Custirsen, an Antisense Oligonucleotide, May Enhance Docetaxel Efficacy in Hormone-Refractory Prostate Cancer
CHICAGO-The combination of custir-sen sodium (OGX-011, OncoGenex Technologies Inc), an investigational agent, with docetaxel (Taxotere) or mitoxantrone has acceptable toxicity in patients with hormone-refractory prostate cancer who have experienced a failure of first-line docetaxel-based chemotherapy, investigators reported at ASCO 2008 (abstract 5002). Efficacy outcomes were somewhat better with the custirsen/docetaxel combination.
ABSTRACT: Custirsen is designed to inhibit clusterin, a protein associated with reduced apoptosis and chemotherapy resistance in prostate cancer.
CHICAGO-The combination of custir-sen sodium (OGX-011, OncoGenex Technologies Inc), an investigational agent, with docetaxel (Taxotere) or mitoxantrone has acceptable toxicity in patients with hormone-refractory prostate cancer who have experienced a failure of first-line docetaxel-based chemotherapy, investigators reported at ASCO 2008 (abstract 5002). Efficacy outcomes were somewhat better with the custirsen/docetaxel combination.

The protein clusterin inhibits treatment-induced apoptosis and has been associated with treatment resistance in prostate cancer, said lead investigator Fred Saad, MD.
“Custirsen is a second-generation antisense oligonucleotide designed to reduce clusterin production,” he explained. “It facilitates tumor cell death by lowering apoptotic threshold and sensitizing cancer cells to a variety of anticancer therapies.”
Participants in the open-label, randomized, noncomparative phase II trial were men with metastatic, hormone-refractory prostate cancer who had received at least two cycles of a docetaxel-based first-line regimen and had progressed while on this treatment or within 6 months afterward. They were given loading doses of custirsen followed by weekly custirsen plus docetaxel every 3 weeks and daily prednisone (CDP), or by weekly custirsen plus mitoxantrone every 3 weeks and daily prednisone (CMP).
Median follow-up of the trial population was 17.2 months, said Dr. Saad, a urologic surgeon at the University of Montreal. Results were based on 20 patients in the CDP arm and 22 in the CMP arm. Some 50% in the former arm and 36% in the latter arm received all nine planned cycles of therapy.
PSA Levels Fall
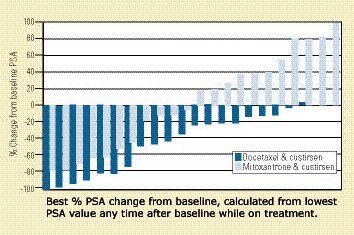
In the CDP group, all but one patient had a reduction from baseline in PSA levels, with values falling by 5% to 100%. In the CMP arm, half of patients had a reduction, with values falling by 5% to 80% (see Figure). Analyses of the entire trial population showed that median survival was significantly longer for patients whose PSA levels fell by more than 30% (19.4 vs 9.7 months).
Median progression-free survival was 7.2 months with CDP and 4.2 months with CMP, and corresponding median overall survival was 14.7 and 11.4 months.
In the entire population, overall survival was significantly longer in patients whose mean postbaseline clusterin level was 55 µg/mL or lower (14.7 vs 6.1 months, P = .002), suggesting that levels of the protein predict survival in this context, Dr. Saad observed.
Pain Response
Among patients with baseline pain, 61% in the CDP arm had a pain response, compared with 46% in the CMP arm.
“What’s very impressive is that 13 out of 14 pain responses actually occurred within the first cycle, and several investigators reported that patients were having pain responses even prior to the first injection of chemotherapy, so basically only the custirsen loading phase was leading to diminished pain,” Dr. Saad commented.
All of the patients who had been taking level 2 or 3 opioids no longer needed any opioids. The median duration of pain response was about 6 months.v
Adverse Events
Grade 3 or higher adverse events occurred in 60% of the CDP patients and 68% of the CMP patients. Most of these events were suspected to be cancer or chemotherapy related, with few suspected to be related to the antisense treatment, Dr. Saad noted. CMP patients had higher rates of grade 3-4 neutropenia (19% vs 10%), anemia (14% vs 0%), elevated liver enzymes (5% vs 0%), and hyponatremia (14% vs 0%).
‘Beyond Our Expectations’
Dr. Saad noted that despite the previous treatment with docetaxel, patients were able to receive a median of eight more cycles of CDP and six more cycles of CMP with acceptable toxicity.
“This went beyond our expectations when we had designed this study,” he commented. Given the encouraging findings, he said, “phase III studies are presently being planned utilizing chemotherapy plus custirsen as second-line therapy in metastatic hormone-refractory prostate cancer.”
Vantage Point
‘Impressive’ Pain results; Tolerability Questioned

Dr. Kelly, of the Yale Cancer Center, cautioned that at least some patients defined as being resistant to docetaxel by the trial’s criteria may still be sensitive to this drug.
The high rates of grade 3-4 adverse events with both CDP and CMP are concerning, he further commented, and “this leads us to question how tolerable these regimens would be when given for prolonged periods of time.” On the other hand, he described the trial’s pain response rates as impressive.
Comparing the results with those from another second-line study in this population (Rosenberg JE et al: Cancer 110:556-563, 2007), Dr. Kelly noted that the rate of a PSA response (reduction by at least half) was better with CDP than with ixabepilone (Ixempra) (40% vs 17%) and slightly better with CMP than with mitoxantrone/prednisone (27% vs 20%). Median overall survival was longer with the custirsen-containing regimens as well-14.7 (CDP) vs 10.4 months and 11.4 (CMP) vs 9.8 months. However, he added that for both trials, “it’s difficult to assess clinical activity without a control arm.”