive outcome data are lacking.
• Breast Reconstruction-After prophylactic mastectomy, the reconstructive technique is tailored to the individual. For a small-breasted woman, a tissue expander or prosthesis placed beneath the pectoralis major muscle may suffice. It is never a good idea to place prostheses immediately beneath the skin envelope, as they feel quite unnatural; placing them beneath a layer of muscle does a much better job of mimicking the sensation of a normal breast. For women whose breasts are larger, and who either have a flat abdomen or do not wish to have surgery involving their abdominal wall, transfer of a portion of the latissimus dorsi muscle to adjoin the pectoralis major muscle between the skin and an appropriate-sized prosthesis permits an excellent reconstruction.
For some women, particularly those who are quite large-breasted and who may be grateful for the opportunity to have a "tummy tuck" procedure, the familiar transverse rectus abdominis myocutaneous (TRAM) flap-either as a pedicle procedure or a free transfer-is a good choice. Pedicle TRAM or latissimus procedures are threatened in women who are actively smoking. The vasospasm causes a significantly increased risk of fat necrosis in the transferred tissue. Avoiding all tobacco and nicotinecontaining tobacco-substitution products for several weeks allows this procedure to be performed without increased risk.
Conclusions
REFERENCE GUIDE
Therapeutic Agents
Mentioned in This Article
Anastrozole (Arimidex)
Raloxifene (Evista)
Tamoxifen
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
Although prophylactic mastectomy can produce a very satisfactory aesthetic result if good technical surgery and reconstructive capabilities are available, its effects must not be trivialized. The procedure itself requires several hours of anesthesia and is usually accompanied by several weeks of fatigue during the recovery period. The loss of all nipple sensation and concern about body image combine to affect arousal and sexual function for many women in the postoperative period.
On the other hand, for women who face a heightened risk of breast cancer- especially those with a family history of death from breast cancer-the tradeoff seems worthwhile. Such women often express great satisfaction in having made this decision. When considerable time is spent exploring options and sharing information with the patient and her family prior to the procedure, the time required to adjust postoperatively may be greatly abbreviated.
In conclusion, prophylactic mastectomy greatly diminishes both the risk of breast cancer and the anxiety of death from breast cancer, while eliminating neither.
Financial Disclosure:The author has no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1.
Srivastava A, McKinnon W, Wood ME:Risk of breast and ovarian cancer in womenwith strong family histories. Oncology 15:905-907, 911-913, 2001.
2.
Available at http://www.myriadtests.com/provider/mutprev.htm. Accessed November 14,2003.
3.
Available at http://astor.som.jhmi.edu/brcapro/. Accessed November 14, 2003.
4.
Kuhl CK, Schrading S, Leutner CC, et al:Surveillance of “high risk” women with provedor suspected familial (hereditary) breast cancer:First mid-term results of a multi-modalityclinical screening trial (abstract 4). Proc AmSoc Clin Oncol 22:2, 2003.
5.
Kriege M, Breckelmans CTM, Boetes C, et al: MRI screening for breast cancer in womenwith high familial and genetic risk: First resultsof the Dutch MRI screening study(MRISC) (abstract 5). Proc Am Soc Clin Oncol22:2, 2003.
6.
Meijers-Heijboer H, van Geel B, vanPutten WLJ, et al: Breast cancer after prophylacticbilateral mastectomy in women with aBRCA1 or BRCA2 mutation. N Engl J Med345:159-164, 2001.
7.
Fisher B, Costantino JP, Wickerham DL,et al: Tamoxifen for prevention of breast cancer:Report of the National Surgical AdjuvantBreast and Bowel Project P-1 Study. J NatlCancer Inst 90:1371-1388, 1998.
8.
Narod SA, Brunet JS, Ghadirian P, et al:Tamoxifen and risk of contralateral breast cancerin BRCA1 and BRCA2 mutation carriers:A case-control study. Hereditary Breast CancerClinical Study Group. Lancet 356:1876-1881, 2000.
9.
Kauf ND, Satagopan JM, Robson ME, etal. Risk-reducing salpingo-oophorectomy inwomen with a BRCA1 or BRCA2 mutation. Engl J Med 346:1609-1615, 2002.
10.
Rebbeck TR: Prophylactic oophorectomyin BRCA1 and BRCA2 mutation carriers.J Clin Oncol 18:100S-103S, 2002.
11.
Weber BL: Risk management in BRCA1and BRCA2 mutation carriers: Lessons learned,challenges posed. J Clin Oncol 20:1164-1166,2002.
12.
Eisen A, Rebbeck TR, Wood WC, et al:Prophylactic surgery in women with hereditary predisposition for breast and ovarian cancer. JClin Oncol 18:1980-1995, 2000.
13.
Klamer TW, Donegan WL, Max MH:Breast tumor incidence in rats after partial mammaryresection. Arch Surg 118:933-935, 1983.
14.
Wong JH, Jackson CF, Swanson JS, etal: Analysis of the risk reduction of prophylacticpartial mastectomy in Sprague-Dawley ratswith 7, 12-dimethylbenzanthracene-inducedbreast cancer. Surgery 99:67-71, 1986.
15.
Nelson H, Miller SH, Buck D, et al: Effectivenessof prophylactic mastectomy in theprevention of breast tumors in C3H mice. PlastReconstr Surg 83:662-669,1989.
16.
Baasch M, Nielsen SF, Engholm G, etal: Breast cancer incidence subsequent to surgicalreduction of the female breast. Br J Cancer73:961-963, 1996.
17.
Hartmann LC, Schaid DJ, Woods JE, etal: Efficacy of bilateral prophylactic mastectomyin women with a family history of breastcancer. N Engl J Med 340:77-84, 1999.
18.
Schrag D, Kuntz KM, Garber JE, et al:Decision analysis: Effects of prophylactic mastectomyand oophorectomy on life expectancyamong women with BRCA1 or BRCA2 mutations.N Engl J Med 336:1465-1471, 1997.
19.
Pennisi VR, Capozzi A: Subcutaneousmastectomy data: A final statistical analysis of1500 patients. Aest Plas Surg 13:15-21, 1989.
20.
Carlson GW, Styblo TM, Moore B, etal: Skin sparing mastectomy. Oncologic andreconstruction considerations. Ann Surg225:570-575, 1997.