Anti-Angiogenesis Therapy in Ovarian Cancer: Which Patient is It Most Likely to Benefit?
This review summarizes the major clinical trials that led to the approval of antiangiogenic drugs for ovarian cancer and gives a brief view into novel combinations of bevacizumab with other targeted therapies in an attempt to enhance the efficacy of bevacizumab.
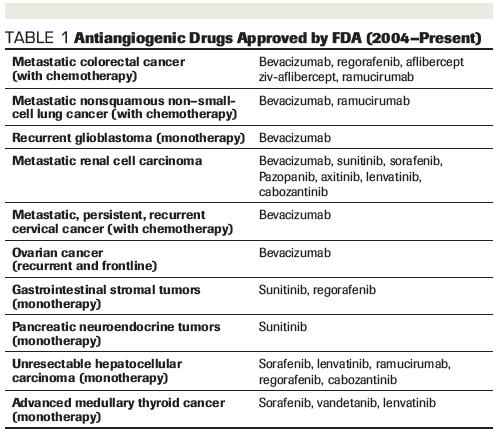
TABLE 1: Antiangiogenic Drugs Approved by FDA (2004–Present)
Anca Chelariu-Raicu, MD, PhD

Robert L. Coleman, MD

Anil K. Sood, MD

Abstract: Angiogenesis is known to play an important role in normal ovarian physiology as well as in growth and progression of ovarian cancer. The first FDA approval of bevacizumab in 2004 was for metastatic colorectal cancer in combination with chemotherapy; this was a key point for several subsequent approvals of antiangiogenic drugs. The efficacy of bevacizumab treatment is modest, however, and most ovarian cancer patients eventually develop acquired resistance, which highlights the need for new targeted therapies and/or combination strategies. Understanding the multitude of variables in response to antiangiogenic therapy would offer potential strategies for selecting patients most likely to benefit from such therapy.
Introduction
The principles of antiangiogenic therapy are rooted in observations made by Folkman and others over 40 years ago.[1] Since then, antiangiogenic therapies have been incorporated into clinical care for many cancer patients. The vascular endothelial growth factor (VEGF)/VEGF receptor (VEGFR) pathway is arguably the most advanced for clinical development. This pathway has been extensively studied for its role in development of malignant ascites and tumor progression.[2] The VEGF molecule is a key angiogenic factor, which is involved in development of physiologic and pathologic neovascularization. VEGF is a growth as well as proliferation factor for endothelial cells and it binds to VEGFR-1 and VEGFR-2 as well as the cofactors neuropilin-1 (NRP-1) and NRP-2.[3] VEGFR-2 is expressed mostly on endothelial cells; VEGFR-1 can be expressed on macrophages, tumor cells, and fibroblasts.[4] While one of the main antiangiogenic approaches is to block VEGF using a monoclonal antibody, other drugs including VEGF pathway inhibitors such as small-molecule tyrosine kinase inhibitors (eg, sunitinib, sorafenib, pazopanib, regorafenib, lenvatinib, vandetanib), soluble VEGF decoy receptor (eg, aflibercept), and human monoclonal antibody against VEGFR-2 (ramucirumab) have also been developed.
Among the various antiangiogenic drugs, bevacizumab, a humanized anti-VEGF monoclonal antibody, is the most widely studied across tumor types and specifically in epithelial ovarian cancer. Beginning in 2004, the US Food and Drug Administration (FDA) granted several approvals for antiangiogenic drugs with a main indication in metastatic disease for colorectal cancer, non–small-cell lung, renal cell, cervical, and ovarian cancers, and glioblastoma. Recently, in June 2018, bevacizumab was approved for the first time also for frontline therapy for ovarian cancer in combination with platinum and taxane-based chemotherapy. Despite positive initial response rates using bevacizumab in advanced ovarian cancer, patients unfortunately develop relapsed disease within weeks to months. Nevertheless, preclinical data suggest that prolonged administration of bevacizumab as maintenance therapy after platinum-based chemotherapy prolongs progression-free survival (PFS).[5] This review summarizes the major clinical trials that led to the approval of antiangiogenic drugs and gives a brief view into novel combinations of bevacizumab with other targeted therapies in an attempt to enhance the efficacy of bevacizumab.
Standard of Care
Ovarian cancer is the most deadly gynecologic malignancy with 5-year survival rates ranging from 47% for all stages compared to only 29% for those with advanced-stage disease (III or IV) and is responsible for approximately 14,000 deaths in the United States annually.[6] The standard-of-care treatment remains primary tumor reductive surgery followed by adjuvant platinum and taxane-based chemotherapy. However, the recurrence rate is approximately 80%, even for patients who respond to initial treatment.[7]
Bevacizumab as Upfront Therapy
GOG-218 and ICON7 were the first two positive advanced-stage frontline ovarian cancer randomized phase III trials that added bevacizumab to chemotherapy.[8,9] In both GOG-218 and ICON7, bevacizumab was added to the standard of care, which consists of 6 cycles of platinum and taxane-based chemotherapy. In GOG-218, the duration of bevacizumab treatment was up to 22 cycles using a dose of 15 mg/kg, and in ICON7, 18 cycles of bevacizumab were given using a dose of 7.5 mg/kg. Although the two trials used different treatment duration and dosing, they both showed an increase in PFS. In GOG-218, the median PFS after adding bevacizumab in frontline and maintenance was increased by 4 months, from 10.3 to 14.1 months (hazard ratio (HR), 0.72; 95% CI, 0.63–0.82).[8] In ICON7, PFS at 36 months was 20.3 months with standard therapy, as compared with 21.8 months with standard therapy plus bevacizumab (HR, 0.81; 95% CI, 0.70–0.94; P = .004).[9] The same study suggested that the benefit of adding bevacizumab was the greatest for patients with high risk of progression (International Federation of Gynecology and Obstetrics [FIGO]) stage III > 1 cm or IV or suboptimally debulked surgery) where the estimated median PFS was 10.5 months with standard therapy, as compared with 15.9 months with bevacizumab (HR, 0.68; 95% CI, 0.55–0.85; P < .001).[9] Another intriguing observation of the study was that the effect on PFS was lost when the therapy with bevacizumab was withdrawn.[9,10] In this context, the optimal strategy for bevacizumab might be to continue the treatment until disease progression, as indicated by the data in the OCEANS trial in recurrent platinum-sensitive setting, where the experimental arm consisted of standard chemotherapy, gemcitabine plus carboplatin, in combination with bevacizumab as maintenance.[11] The same observation was made in the GOG-213 trial where the enrolled patients presenting recurrent platinum-sensitive disease were randomly assigned to standard paclitaxel and carboplatin every 3 weeks with or without bevacizumab. The latter was continued as maintenance every 3 weeks until disease progression or unacceptable toxicity.[12] As already mentioned from the OCEANS trial results, the effects of adding bevacizumab to chemotherapy and continuation as maintenance were reproducible. This was also the case in patients enrolled in the GOG-213 trial, where the median overall survival (OS) in the chemotherapy plus bevacizumab group was 42.2 months (95% CI, 37.7–46.2) vs 37.3 months (95% CI, 32.6–39.7) in the chemotherapy group (HR, 0.829; 95% CI, 0.683–1.005; P = .056).[12] Results from the ENGOT-ov15/AGO-OVAR 17 trial will most probably give an answer to the optimal treatment duration with bevacizumab, as this trial consists of 2 experimental arms, one being frontline chemotherapy combined with bevacizumab for 15 months while the second arm incorporates bevacizumab with the same frontline chemotherapy, but for a longer period (30 months). Considering the increase in PFS and OS after administering bevacizumab in frontline therapy in GOG-218 and ICON7, the European Medicines Agency (EMA) granted first approval of the drug for ovarian cancer in 2011 while the FDA approved it in June 2018.
Other Antiangiogenic Drugs Used as Upfront Therapy
Other multitarget compounds have demonstrated promising results in phase III trials. In the AGO-OVAR 16 trial, pazopanib (a protein kinase inhibitor of VEGFR and platelet-derived growth factor receptor [PDGFR]) maintenance therapy showed that PFS was higher in the experimental arm with a median improvement of 5.6 months (HR, 0.77; 95% CI, 0.64–0.91). Grade 3 or 4 hypertension (30.8%), neutropenia (9.9%), liver-related toxicity (9.4%), and diarrhea (8.2%) were significantly higher in the pazopanib arm.[13] A substudy of the same group of patients looked at the germline BRCA1 or BRCA2 mutation status and explored the effectiveness of maintenance therapy with pazopanib in these patients. Consistent with previous observations, germline BRCA status was prognostic, demonstrating that the median PFS was longer in the placebo arm for the BRCA1 or BRCA2 mutation carriers versus BRCA1 or BRCA2 wild-type patients (30.3 vs 14.1 months) (HR, 0.48; 95% CI, 0.29–0.78).[14] In another study, DNA from tumor and blood samples from patients enrolled in GOG-218 were sequenced, showing that patients with mutations in homologous recombination repair (HRR) had significantly prolonged PFS and OS when compared to those without mutations.[15] These data show that genetic testing plays an important role with regard to prognostic implications and should be discussed with all patients. This is particularly relevant for treatment with poly (ADP-ribose) polymerase (PARP) inhibitors.[16] There was no positive or negative correlation between HRR and the use of bevacizumab as maintenance therapy in this study.[15]
In the AGO-OVAR 12 study, another multitargeted compound, nintedanib (a potent inhibitor of VEGFR, fibroblast growth factor receptor [FGFR], and PDGFR), was investigated. Patients with advanced ovarian cancer were given standard-of-care chemotherapy, carboplatin and paclitaxel, and randomized to nintedanib or placebo. The median PFS was significantly improved in the experimental arm compared with placebo (17.2 vs 16.6 months) (HR, 0.84; 95% CI, 0.72–0.98). Patients treated with nintedanib reported grade 3 adverse effects such as diarrhea (21% vs 2%), thrombocytopenia (12% vs 5%), and anemia (12% vs 6%).[17] Another trial with trebananib, a selective angiopoietin-1 (Ang1) and Ang2 neutralizing peptibody, examined its effects in combination with standard chemotherapy as well as maintenance. This trial was a randomized study, in which patients received trebananib or placebo plus carboplatin and paclitaxel as first-line treatment. The primary endpoint of the study, PFS, did not show any improvement after the combination of trebananib with carboplatin and paclitaxel.[18]
Bevacizumab and Other Antiangiogenic Drugs Used in the Relapse Setting, Platinum Resistant
While the antiangiogenic frontline therapy was seen from different perspectives by the FDA and the EMA, bevacizumab was initially granted FDA approval for use in recurrent ovarian cancer based on the AURELIA trial. The experimental arm of this trial consisted of adding bevacizumab to chemotherapy until disease progression. Patients who received bevacizumab had a median PFS of 6.7 vs 3.4 months in patients receiving chemotherapy alone (HR, 0.48; 95% CI, 0.38–0.60) and median OS of 16.6 vs 13.3 months, respectively (HR, 0.85; 95% CI, 0.66–1.08).[19] Another trial, TRINOVA-1, aimed to determine whether adding trebananib to weekly paclitaxel until disease progression would improve PFS. This trial showed that inhibition of Ang1/Ang2 determined a prolongation of PFS but not over the benefit of bevacizumab.[20] A third randomized phase III trial, ENGOT-ov-6/TRINOVA-2, which had a similar study design to TRINOVA-1, evaluated PFS and OS after adding trebananib to pegylated liposomal doxorubicin (PLD) in patients with recurrent ovarian cancer (platinum sensitive and resistant). Patients in the experimental arm had a median PFS of 7.6 months (95% CI, 7.2–9.0) vs 7.2 months (95% CI, 4.8–8.2) in the placebo arm (HR, 0.92; 95% CI, 0.68–1.24). Trebananib demonstrated anticancer activity indicated by improved objective response rate (46% vs 21% in the placebo arm [odds ratio, 3.43; 95% CI, 1.78–6.64]). Median duration of response was also improved in the trebananib arm (7.4 months; 95% CI, 5.7–7.6) vs placebo (3.9 months; 95% CI, 2.3–6.5).[21]
Bevacizumab and Other Antiangiogenic Drugs Used in the Relapse Setting, Platinum Sensitive
In patients with recurrent platinum-sensitive ovarian cancer, the OCEANS and GOG-213 trials led to important advances. In the OCEANS trial, bevacizumab or placebo was added to gemcitabine and carboplatin for 6 to 10 cycles and then continued until progression. The addition of bevacizumab led to a statistically significant increase in PFS (HR, 0.484; 95% CI, 0.388–0.605). Median PFS was 12.4 months for bevacizumab vs 8.4 months in the placebo group.[11] In the GOG-213 trial, a different chemotherapy backbone (paclitaxel and carboplatin) was used and it was not placebo-controlled due to its primary endpoint being OS. In addition, surgical randomization for candidates deemed appropriate for secondary surgery was done for about 16% of the intent-to-treat population. This trial also demonstrated an increase in the median PFS in the bevacizumab plus chemotherapy arm compared with chemotherapy alone (13.8 months vs 10.4 months). Of note, GOG-213 showed a positive trend in median OS from 37.3 months in the chemotherapy group to 42.2 months in the chemotherapy plus bevacizumab group (HR, 0.829; 95% CI, 0.683–1.005; P = .056), which when adjusted for platinum-free interval and participation in the surgical objective, was significantly associated with OS (HR, 0.823; 95% CI, 0.680–0.996, P = .0447).[12] While the patients in the OCEANS trial did not receive bevacizumab with the frontline treatment, a third trial, MITO16B-MaNGO OV2B-ENGOT OV17, enrolled patients with carboplatin-sensitive relapsed disease who had had previous bevacizumab treatment. They found that bevacizumab in combination with a platinum-based doublet is associated with significantly prolonged PFS and a good safety profile.[22] Results from AGO OVAR 2.21, which evaluated patients with relapsed disease who previously had bevacizumab in frontline, were presented during the ESMO 2018 meeting. In this study, both arms contained bevacizumab added to a platinum-based chemotherapy; one arm consisted of gemcitabine and carboplatin and the other arm consisted of PLD and carboplatin. Being the first phase III trial in ovarian cancer comparing two bevacizumab-containing regimens, the study showed that the carboplatin/PLD/bevacizumab combination resulted in superior PFS compared with carboplatin/gemcitabine/bevacizumab (HR, 0.80; 95% CI, 0.68–0.96; P = .0128).[23]
Only one antiangiogenic VEGF receptor 1-3 inhibitor investigated in recurrent platinum-sensitive ovarian cancer patients so far has shown anti-tumor activity. In the 3-arm ICON6 trial, participants were randomly assigned to receive placebo plus chemotherapy then placebo maintenance (arm A), cediranib 20 mg once daily plus chemotherapy then placebo maintenance (arm B), or cediranib 20 mg once daily plus chemotherapy then cediranib 20 mg once daily for maintenance (arm C). Median PFS was 11 months for arm C vs 8.7 months for arm A (HR, 0.56; 95% CI, 0.44–0.72). The difference in OS was nonsignificant (P = .3) across the 3 arms.[24] Although the improvement in PFS to a median of 11 months with cediranib as maintenance is similar to that reported with bevacizumab maintenance after chemotherapy, the risk of hypertension, fatigue, diarrhea, and nausea in patients taking cediranib in combination with chemotherapy makes this a worse candidate compared to intravenous bevacizumab.
Other Emerging Antiangiogenic Therapies in Combination With Anti-VEGF Drugs
Using antiangiogenic drugs to target the VEGF molecule or angiogenic receptors such as VEGFR, FGFR, and PDGFR proved to be an effective strategy for inhibiting tumor angiogenesis. The effects on PFS and OS are modest, as most patients develop adaptive resistance to anti-VEGF therapy and eventually present with progressive disease. Novel concepts that combine antiangiogenic drugs with other emerging approaches such as Delta-like ligand 4 (DLL4)-blocking antibody,[25,26] and colony stimulating factor 1 receptor (CSF1R) found on macrophages,[27] are showing promising results in decreasing tumor burden in vivo.[25-27] Previous studies that investigated the DLL4 pathway showed that DLL4 blockade can inhibit tumor growth by promoting nonproductive angiogenesis.[25] Furthermore, dual targeting of VEGF and DLL4 showed superior anti-tumor effects (decreased tumor burden, less ascites) in ovarian cancer mouse models compared with either therapy alone.[26] Navicizixumab, a DLL4 and VEGF inhibitor, is a clinical candidate being tested in a phase I/Ib study.[28]
With the genetic ablation of CSF1R and thereby macrophages, it was observed that the macrophages could have a protumoral effect.[29,30] Additional studies have shown that macrophages support tumor growth by production of proangiogenic factors as VEGF and other angiogenic chemokines (eg, CXCL12).[31] After emergence of resistance to anti-VEGF therapy and paclitaxel in an in vivo mouse model, CSF1R inhibitor therapy added to anti-VEGF therapy restored response to antiangiogenic therapy and an 83% lower tumor burden compared to treatment with anti-VEGF therapy and paclitaxel alone.[27]
Other Interesting Combinations
Phase III clinical trials showed that adding PARP inhibitors in maintenance therapy improves PFS for patients with recurrent epithelial ovarian, fallopian-tube, or primary peritoneal cancer who had received prior platinum-based chemotherapy.[32,33] The SOLO-1 study demonstrated that the risk of disease progression or death was 70% lower with olaparib than with placebo (HR, 0.3; 95% CI, 0.23–0.41; P < .001) in patients with newly diagnosed advanced ovarian cancer who have a complete or partial response after platinum-based chemotherapy.[16] Taking into account the response rate to PARP inhibitors, the combination of PARP inhibitor with bevacizumab is the premise of the PAOLA-1 phase III clinical trial. Specifically, olaparib and bevacizumab are used in frontline maintenance in advanced ovarian cancer. Different combinations of PARP inhibitors and antiangiogenic drugs are studied in the NRG-GY005 (NCT02502266) phase II/III and NRG-GY004 (NCT02446600) phase III trials in which a PARP inhibitor is given alone or in combination with cediranib maleate in the experimental arms to determine efficacy compared with standard platinum-based chemotherapy in platinum-sensitive relapsed ovarian cancer.
VEGF inhibitors in combination with immunotherapy are also being investigated. The rationale for combining immunotherapy with VEGF inhibitors is that the latter induce abundant tumor vasculature and inhibit directly T-cell function.[34] There are several promising trials in development evaluating immunotherapy in combination with VEGF inhibitors such as NRG-GY009 (NCT02839707), ATLANTE (NCT02891824), and IMagyn050 (NCT03038100).
Possible Markers of Response to Antiangiogenic Therapy
Treatment with antiangiogenic agents can be quite expensive and can have substantial side effects. One potential solution for optimizing the treatment is to identify useful biomarkers that can allow selection of patients most likely to benefit from such therapy and potentially to detect early escape from anti-VEGF therapy. Circulating molecular and cellular biomarkers in blood would be ideal candidates, as such markers can be followed longitudinally. However, circulating protein levels (eg, VEGF or other angiogenic molecules such as placental growth factor [PIGF]) have not been particularly effective.[35]
Circulating endothelial cells (CECs) are mobilized in murine models as well as in humans in response to VEGF.[36,37] This is especially important because the level of CECs should decrease in response to anti-VEGF therapy. Although the suppression of mobilized endothelial cells was observed in patients with confirmed response to anti-VEGF therapy, an increase in value before clinical progression was not noted.[38]
Some have attempted to identify molecular subgroups of high-grade serous ovarian cancer that could predict response to anti-VEGF therapy. For example, Gourley and colleagues identified three major subgroups in the ICON7 participants based on mRNA analysis of human tissue samples. In two of the subgroups, the angiogenic genes were upregulated, while the third subgroup presented more complex features including repression of the angiogenic genes and upregulation of the immune genes. With regard to OS, the latter group had a superior OS compared to the other two subgroups. However, addition of bevacizumab therapy in this latter group was associated with worse PFS and OS compared to chemotherapy alone. This study suggests that an immune subgroup “geno-signature” with the repressed angiogenic-related expression could better select patients in whom antiangiogenic therapy could be avoided. Addition of bevacizumab in the proangiogenic group was associated with a nonsignificant trend for improved PFS compared with controls (median, 17.4 vs 12.3 months, respectively).[39]
Given the lack of reliable plasma biomarkers, imaging modalities such as CT and MRI scans are the most common assessment tools to evaluate efficacy. However, other functional imaging methods such as dynamic contrast-enhanced (DCE)-MRI and CT perfusion can provide information on tumor perfusion, vascularity, and permeability and could be useful as early markers of treatment efficacy.[38,40,41] The ACRIN 6695 study investigated whether CT perfusion biomarkers are associated with PFS in patients with advanced ovarian cancer treated with carboplatin and dose-dense or conventional paclitaxel. The patients were enrolled from the prospective phase III GOG-0262 clinical trial in which bevacizumab use was left to the physician’s choice and was overwhelmingly preferred based on the results from previous clinical trials in patients with advanced ovarian cancer. The study showed that changes in vasculature parameters within 4 weeks of initiating therapy in one or more CT-perfusion biomarkers were associated with shorter PFS, proving that these biomarkers can be considered good imaging candidates to provide early prognostic information.[41]
Future Directions
The number of antiangiogenic drugs developed during the last 30 years is impressive and is associated with improved patient outcomes. Nevertheless, due to emergence of adaptive resistance, additional therapies are needed. Steps forward would be made with the identification of predictive biomarkers that could help assess the response among patients and a better understanding of mechanisms of adaptive resistance. While neutralization of VEGF was the first approach for targeting the tumor microenvironment, additional approaches (eg, immune therapy) have been also quite successful. In this context, the potential of tumor vessel normalization using antiangiogenic drugs to improve the effectiveness of immunotherapy should be explored further. Collectively, such microenvironment-targeted approaches hold promise for further improving the outcomes of women with ovarian cancer.
FINANCIAL DISCLOSURES:Dr. Chelariu-Raicu has no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article. Dr. Sood has received funding from Merck, Kiyatec, and Bio-Path. Dr. Coleman has been a consultant, speaker, or advisor for AbbVie, Cell Medica, Genmab, MORE Health, Takeda, Roche, Merck, Aravive, ArQule, AstraZeneca, Clovis, Eisai, Genentech, Immunogen, and Janseen.
PERSPECTIVE

ncorporating Antiangiogenic Agents in the Treatment of Advanced Ovarian Cancer
Kristina Frinzi Byers, PharmD, BCOP
The incorporation of antiangiogenic therapy in the treatment of solid tumor malignancies dates back to 2004, when bevacizumab, an anti-vascular endothelial growth factor (VEGF) monoclonal antibody, received US Food and Drug Administration (FDA) approval in advanced colorectal cancer after demonstrating an improvement in both overall and progression-free survival (PFS).[1] Studies in epithelial ovarian cancer have shown a correlation between VEGF expression and more advanced disease leading to worse survival rates.[2] After initial skepticism, bevacizumab was finally granted FDA approval in 2011 for recurrent ovarian cancer and has since received approval in 2018 as front-line therapy after initial surgical resection.[3] Other antiangiogenic agents of interest include pazopanib, nintedanib, cediranib, and navicizumab, all of which are currently being evaluated in clinical trials.
Although bevacizumab demonstrated a modest improvement in PFS, the unique toxicity profile of antiangiogenic therapies and the lack of an overall survival benefit must be considered when selecting patients most appropriate for treatment. Common adverse effects can be divided into these major categories: generalized, cardiovascular, gastrointestinal (GI), and dermatologic. Generalized symptoms primarily include fatigue, headache, dyspnea, arthralgia, and myalgia.[4] In the phase III PALETTE trial that evaluated using pazopanib in treating advanced soft-tissue sarcoma, the incidence of all-grade and grade > 3 fatigue was 65% and 13%, respectively.[5] Although not FDA approved for use in ovarian cancer, the debilitating fatigue associated with pazopanib often warrants dose modification to improve tolerability. Cardiovascular symptoms such as hypertension and venous thromboembolism can be concerning in a primarily postmenopausal population. Frequent blood pressure (BP) monitoring is essential when treating patients with baseline hypertension, and all patients should have adequate BP control prior to initiating treatment with anti-VEGF therapies. Common GI symptoms include diarrhea and abdominal pain. More severe GI adverse events (ie, perforation, fistula, and/or necrosis) have been reported in 2.9% of patients with ovarian cancer, and identifiable risk factors include history of inflammatory bowel disorder and previous bowel resection.[6] Palmar-plantar erythrodysesthesia has been reported in patients receiving anti-VEGF therapies, and early identification of symptoms is essential in preventing dose interruptions. Impaired wound healing can result in serious or fatal complications; therefore, anti-VEGF therapies should be held at least 28 days prior to and after elective invasive procedures.[4] Considering the potentially substantial toxicities associated with bevacizumab and other anti-VEGF agents, their incorporation into the standard treatment of ovarian cancer should be reserved for patients with high-risk clinical features and minimal comorbidities.
FINANCIAL DISCLOSURE:Dr. Byers has served on advisory boards for Pfizer, Tesaro, and Heron Therapeutics, and participated in surveys for The Delham Group.
REFERENCES
1. Genentech press release. FDA approves Avastin, a targeted therapy for first-line metastatic colorectal cancer patients. February 26, 2004. Available at: https://www.gene.com/media/press-releases/7167/2004-02-26/fda-approves-avastin-a-targeted-therapy. Accessed July 1, 2019.
2. Duncan TJ, Al-Attar A, Rolland P, et al. Vascular endothelial growth factor expression in ovarian cancer: a model for targeted use of novel therapies. Clin Cancer Res. 2008;14:3030-5.
3. US Food and Drug Administration. FDA approves bevacizumab in combination with chemotherapy for ovarian cancer. June 13, 2018. Available at: www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm610664.htm. Accessed July 1, 2019.
4. Avastin (bevacizumab) [prescribing information]. South San Francisco, CA: Genentech, Inc.; February 2019.
5. van der Graaf WT, Blay JY, Chawla SP, et al; EORTC Soft Tissue and Bone Sarcoma Group; PALETTE study group. Pazopanib for metastatic soft-tissue sarcoma (PALETTE): a randomized, double-blind, placebo-controlled phase 3 trial. Lancet. 2012;379:1879-86.
6. Burger RA, Brady MF, Bookman MA, et al. Risk factors for GI adverse events in a phase III randomized trial of bevacizumab in first-line therapy of advanced ovarian cancer: a gynecologic oncology group study. J Clin Oncol. 2014;32:1210-7.
References:
1. Folkman J. Tumor angiogenesis: Therapeutic implications. N Engl J Med. 1971; 285:1182-6.
2. Graybill W, Sood AK, Monk BJ, Coleman RL. State of the science: emerging therapeutic strategies for targeting angiogenesis in ovarian cancer. Gynecol Oncol. 2015;138:223-6.
3. Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298-307.
4. Fischer C, Mazzone M, Jonckx B, Carmeliet P.FLT1 and its ligands VEGFB and PlGF: drug targets for anti-angiogenic therapy? Nat Rev Cancer. 2008;8:942-56.
5.Mabuchi S, Terai Y, Morishige K, et al. Maintenance treatment with bevacizumab prolongs survival in an in vivo ovarian cancer model. Clin Cancer Res. 2008;14:7781-9.
6.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7-34.
7.Monk BJ, Herzog TJ, Tewari KS. Evolution of chemosensitivity and resistance assays as predictors of clinical outcomes in epithelial ovarian cancer patients. Curr Pharm Des. 2016;22:4717-28.
8.Burger RA, Brady MF, Bookman MA, et al. Gynecologic Oncology Group. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N Engl J Med. 2011;365:2473-83.
9.Perren TJ, Swart AM, Pfisterer J, et al. A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med. 2011;365:2484-96.
10.Oza AM, Cook AD, Pfisterer J, et al. Standard chemotherapy with or without bevacizumab for women with newly diagnosed ovarian cancer (ICON7): overall survival results of a phase 3 randomised trial. Lancet Oncol. 2015;16:928-36.
11.Aghajanian C, Blank SV, Goff BA, et al. OCEANS: a randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. J Clin Oncol. 2012;30:2039-45.
12.Coleman RL, Brady MF, Herzog TJ, et al. Bevacizumab and paclitaxel-carboplatin chemotherapy and secondary cytoreduction in recurrent, platinum-sensitive ovarian cancer (NRG Oncology/Gynecologic Oncology Group study GOG-0213): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2017;18:779-91.
13.du Bois A, Floquet A, Kim JW, et al. Incorporation of pazopanib in maintenance therapy of ovarian cancer. J Clin Oncol. 2014;32:3374-82.
14.Harter P, Johnson T , Berton-Rigaud D, et al. BRCA1/2 mutations associated with progression-free survival in ovarian cancer patients in the AGO-OVAR 16 study. Gynecol Oncol. 2016;140:443-9.
15.Norquist BM, Brady MF, Harrell MI, et al. Mutations in homologous recombination genes and outcomes in ovarian carcinoma patients in GOG 218: an NRG Oncology/Gynecologic Oncology Group Study. Clin Cancer Res. 2018;24:777-83.
16.Moore K, Colombo N, Scambia G, et al. Maintenance olaparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med. 2018;379:2495-505.
17.du Bois A, Kristensen G, Ray-Coquard I, et al. Standard first-line chemotherapy with or without nintedanib for advanced ovarian cancer (AGO-OVAR 12): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet Oncol. 2016;17:78-89.
18.Vergote I, Scambia G, O’Malley DM, et al. Trebananib or placebo plus carboplatin and paclitaxel as first-line treatment for advanced ovarian cancer (TRINOVA-3/ENGOT-ov2/GOG-3001): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2019;20:862-76.
19.Pujade-Lauraine E, Hilpert F, Weber B, et al. AURELIA: A randomized phase III trial evaluating bevacizumab (BEV) plus chemotherapy (CT) for platinum (PT)-resistant recurrent ovarian cancer (OC). J Clin Oncol. 2012;30(suppl):abstr LBA5002.
20.Monk BJ, Poveda A, Vergote I, et al. Anti-angiopoietin therapy with trebananib for recurrent ovarian cancer (TRINOVA-1): a randomised, multicentre, double-blind, placebo-controlled phase 3 trial. Lancet Oncol. 2014;15:799-808.
21.Marth C, Vergote I, Scambia G, et al. ENGOT-ov-6/TRINOVA-2: Randomised, double-blind, phase 3 study of pegylated liposomal doxorubicin plus trebananib or placebo in women with recurrent partially platinum-sensitive or resistant ovarian cancer. Eur J Cancer. 2017;70:111-21.
22.Pignata S, Lorusso D, Joly F. et al Chemotherapy plus or minus bevacizumab for platinum-sensitive ovarian cancer patients recurring after a bevacizumab containing first line treatment: the randomized phase 3 trial MITO16B-MaNGO OV2B-ENGOT OV17. J Clin Oncol. 2018;36(suppl):abstr 5506.
23.Pfisterer J, Dean AP, Baumann K. et al. Carboplatin/pegylated liposomal doxorubicin/bevacizumab (CD-BEV) vs. carboplatin/gemcitabine/bevacizumab (CG-BEV) in patients with recurrent ovarian cancer. A prospective randomized phase III ENGOT/GCIG-Intergroup study (AGO Study Group, AGO-Austria, ANZGOG, GINECO, SGCTG). Ann of Oncol. 2018:29(suppl 8):abstr 9330.
24.Ledermann JA, Embleton AC, Raja F, et al. Cediranib in patients with relapsed platinum-sensitive ovarian cancer (ICON6): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016; 387:1066-74.
25.Noguera-Troise I, Daly C, Papadopoulos NJ, et al. Blockade of Dll4 inhibits tumour growth by promoting non-productive angiogenesis. Nature. 2006;444:1032-1037.
26.Huang J, Hu W, Hu L, et al. Dll4 inhibition plus aflibercept markedly reduces ovarian tumor growth. Mol Cancer Ther. 2016;15:1344-52.
27.Lyons YA, Pradeep S, Wu SY, et al. Macrophage depletion through colony stimulating factor 1 receptor pathway blockade overcomes adaptive resistance to anti-VEGF therapy. Oncotarget. 2017;8:96496-505.
28.Jimeno A, Morre KN, Gordon M, et al. A first-in-human phase 1a study of the bispecific anti-DLL4/anti-VEGF antibody navicixizumab (OMP-305B83) in patients with previously treated solid tumors. Invest New Drugs. 2019;37:461-72.
29.Lin EY, Nguyen AV, Russell RG, Pollard JW. Colony-stimulating factor 1 promotes progression of mammary tumors to malignancy. J Exp. Med. 2001;193,727-40.
30.Lin EY, Pollard JW. Tumor-associated macrophages press the angiogenic switch in breast cancer. Cancer Res. 2007;67:5064-6.
31.Hughes R, Qian BZ, Rowan C, et al. Perivascular M2 macrophages stimulate tumor relapse after chemotherapy. Cancer Res. 2015;75:3479-91.
32.Mirza MR, Monk BJ, Herrstedt J, et al. Niraparib maintenance therapy in platinum-sensitive, recurrent ovarian cancer. N Engl J Med. 2016;375:2154-64.
33.Coleman RL, Oza AM, Lorusso D, et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:1949-61.
34.Yang J, Yan J, Liu B. Targeting VEGF/VEGFR to modulate antitumor immunity. Front Immunol. 2018;9:978.
35.Jain RK, Duda DG, Willett CG, et al. Biomarkers of response and resistance to antiangiogenic therapy. Nat Rev Clin Oncol. 2009;6:327-38.
36.Takahashi T, Kalka C, Masuda H, et al. Ischemia- and cytokine-induced mobilization of bone marrow-derived endothelial progenitor cells for neovascularization. Nat Med. 1999;5:434-8.
37.Kalka C, Masuda H, Takahashi T, et al. Vascular endothelial growth factor(165) gene transfer augments circulating endothelial progenitor cells in human subjects. Circ Res. 2000;86:1198-202.
38.Coleman RL, Duska LR, Ramirez PT, et al. Phase 1-2 study of docetaxel plus aflibercept in patients with recurrent ovarian, primary peritoneal, or fallopian tube cancer. Lancet Oncol. 2011;12:1109-17.
39.Gourley C, McCavigan A, Perren T, et al. Molecular subgroup of high-grade serous ovarian cancer (HGSOC) as a predictor of outcome following bevacizumab. J Clin Oncol. 2014;32(suppl):5502.
40.Lockhart AC, Rothenberg ML, Dupont J, et al. Phase I study of intravenous vascular endothelial growth factor trap, aflibercept, in patients with advanced solid tumors. J Clin Oncol. 2010;28:207-14.
41.Ng CS, Zhang Z, Lee SI, et al. CT perfusion as an early biomarker of treatment efficacy in advanced ovarian cancer: an ACRIN and GOG study. Clin Cancer Res. 2017;23:3684-91.