African-American genetic mutations pose Rx challenge
Lung cancer is not a discriminate disease, but the disease burden is especially high on African Americans in the U.S. The statistics are stark: African-American men are 37% more likely to develop lung cancer than white men and are 22% more likely to die of it. In addition, only 12% of African Americans live longer than five years after a diagnosis of lung cancer, compared with 16% of whites, according to a recent report by the American Lung Association.
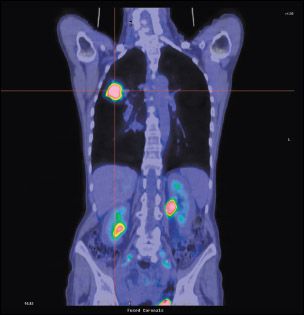
A PET/CT fusion image, frontal (coronal) section, showing non-small-cell lung cancer (NSCLC) of the right lung (on the left in this image). The large spot represents cancer of the lung at an advanced stage.
Lung cancer is not a discriminate disease, but the disease burden is especially high on African Americans in the U.S. The statistics are stark: African-American men are 37% more likely to develop lung cancer than white men and are 22% more likely to die of it. In addition, only 12% of African Americans live longer than five years after a diagnosis of lung cancer, compared with 16% of whites, according to a recent report by the American Lung Association (see Fact box).
One suggested reason for this gap in outcomes is differences in race-based genetics. In the era of personalized medicine and treatments that target specific disease pathways, identifying genetic differences among populations is becoming increasingly important to optimize benefit.
In lung cancer, it is well established that patients with non-small-cell lung cancer (NSCLC) who harbor the epidermal growth factor receptor (EGFR) gene mutation benefit from the targeted therapies erlotinib (Tarceva) and gefitinib (Iressa).
FACT ALA report "Too Many Cases, Too Many Deaths: Lung Cancer in African Americans," can be accessed at
www.lungusa.org/about-us/our-impact/top-stories/african-americans-and-lung-cancer.html
.

"Differences in [lung cancer] treatment for African Americans are more important than the genetic differences." - WILLIAM J. HICKS, MD
Data are mixed on the importance of EGFR mutations in the African-American population: Some research finds that the mutation is infrequent in African Americans while other data indicate no difference in the frequency of this mutation between African Americans and whites. Furthermore, how does genetic difference influence treatment? Oncology News International spoke with lung cancer experts on the current data on EGFR mutations in this population and the current therapeutic options.
"The whole emphasis on genetic analysis is in its infancy," said William J. Hicks, MD, one of the authors of the ALA report. "Certainly data are going to evolve, and we are going to modify our suggestions and approach based on that." Dr. Hicks is a professor of clinical medicine, division of hematology and oncology, at the Ohio State University Comprehensive Cancer Center–Arthur G. James Cancer Hospital and Richard J. Solove Research Institute in Columbus.
Disparate data
Rom S. Leidner, MD, and colleagues at Case Western Reserve University in Cleveland found that African Americans were significantly less likely to have the EGFR mutation than whites. Among 53 African Americans in the study, only one carried the EGFR mutation whereas the mutation was found in 15 of 89 whites (2% vs 17%; P = .02).
The authors suggested that because African Americans are more likely to have a lower frequency of the EGFR mutation, therapies that target EGFR may be less beneficial to them (J Clin Oncol 27:5620-5626, 2009).
"We know that in people who have the mutation, there is a higher rate of response to therapy," Dr. Leidner said. "We know the rates of mutation in different populations are different. In East Asians, it is the highest. In Caucasians, it is about 12%, and in African Americans, 0%."
To understand better the clinical responses in African Americans with NSCLC who receive targeted therapies, Dr. Leidner's group is currently reviewing radiographic studies of African Americans with NSCLC who were treated with targeted therapies, to objectively measure tumor shrinkage before and after treatment.
Researchers at New York's Memorial Sloan-Kettering Cancer Center included a larger sample population of 121 African Americans, and they found no difference in the frequency of EGFR mutations between black and white patients (19% vs 18%; P = 0.9; ASCO 2009 abstract 11065).

MELISSA JOHNSON, MD
"The crux of our study was that we found an equivalent frequency of EGFR mutations amongst our African American cohort, as compared to our Caucasian cohort," said Melissa Johnson, MD, a senior medical oncology fellow in the thoracic oncology group at MSKCC.
According to Dr. Leidner, the disparity between his group's findings and that of the MSKCC group suggests that newer methods of detection may be much more sensitive to finding EGFR mutations. "I don't think we have enough information to know the answers to these questions, but in the end, these are surrogates for what we ultimately want to know, which is how to determine which patients will benefit most from which type of therapy," he said.
KRAS mutations are another area where racial differences may impact treatment outcomes. While the MSKCC investigators found that Caucasians were significantly more likely to have the KRAS mutation than the African-American cohort, the Case Western Reserve study found no significant difference in the frequency of KRAS mutation between the two populations. Both Dr. Leidner and Dr. Johnson said that the clinical importance of KRAS mutations is uncertain, especially since there is no drug currently available that effectively targets the KRAS mutation.
Clinical application
Given the current evidence, is it worthwhile for African-American patients to undergo EGFR testing? The experts said "yes."

PAUL A. BUNN JR., MD
All patients with lung cancer should be tested for the EGFR mutation regardless of race, sex, or any other population identifier, said Paul A. Bunn, Jr., MD, James Dudley professor of lung cancer research at the University of Colorado in Aurora. Citing other well-established variables that are also associated with low frequency of EGFR mutations (male gender, smoking), Dr. Bunn emphasized the need for multivariate analyses to isolate any one particular variable such as race.
Poor performance status plagues black lung cancer patients
The disparity in lung cancer outcomes may be due to more advanced disease and poorer performance status at presentation in African Americans. A recent study from the Sylvester Comprehensive Cancer Center, University of Miami looked at the Florida cancer registry and inpatient and ambulatory data for lung cancer patients from 1998 to 2002. A total of 76,086 patients were identified, with 92.7% Caucasian and 6.7% African American.
The study authors reported that black patients presented at a younger age with more advanced disease and were less likely to undergo surgical therapy than their white counterparts. Their median survival time was 7.5 months vs 7 months for the entire cohort.
Stepwise multivariate analysis revealed that African-American race was no longer a statistically significant predictor of worse outcomes once corrections were made for demographics and comorbidities. "Emphasis must be placed on improving pretreatment performance status among African American patients," they wrote (
Cancer
116:2437-2447, 2010).
"If you thought the biomarker test was more expensive than the drug, which it isn't, you might say that you should select for testing the group most likely to have the mutation," he said. But Dr. Bunn emphasized that would be a bad deal for patients who actually have the mutation but happen to fall in a population that has been shown to have less frequent mutations.
Dr. Hicks agreed that checking for the mutation in every patient with NSCLC is needed and believes that most sophisticated medical oncology centers check for this mutation frequently.
The situation gets a bit more complicated in patients without the EGFR mutation. According to Dr. Hicks, data show that between 19% and 27% of people without the mutation respond to erlotinib.
"I liken this to an orchestra with a lot of these mutations being the players, and we sometimes don't know how they interact," he said. "So we may ultimately find that the reason that people still respond to the EGFR inhibitors despite not having the mutation is that there are other mutations that allow them to impact on EGFR inhibition."
Given the current discrepancies in treatment for African Americans, pinpointing which therapy will serve them best is crucial. According to the ALA report, blacks are less likely to undergo staging. In addition, they are less likely to have surgery (34% vs 61.6% of whites) and are less likely to receive chemotherapy (28.6% vs 46.9%). A recent study of more than 83,000 Medicare patients found that the disparity was relatively unchanged over the 12-year course of the study (Cancer 115:2199-2211, 2009; J Clin Oncol 24:413-418, 2006).
"These differences in treatment for African Americans are more important than the genetic differences," Dr. Hicks said. "As a consumer advocate, I am suggesting that when faced with lung cancer, you certainly want to be treated by an institution or individual who has significant experience and a track record with that illness. Adequate staging to pick the best treatment is very important."