Chemotherapy-Induced Peripheral Neuropathy
Chemotherapy-induced peripheral neuropathy (CIPN) is a common treatment-related side effect of several widely used drugs. Agents known to cause CIPN include platinum analogs, antitubulins, proteasome inhibitors, immunomodulatory agents, and some of the newer biologics.
Oncology (Williston Park). 30(3):240–244.

Table 1. Risk Factors and Medical Comorbidities Associated With Peripheral Neuropathy
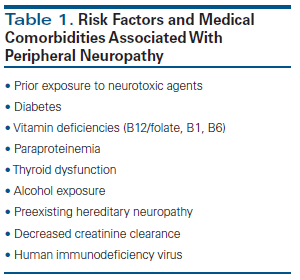
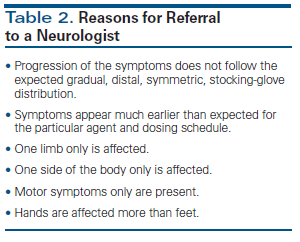
Table 2. Reasons for Referral to a Neurologist
Introduction
Chemotherapy-induced peripheral neuropathy (CIPN) is a common treatment-related side effect of several widely used drugs. Agents known to cause CIPN include platinum analogs, antitubulins (taxanes, vinca alkaloids, eribulin), proteasome inhibitors (bortezomib), immunomodulatory agents (thalidomide, lenalidomide, pomalidomide), and some of the newer biologics (alemtuzumab, ipilimumab, brentuximab).[1] In a recent meta-analysis of 31 studies of CIPN involving a total of 4,179 patients, the aggregate prevalence of CIPN was 48%. Within the first month after the patients completed chemotherapy, 68.1% had CIPN; the prevalence decreased to 30% after 6 months.[2] The reported proportion of patients affected by CIPN varies depending on the chemotherapy regimen administered, the duration of patient exposure to the neurotoxic agent(s), and the evaluation methods used.[3] For some patients, the side effects and deficits caused by CIPN are so severe that they impair daily function and diminish quality of life. CIPN can result in chemotherapy dose reductions or early treatment discontinuation, compromising effective cancer treatment and patient survival. Since cancer treatment advances have extended survival times for many patients, the long-term sequelae of CIPN have become increasingly important.
Presentation and Diagnosis
The classic clinical presentation is a symmetric, predominantly sensory, distal neuropathy (in a stocking-glove pattern). Common presenting symptoms are paresthesia (with positive symptoms including burning, tingling, and sharp pain), numbness (with negative symptoms including loss of sensation), and impaired balance. Occasionally, patients present with more prominent motor symptoms, autonomic involvement, or cranial neuropathies. The intensity and severity of the symptoms vary depending on the chemotherapeutic agent, the dosage and treatment schedule, the duration of therapy, coadministration of more than one known neurotoxic agent (eg, combination of carboplatin with paclitaxel), and comorbid conditions that predispose the peripheral nervous system to injury (Table 1).[4] The mechanisms of anticancer activity are usually well known and described for the specific chemotherapeutic agents used; however, their individual mechanisms of neurotoxicity may differ, making the onset and course of CIPN unpredictable.[5] There is great individual variability in the onset, severity, and duration of symptoms; recovery is often lengthy and frequently incomplete. With some chemotherapeutic agents, the patient’s symptoms continue to progress after treatment has ended; this so-called coasting phenomenon is observed with oxaliplatin, cisplatin, and vincristine.[6] Individual genetic variations or polymorphisms may explain the wide spectrum of vulnerability to CIPN from a given agent. Numerous genes have been investigated in an attempt to clarify this association, such as GSTP1, CYP2C8, and AGXT, but the findings are inconclusive.[7]
In practice, CIPN is graded based on subjective complaints from the patient and an examination by the oncologist. The most widely used tools to evaluate the degree of CIPN are questionnaires, either administered by healthcare professionals (such as the National Cancer Institute’s Common Terminology Criteria for Adverse Events grading scale) or completed by patients (such as the Functional Assessment of Cancer Therapy/Gynecologic Oncology Group–Neurotoxicity questionnaire). These tools are limited because they rely on the subjective report of symptoms. An important consideration is that healthcare providers and patients frequently have a different perception of CIPN severity.[1] This is especially important for patients who are engaged in professions or activities requiring intact sensory and motor functions, as well as fine control of the hands (eg, dentist, pianist, carpenter, jewelry maker) or feet (eg, professional driver).
Prevention and Treatment
There are no high-quality studies demonstrating effective prevention of CIPN using any agent. The latest guidelines from the American Society of Clinical Oncology (ASCO) acknowledge this limitation and recommend against offering any CIPN-preventive drug to patients undergoing neurotoxic cancer treatment.[8] Regarding treatment of CIPN, the ASCO guidelines state that clinicians may offer duloxetine to symptomatic patients[9] and should consider offering tricyclic antidepressants, gabapentin, or pregabalin to manage the positive symptoms associated with CIPN; however, these agents have no effect on the motor symptoms or the negative sensory symptoms. Patients should be informed of the limited scientific evidence of benefit from these anti-CIPN drugs, and of their potential harms and associated costs.[8]
Role of the Neurologist and ElectroDiagnostic Testing in Management of CIPN
Early and accurate diagnosis of CIPN is crucial, since it enables dose adjustment of chemotherapy to prevent worsening of peripheral neuropathy and possibly avert irreversible nerve damage. Prior to the initiation of neurotoxic chemotherapy, all patients should have laboratory testing to screen for diabetes (the hemoglobin A1c test), vitamin deficiencies (B12, B1), pyridoxine (B6) intoxication, and thyroid abnormalities, with correction of any underlying comorbidity. In addition, the treating physician should conduct a baseline neurologic examination, recording any sensory or motor abnormalities and documenting the patient’s deep tendon reflexes.[10] Loss of the Achilles tendon reflex is usually the first clinical sign of CIPN.
Notably, however, overdiagnosis of CIPN may compromise treatment with an otherwise beneficial chemotherapy regimen, negatively affecting cancer outcomes and survival. In a study of 55 breast cancer patients referred for electrodiagnostic studies due to symptoms suggesting possible taxane-related polyneuropathy, 33% had no electrophysiologic evidence of polyneuropathy or showed only focal entrapment neuropathy (carpal tunnel syndrome); 67% had a large fiber polyneuropathy.[11] Thus, neurologic evaluation can clarify when symptoms are unrelated to CIPN, allowing full oncologic treatment to continue.
Usually patients are referred to a neurologist only if symptoms of neuropathy persist for more than 6 months. In our opinion, a neurologist should be consulted early for patients with preexisting conditions or atypical presentations (Table 2). For patients with preexisting conditions, documentation of baseline neurologic deficits might prove invaluable if they develop neuropathic symptoms during cancer treatment. In addition, a careful neurologic examination of a patient with an atypical presentation should be enough to differentiate between CIPN and other entities (eg, cervical or lumbar radiculopathy, compression neuropathies). Nerve conduction studies (NCS) and an electromyogram (EMG) are well-tolerated electrophysiologic tests that are an invaluable complementary tool in the diagnostic evaluation of patients with suspected CIPN, especially when the timing and course of symptoms are unusual. NCS and EMG serve as an objective predictive measurement of the severity of peripheral nerve damage and therefore can be used to prognosticate neurologic recovery.[12]
The neurologist can also assist with treatment options. Despite the absence of strong evidence in favor of the available neuropathic medications, they may be helpful. In our practice, we frequently encounter patients for whom the available treatments failed, but often the doses were too low or inadequate time was allowed for the medication to take effect. Slow titration of gabapentin up to 600 mg three times a day is well tolerated and often provides moderate symptom relief. Alternatively, treatment with 30 mg of duloxetine daily for 1 week, followed by 60 mg daily, yields comparable symptom control. The neurologist will also be able to counsel the patient regarding expectations and limitations of the pharmacologic treatments. Patients should be offered physical or occupational therapy, and patient education should focus on lifestyle modifications to avoid falls and injury. Patients without laboratory-proven vitamin deficiencies should be reminded to avoid taking nutritional supplements, since they may worsen the neuropathy. Frequent neurologic examination should include reassessment of the need for symptomatic therapy.
Conclusion
Although CIPN is a common side effect of cancer treatment, physicians may not fully appreciate its impact on patients’ long-term quality of life.[13] Preexisting conditions should be taken into consideration prior to initiation of potentially neurotoxic agents. It is important that the treating physician collaborate closely with a neurologist in evaluating and managing high-risk patients. Symptom management, along with physical or occupational therapy, may benefit select patients.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Cavaletti G, Marmiroli P. Chemotherapy-induced peripheral neurotoxicity. Curr Opin Neurol. 2015;28:500-7.
2. Seretny M, Currie GL, Sena ES, et al. Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Pain. 2014;155:2461-70.
3. Cavaletti G, Zanna C. Current status and future prospects for the treatment of chemotherapy-induced neurotoxicity. Eur J Cancer. 2002;38:1832-7.
4. Kawakami K, Tunoda T, Takiguchi T, et al. Factors exacerbating peripheral neuropathy induced by paclitaxel plus carboplatin in non-small cell lung cancer. Oncol Res. 2012;20:179-85.
5. Cavaletti G. Chemotherapy-induced peripheral neurotoxicity (CIPN): what we need and what we know. J Peripher Nerv Syst. 2014;19:66-76.
6. Cavaletti G, Alberti P, Frigeni B, et al. Chemotherapy-induced neuropathy. Curr Treat Options Neurol. 2011;13:180-90.
7. Alberti P, Cavaletti G. Management of side effects in the personalized medicine era: chemotherapy-induced peripheral neuropathy. Methods Mol Biol. 2014;1175:301-22.
8. Hershman D, Lacchetti C, Dworkin R, et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2014;32:1941-67.
9. Smith EM, Pang H, Cirrincione C, et al. Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. JAMA. 2013;309:1359-67.
10. Hausheer F, Schilsky R, Bain S, et al. Diagnosis, management, and evaluation of chemotherapy-induced peripheral neuropathy. Semin Oncol. 2006;33:15-49.
11. Chen X, Stubblefield M, Custodio C, et al. Electrophysiological features of taxane-induced polyneuropathy in patients with breast cancer. J Clin Neurophysiol. 2013;30:199-203.
12. Kaley T, DeAngelis LM. Treatment of chemotherapy-induced peripheral neuropathy. Br J Haematol. 2009;145:3-14.
13. Park S, Goldstein D, Krishnan A. Chemotherapy-induced peripheral neurotoxicity: a critical analysis. CA Cancer J Clin. 2013;63:419-37.

Late Hepatic Recurrence From Granulosa Cell Tumor: A Case Report
Granulosa cell tumors exhibit late recurrence and rare hepatic metastasis, emphasizing the need for lifelong surveillance in affected patients.