Cabazitaxel, a Taxane for Men With Hormone-Refractory Metastatic Prostate Cancer
Cabazitaxel is a microtubule inhibitor in the taxane class. It is made from a yew needle precursor using a semisynthetic process. It binds to free tubulin, which is used during mitosis to form two daughter cells.
Approved Drugs: Cabazitaxel (Jevtana)
Indications
Treatment of patients with hormone-refractory metastatic prostate cancer previously treated with a docetaxel (Taxotere)-containing regimen.
Mechanism of Action
Cabazitaxel is a microtubule inhibitor in the taxane class. It is made from a yew needle precursor using a semisynthetic process. It binds to free tubulin, which is used during mitosis to form two daughter cells. It promotes assembly of tubulin into stable microtubules while simultaneously inhibiting disassembly. This prevents mitosis, as well as other interphase cellular functions. The drug has activity in tumor cells sensitive and resistant to docetaxel.
Metabolism
Peak drug concentration following an IV dose given every 3 weeks is achieved at the end of the 1-hour drug infusion (Cmax). Binding to plasma proteins is 89%–92%, mainly to serum albumin and lipoproteins. The drug is extensively metabolized in the liver via the CYP3A4/5 isoenzymes and to a lesser extent by CYP2C8 (10%–20%). However, the potential for cabazitaxel to inhibit drugs that are substrates of CYP isoenzymes 3A4/5 or 2C8 is low.
No studies have been done evaluating drug interactions with CYP3A4 inhibitors or inducers, so concomitant administration of cabazitaxel with strong CYP inhibitors should be avoided. A three-compartment pharmacokinetic model is used to determine drug half-lives of 1) alpha, 4 minutes; 2) beta, 2 hours; and 3) gamma phase, 95 hours. About 20 metabolites are excreted in the feces (76%) and urine (3.7%), with 80% excreted within 2 weeks after drug administration. Because of a small role in drug excretion, patients with mild (creatinine clearance 50–80 mL/min) to moderate (creatinine clearance 30–50 mL/min) renal impairment can receive full drug dose. Drug should not be given to patients with hepatic impairment (total bilirubin ≥ ULN [upper limit of normal], or AST [aspartate aminotransferase] or ALT [alanine aminotransferase] ≥ 1.5 ULN).
Drug Administration
• Premedicate 30 minutes prior to drug dose with an antihistamine (eg, diphenhydramine at 25 mg), corticosteroid (eg, dexamethasone at 8 mg), and an H2 receptor antagonist (eg, ranitidine at 50 mg) to minimize risk of hypersensitivity reaction. In addition, an antiemetic should be given.
• 25 mg/m2 IV over 1 hour every 3 weeks, in combination with oral prednisone 10 mg PO daily throughout treatment; absolute neutrophil count (ANC) must be > 1,500 cells/mm3.
• Dose reductions to 20mg/m2 for
a) Prolonged grade 3 or higher neutropenia lasting for more than 1 week despite growth factor support: delay treatment until ANC > 1,500 cells/mm3 then reduce dose and give G-CSF for secondary prophylaxis.
b) Febrile neutropenia: delay treatment until improvement/resolution and ANC > 1,500 cells/mm3 then reduce dose and use G-CSF for secondary prophylaxis.
c) Grade 3 or higher diarrhea, despite antidiarrheal medication, fluid and electrolyte replacement: delay drug until improvement/resolution, then dose-reduce.
• Wear personal protective equipment when preparing and administering the drug.
• Drug preparation requires two dilutions. Drug comes as a 60 mg/1.5 mL vial. First, the drug is dissolved in the supplied diluent, which contains alcohol, delivering a solution of 10 mg/mL. Second, within 30 minutes of the first step, the ordered drug is asceptically removed and added to a 250-mL bag (non–PVC-containing) 0.9% sodium chloride or 5% dextrose solution, to deliver a final concentration between 0.10–0.26 mg/mL. If the ordered dose is > 65 mg,
use a larger infusion (non-PVC) bag to deliver a
maximum concentration of 0.26 mg/mL.
• Administer via non-PVC infusion sets, with a 0.22 micron in-line filter, within 7 hours of mixing when kept at ambient temperature, or within 23 hours if refrigerated. This timing allows for the 1-hour infusion time and completion of drug administration by
8 hours, and 24 hours respectively.
• Cabazitaxel drug contains polysorbate 80, which can cause the DEHP plasticizer to be drawn from PVC bag or tubing into the IV fluid, so that non-PVC containing bag and administration sets must be used. The diluent contains 13% ethanol in water, and may cause the patient to have flushing of the cheeks.
• Drug is contraindicated in patients with an ANC
≤ 1,500 cells/mm3, and patients who have a history of severe hypersensitivity reactions to cabazitaxel or to other drugs formulated with polysorbate 80 (eg, docetaxel).
• Hepatic impairment is likely to increase drug concentrations and increase toxicity. Drug should NOT be given to patients with hepatic impairment.
• Use caution in administering drug to patients with severe renal failure (creatinine clearance of < 30 mL/min) and patients with end-stage renal diseases.
• Severe hypersensitivity can occur, including generalized rash/erythema, hypotension, and bronchospasm. If this occurs, drug should be discontinued; pretreat as above, and if reactions occur, treat emergently (airway, breathing, circulation).
Patient Education
• This drug is used to stop the cancer cells from dividing and growing. You will need to take a steroid pill, prednisone, every day while receiving cabazitaxel. You need to take the prednisone pill with milk or food to prevent stomach irritation.
• You should not receive this drug if your white blood cell (neutrophil) count is too low, or if you are allergic to the drug or other medicines that contain polysorbate 80 (eg, docetaxel, RHOgam, and certain vaccines).
• Tell your doctor all the medicines you are taking as well as over-the-counter and herbal preparations. Also tell your doctor if you have had allergic reactions in the past, have kidney or liver problems, are over the age of 65, or have any other medical conditions. Do not start any new medicines until you tell your doctor about them.
• The drug has some drug interactions. The pharmacist, nurse, and doctor will review your medicines and let you know. Do not start any new medicine without talking to your doctor or nurse, including herbal preparations such as St. John’s wort.
• The medicine may cause an allergic reaction. You must tell your doctor or nurse right away if you get any of these problems during or after the drug infusion: rash or itching, skin redness, feeling dizzy or faint, breathing problems, chest or throat tightness, swelling of the face.
• The drug may increase your risk for infection due to low white blood counts, so it is important to tell your nurse or doctor right away if you get a fever (100.5 ºF or higher), or have signs or symptoms of infection (eg, burning when you pass your urine, coughing up colored sputum) or chills. The drug may also increase the risk of bleeding (due to low platelets), so it is important to avoid getting cuts or injuring yourself. Report right away any bleeding or unusual bruising. Your red blood cell counts may be low, causing you to feel tired. Try to alternate rest and activity so you don’t get too tired. Call your nurse or doctor if you get shortness of breath. In order to check whether your blood counts are low, you will have your blood tested frequently (once weekly during cycle 1, and prior to each cycle of treatment). It is very important that you come to have your blood counts checked as directed. If your blood counts get too low, and you get a fever, you must go to the hospital and receive antibiotics. Patients can die from this.
• You may need to have an injection of a medicine to help keep your white blood cells (neutrophils) high. Your doctor or nurse practitioner/physician assistant will check your blood counts and decide if you need this shot. If you have risk factors for getting a low blood count, you may start the treatment receiving this shot so that your blood counts do not get so low.
• The drug may cause nausea, vomiting, diarrhea, and/or loss of appetite. If nausea, vomiting, or diarrhea occur and do not stop after 24 hours with the medicines you are given, call your nurse or doctor right away. This may cause you to become dehydrated, and your blood pressure to fall. In some cases, it can cause the kidneys to stop working. It is important that you call your doctor or nurse, as you can receive IV fluids, electrolytes, and effective medicines to stop the nausea/vomiting and the diarrhea.
Drug Interactions
• Drugs that strongly induce the CYP3A system will decrease cabazitaxel plasma concentrations (phenytoin, carbamazepine, rifampin, rifabutin, rifapentin, phenobarbital, St. John’s wort); avoid coadministration.
• Drugs that strongly inhibit the CYP3A system will increase cabazitaxel plasma concentrations (ketoconazole, itraconazole, clarithromycin, atazanavir, indinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, voriconazole); avoid coadministration; use caution with drugs that are moderate CYP3A inhibitors.
Special Considerations
• Neutropenia, febrile neutropenia can occur, and deaths have been reported. Assess CBC/differential weekly during cycle 1, prior to each cycle, and give G-CSF as needed/ordered. Patients with high-risk features should have primary G-CSF prophylaxis for cycle 1 (65 years of age or older, poor performance status, previous febrile neutropenia, extensive prior RT, poor nutritional status, serious comorbidities).
• Nausea, vomiting, diarrhea may be severe, and deaths have been reported. Rehydrate and treat with antiemetics and antidiarrheals, especially in elderly patients.
• Renal failure may rarely occur and can be fatal. Identify early and treat aggressively.
• Elderly patients must be closely monitored as they have increased mortality from treatment side effects, such as febrile neutropenia. Other side effects with increased incidence are fatigue, asthenia, pyrexia, dizziness, UTI, and dehydration.
• Drug can cause fetal harm, so women of childbearing age should use effective contraception, and mothers should not breastfeed while receiving the drug.
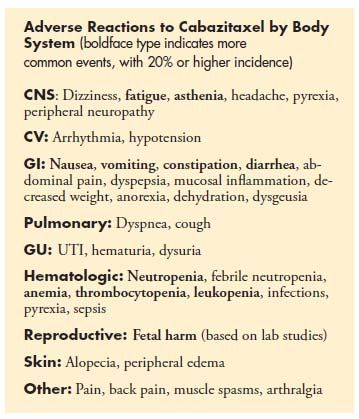
• Most common side effects occurring in > 10% of patients: neutropenia, anemia, thrombocytopenia, diarrhea, fatigue, nausea, vomiting, constipation, asthenia, abdominal pain, hematuria, back pain, anorexia, peripheral neuropathy,
pyrexia, dyspnea, dysgeusia, cough, arthralgia, alopecia.
Contraindications/Precautions
• Neutrophil count < 1,500 cells/mm3
• History of severe hypersensitivity to cabazitaxel or polysorbate 80
• Precautions
– Neutropenia can be fatal. Patients at risk for neutropenia should receive primary prophylaxis with G-CSF (age > 65, poor performance status, previous episodes of febrile neutropenia, extensive prior radiation ports, poor nutritional status, or other serious comorbidities). Monitor CBC/differential weekly during cycle 1, and before each treatment cycle, and adjust dose as needed. Use G-CSF as secondary
prophylaxis as needed.
– Hypersensitivity reactions (HSR) may occur. Administer premedications to minimize this risk. Discontinue drug if HSR occurs, and do not rechallenge the patient who has a severe HSR (eg, generalized rash/erythema, hypotension, bronchospasm).
– Nausea and vomiting, together with severe diarrhea with fluid and electrolyte imbalance may occur, and rarely can be fatal. Anticipate and monitor elderly patients or those at risk closely, and intervene early with aggressive rehydration, antidiarrheal or antiemetic therapy, as needed. Reduce dose in patients who
develop grade 3 or higher diarrhea.
– Renal failure may occur rarely, and was associated with sepsis, dehydration, or obstructive uropathy. Monitor patients with declining renal function closely, and treat underlying cause aggressively.
– Elderly patients are at greater risk for neutropenia, febrile neutropenia, as well as fatigue, asthenia, pyrexia, dizziness, UTI, and dehydration compared with younger patients. Monitor elderly patients closely and intervene early to manage symptoms.
– Use drug cautiously in patients with poor renal function (creatinine clearance < 30 mL/min), and patients with end-stage renal disease.
– Cabazitaxel has not been studied in patients with hepatic impairment. The drug should not be administered to patients with impaired hepatic function (total bilirubin ≥ ULN, or AST and/or ALT ≥ 1.5 ULN).
Prolaris in Practice: Guiding ADT Benefits, Clinical Application, and Expert Insights From ACRO 2025
April 15th 2025Steven E. Finkelstein, MD, DABR, FACRO discuses how Prolaris distinguishes itself from other genomic biomarker platforms by providing uniquely actionable clinical information that quantifies the absolute benefit of androgen deprivation therapy when added to radiation therapy, offering clinicians a more precise tool for personalizing prostate cancer treatment strategies.