CYP2D6 Testing in Breast Cancer: Ready for Prime Time?
This article will review and summarize the current data regarding the influence of the major cytochrome P450 2D6 (CYP2D6) genotypes and CYP2D6 inhibitors on tamoxifen metabolism and clinical efficacy. We will discuss the clinical relevance and limitations of this data and how to best incorporate our current understanding of CYP2D6 genotyping into our clinical practice and discussions with patients.
Despite recent advances in hormonal therapy for breast cancer, tamoxifen remains a major therapeutic option, with indications ranging from primary prevention to metastatic disease. Understanding the variation in response to tamoxifen may significantly improve our ability to personalize cancer care and maximize therapeutic efficacy. One area of particular interest is the impact of cytochrome P450 CYP2D6 genetic polymorphisms on tamoxifen metabolism. Tamoxifen is considered a prodrug, whose efficacy may be dependent on active metabolites, including endoxifen. Patients with reduced CYP2D6 enzymatic activity tend to have lower endoxifen levels, but clinical relevance of reduced endoxifen levels remains to be determined. Several small to moderately sized retrospective studies have suggested an intriguing association between poor metabolizer status and increased disease recurrence. However, these data are limited by sample size and methodologic challenges, including the inability to adjust for major prognostic and confounding factors. Several subsequent studies have failed to find an association or found improved outcomes among reduced CYP2D6 metabolizers. Therefore, current findings are conflicting and should be considered preliminary. Nevertheless, the CYP2D6 test is commercially available, making clinical use possible even as evidence in this area is still evolving. More definitive clinical research is needed before routine CYP2D6 testing can be recommended and considered standard of care. Anticipated data from retrospective analysis of large adjuvant randomized trials of tamoxifen should help address the clinical utility of CYP2D6 testing.
Despite recent advances in hormonal therapy for breast cancer, tamoxifen, a selective estrogen receptor modulator first approved in the 1970s, remains one of the most effective interventions in our therapeutic armamentarium, with indications ranging from prevention of breast cancer to treatment of metastatic disease. However, for reasons that remain incompletely understood, not all patients with endocrine receptor–positive breast cancer will respond to or benefit from tamoxifen. There are now multiple alternative endocrine therapies available, with variable efficacy and toxicity profiles, making it increasingly important to understand the optimal endocrine strategy for an individual patient.
One area of particular interest is the rapidly evolving evidence in the field of pharmacogenetics, evaluating the association between genetic differences in drug metabolism and patient outcomes. Recent studies have suggested that we may soon be able to rationally select drugs for specific patients based on differing drug metabolism in addition to other clinical factors. This article will review and summarize the current data regarding the influence of the major cytochrome P450 2D6 (CYP2D6) genotypes and CYP2D6 inhibitors on tamoxifen metabolism and clinical efficacy. We will discuss the clinical relevance and limitations of this data and how to best incorporate our current understanding of CYP2D6 genotyping into our clinical practice and discussions with patients.
Tamoxifen
The majority of breast cancers are dependent on estrogen, and estrogen deprivation has been recognized as an effective treatment for breast cancer for over 100 years, following Beatson’s initial publication on the role of oophorectomy in advanced disease.[1] Our ability to provide endocrine therapy for patients advanced markedly with the approval of tamoxifen by the US Food and Drug Administration (FDA) in 1977 for the treatment of postmenopausal women with metastatic breast cancer.[2] In 1986, tamoxifen gained FDA approval for adjuvant therapy in postmenopausal node-positive women, and the drug has subsequently been proven effective in hormone receptor–positive premenopausal and node-negative breast cancer patients,[3] breast cancer prevention,[4] ductal carcinoma in situ (DCIS),[5] and male breast cancer.[6] Among estrogen receptor (ER)-positive breast cancers, adjuvant tamoxifen reduces the relative recurrence rate by over 40% and breast cancer mortality by approximately one-third.[3] Tamoxifen remains the only FDA-approved hormonal agent for the treatment of premenopausal women, and DCIS.
Recent study of genetic predictors of recurrence risk and response to therapy reminds us that tamoxifen alone is a highly effective drug for early-stage breast cancer, conveying a sufficiently low risk of recurrence that chemotherapy can be avoided for many patients.[7] While in postmenopausal women, an adjuvant strategy involving aromatase inhibitors (AIs), either alone or in sequence with tamoxifen, is now preferred for most patients, the absolute difference in disease-free survival is on the order of 3% to 4%, with no clear improvement in overall survival.[8] The AI side-effect profile is preferable for many patients, without the risks of thrombosis and uterine malignancy observed with tamoxifen. However, some patients with severe joint symptoms or refractory osteoporosis may not be able to tolerate an AI.[9-11] Further, the higher cost for AIs compared to tamoxifen may be a treatment barrier for some patients. Tamoxifen remains a standard part of treatment for many patients with breast cancer. If the factors impacting response could be identified, we might be able to obtain even greater results for some patients on tamoxifen, and use alternative endocrine therapies for other patients. Many factors, ranging from tumor biology to adherence, likely play a role in response to tamoxifen, but recently it has become apparent that understanding differences in metabolism may provide clues that can help optimize management of endocrine-responsive breast cancer.
Tamoxifen Metabolic Pathway and Active Metabolites: Endoxifen and 4-Hydroxy-Tamoxifen
TABLE 1
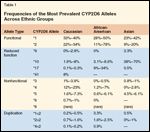
Frequencies of the Most Prevalent CYP2D6 Alleles Across Ethnic Groups
Once orally absorbed, tamoxifen is initially metabolized primarily by two hepatic enzymes in the cytochrome P450 family, CYP2D6 and CYP3A4/5. As demonstrated in Figure 1, the major metabolic pathway involves initial conversion of tamoxifen to N-desmethyl-tamoxifen via CYP3A4/5, followed by conversion of N-desmethyl-tamoxifen to endoxifen, via CYP2D6. In addition, some tamoxifen is initially metabolized by CYP2D6 to the active metabolite 4-hydroxy-tamoxifen, which in turn is either degraded or converted by CYP3A4/5 to endoxifen. Tamoxifen has weak estrogen receptor binding and is considered a prodrug. Endoxifen and 4-hydroxy-tamoxifen are much more potent blockers of the estrogen receptor than tamoxifen, with over 100 times stronger binding affinity. Furthermore, endoxifen reaches several-fold higher concentrations than 4-hydroxy-tamoxifen, suggesting that it may be the most important active tamoxifen metabolite.[12]
FIGURE 1
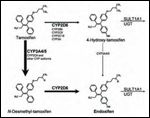
Tamoxifen Metabolism and Its Metabolites
Natural genetic variation in alleles for the CYP2D6 gene that lead to marked differences in CYP2D6 enzymatic activity were recognized as early as the 1970s, and variation in metabolism has been determined for a number of commonly used drugs.[13] Over 80 different CYP2D6 alleles have now been identified and can be categorized as nonfunctional alleles (also called null alleles, mainly *3, *4, *5, *6, and *8), reduced function alleles (mainly *9, *10, *17, and *41), and wild-type (wt) alleles (mainly *1, and *2), with increased enzymatic functioning (Table 1).[14-16] Allelic frequency varies among ethnic groups (Table 1), with the nonfunctional allele CYP2D6*4 being most prevalent in Caucasians, and the reduced-functioning allele CYP2D6*10 most common among Asian populations.[14,16] Based on allele combinations, (or allele duplication) patients can be classified into four major genotypes: (1) poor metabolizers (PM)-homozygous for null alleles; (2) intermediate metabolizers (IM)-heterozygous for null or partially functional alleles; (3) extensive metabolizers (EM)-homozygous for wildtype alleles; and (4) ultrarapid metabolizers (UM)-carrying more than two CYP2D6 copies in their genome. Among Caucasian populations, the prevalence of genotypes with reduced CYP2D6 function is estimated to be roughly 5% to 10% for PM.[17]
Effect of CYP2D6 Genotype and CYP2D6 Inhibitors on Endoxifen Levels
TABLE 2
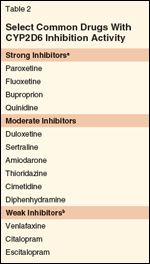
Select Common Drugs With CYP2D6 Inhibition Activity
CYP2D6 enzymatic activity can be substantially reduced not only by the presence of various polymorphisms, but also due to intake of many common drugs. There are numerous drugs that act as strong or moderate inhibitors of the CYP2D6 enzyme. Among the commonly used strong CYP2D6 inhibitors are fluoxetine, paroxetine, buproprion, and quinidine, whereas commonly used moderate CYP2D6 inhibitors are sertraline, duloxetine, diphenhydramine, trazodone, cimetidine, and amiodarone (Table 2). Further helpful information on CYP2D6 inhibitors and other drug interactions can be found at the website, www.drug-interactions.com. The impact of the selective serotonin reuptake inhibitors (SSRIs) and selective noradrenergic reuptake inhibitors (SNRI) on CYP2D6 is highly relevant in breast cancer patients, given the efficacy in control of hot flashes,[18-20] and depression.[21]
In an intriguing pilot study, the strong CYP2D6 inhibitor paroxetine was found to significantly reduce endoxifen levels in the plasma of 12 breast cancer patients receiving adjuvant tamoxifen therapy. Average endoxifen plasma levels decreased significantly after 4 weeks of concomitant paroxetine therapy, but levels of tamoxifen and other major metabolites did not change.[22] A follow-up study confirmed these findings in 80 newly diagnosed breast cancer patients on tamoxifen therapy, reporting that among women with homozygous wild-type CYP2D6 genotype, treatment with paroxetine yielded low endoxifen levels consistent with levels in poor metabolizers without paroxetine.[23] In addition, among the 56 patients on tamoxifen without concomitant inhibitor use, poor or intermediate metabolizers had significantly lower endoxifen levels compared to extensive metabolizers.[23]
Of note, overall correlation between CYP2D6 genotype and endoxifen is relatively poor and there remains great interindividual variability in concentrations of tamoxifen and its metabolites, which is not explained by the various genotypes.[24,25] The clinical relevance of lower endoxifen levels also remains to be determined. Dose-setting and receptor-binding studies have suggested that tamoxifen metabolites may reach sufficient levels for full therapeutic effect irrespective of CYP2D6 activity level.[25]
Impact of CYP2D6 Genotype on Tamoxifen Efficacy and Patient Outcomes
Positive Association Between CYP2D6 Genotype and Poor Patient Outcomes
TABLE 3

Studies Assessing Association of CYP2D6 Genotype and Clinical Outcome in Breast Cancer Patients on Adjuvant Tamoxifen Therapy
Given endoxifen’s high antiestrogen activity, its elevated concentration in comparison to other active tamoxifen metabolites, and the influence of CYP2D6 activity on endoxifen levels, there has been interest in evaluating the impact of CYP2D6 genotype on clinical outcomes for patients on tamoxifen (Table 3).
Among the first attempts to evaluate the clinical impact of CYP2D6 genotype was an initial report by a collaboration of investigators from the Consortium on Breast Cancer Pharmacogenetics (COBRA),[17] and the North Central Cancer Treatment Group (NCCTG)/Mayo Clinic, studying 223 of 256 ER-positive postmenopausal women with early-stage breast cancers, randomized to 20 mg tamoxifen therapy for 5 years without chemotherapy within a randomized trial.[26] Only the CYP2D6 *4 null allele was determined from the archival tumor specimens,[17] but this genotype accounts for the majority of poor metabolizers in Caucasian women. In univariate analysis, women homozygous for this nonfunctional allele (*4/*4) had significantly worse disease-free survival and recurrence-free time compared to women heterozygous for this variant allele (*4/wildtype) or women without this allele. However, in multivariate analysis after adjustment for other prognostic factors, statistical significance of these findings was lost.
In the follow-up study utilizing 171 patients of the same patient population, Goetz et al refined their findings by determining the presence of CYP2D6 inhibitor use in these patients.[27] In multivariate analysis after adjusting for tumor size and nodal status, patients with decreased CYP2D6 metabolism, determined by either genotype or the use of a moderate or strong CYP2D6 inhibitor, resulted in a significantly reduced relapse-free survival (RFS; hazard ratio [HR] = 1.74; P = .02), and shorter time to recurrence (HR = 1.91; P = .03), but overall survival (OS) did not differ significantly (HR = 1.34; P = .22).[27] In a recently presented long-term update of this study analyzing additional CYP2D6 variant alleles (*3, *4, *6, *10, *17, *41), poor metabolizers continued to have reduced RFS (HR = 2.0; P = .02) and time to recurrence (HR = 4.0; P = .001) after adjusting for tumor size and nodal status, while intermediate metabolizers had nonsignificant reductions in these outcomes.[28]
Comparable results were seen in a German study, retrospectively genotyping archived tissue from 206 pre- and postmenopausal women undergoing adjuvant tamoxifen therapy alone, and 280 control patients without tamoxifen.[29] After assessing various genotypes (*4, *5, *10, *41) and adjusting results for tumor size and nodal status, women with the presence of at least one nonfunctional allele did experience significantly reduced event-free survival (EFS; HR = 1.89; P = .02) and RFS (HR = 2.24; P = .02), but not OS. As expected, no significant association between CYP2D6 genotype and outcomes was seen among control patients without tamoxifen.
Similar results have been reported in two small cohort studies in Asian women on adjuvant tamoxifen, examining the most frequent reduced-function allele CYP2D6*10.[30,31] Most recently, a small nested case-control study (67 cases; 55 controls) utilizing matched samples from the recent Austrian Breast Cancer Study Group (ABCSG) trial 8 presented at the 2008 San Antonio Breast Cancer Symposium, revealed significantly increased risk of distant breast cancer recurrence among poor CYP2D6 metabolizers (recurrence risk [RR] = 3.83; P = .02) but not among intermediate metabolizers (RR = 0.87; P = .69) in patients treated with tamoxifen. This difference in recurrence risk for poor metabolizers was not seen among patients switched to anastrozole (Arimidex) after 2 years of tamoxifen.[32] Suggestive results are also seen in a very small Spanish study,[33] and two small nonadjuvant cohorts.[34,35] Reduced CYP2D6 functioning was more likely to be present among 211 Korean patients with metastatic breast cancer whose cancer did not respond to tamoxifen,[34] and among the 47 Italian women who developed breast cancer, while participating in a tamoxifen cancer prevention trial.[35]
Absent or Opposite Association Between CYP2D6 Genotype and Poor Patient Outcomes
The results above stand in contrast to several moderately sized studies that suggested improved clinical outcomes in conjunction with reduced CYP2D6 enzymatic activity (Table 3). Wegman et al retrospectively analyzed samples from a Swedish trial that had randomized 679 postmenopausal women in a 2 × 2 factorial design to compare 2 years of adjuvant tamoxifen therapy (40 mg) to no endocrine therapy and a second randomization to compare the addition of chemotherapy vs radiation therapy.[36] They were able to assess additional genotypes (*1, *4) in 226 of these women (112 with tamoxifen and 114 without). Comparing poor metabolizer ER-positive patients on tamoxifen vs those not receiving tamoxifen, it was found that patients possessing at least one CYP2D6*4 allele had a significantly reduced distant recurrence rate when randomized to tamoxifen compared to those not randomized to tamoxifen (RR = 0.28; P = .009). No such difference was found among extensive metabolizer patients (RR = 0.91; P = .75), suggesting that tamoxifen is still an active drug for patients with poor CYP2D6 metabolism.
The same investigators performed a subsequent larger retrospective tumor tissue analysis of 677 postmenopausal women status post either 20 or 40 mg of adjuvant tamoxifen therapy for 2 or 5 years. Poor metabolizers (*4 homozygotes), and intermediate metabolizers (*4 heterozygotes) were significantly associated with improved RFS (P = .05) and (P = .04), respectively, compared to extensive metabolizers in univariate analysis. After adjusting for tumor stage, size, and nodal status, these differences did not quite reach statistical significance (P = .055). Similarly, examining tumor bank tissue from the Arkansas Cancer Research Center from pre- and postmenopausal women with (n = 162) or without (n = 175) tamoxifen therapy, Nowell and colleagues found a nonsignificant trend toward improved RFS and OS among tamoxifen-treated women with at least one nonfunctional allele (*4) after adjusting for age, race, stage, ER and progesterone receptor status.[37] Most recently, Okishiro et al found that among 173 Asian women on adjuvant tamoxifen, reduced CYP2D6 metabolism was not associated with recurrence-free survival, nor did it affect cholesterol levels, bone mineral density, or uterine thickness.[38]
These diametrically opposed study results have been attributed to differences in study design including varying length and dose of tamoxifen, inclusion of ER-negative patients, and variable use of chemotherapy. However, important methodologic limitations can be found among all described studies (Table 3), which can only be resolved by examining the association of CYP2D6 genotype and patient outcomes in large randomized controlled tamoxifen trials.
Impact of CYP2D6 Inhibitors on Patient Outcomes
While previously reported studies have revealed intriguing results regarding the influence of CYP2D6 inhibitors on changes in endoxifen levels, only recently have two studies sought to evaluate the influence of CYP2D6 inhibitors on actual patient clinical outcomes. Preliminary results of these two large retrospective studies were presented at the 2009 annual meeting of the American Society of Clinical Oncology, providing conflicting results. Aubert et al evaluated claims data from breast cancer patients receiving tamoxifen therapy. In univariate analysis, they found a significant reduction in EFS among patients with concurrent use of a moderate or strong CYP26D inhibitor compared to patients not receiving such agents.[39] No such effect was seen among patients using a weak CYP26D inhibitor. Of note, event-free survival in this study was approximated based on ICD-9 and CPT-4 claims codes, including procedures codes (eg, lumpectomy, mastectomy, lymph node dissection) and hospitalization codes to estimate breast cancer recurrence.
A second study analyzed the impact of CYP2D6 inhibitors and tamoxifen adherence in over 1,900 stage I–III breast cancer patients from the Dutch Medical Register (LMR) and linked the data to large pharmacy data repositories.[40] In this study, patients on tamoxifen and a concomitant moderate or strong CYP2D6 inhibitor had the same EFS (distant metastases, locoregional recurrence, second primary breast cancer) as patients without inhibitor use (HR = 0.95; P = .73). However, it was observed that reduced tamoxifen adherence below 90% correlated with reduced EFS.[40] Of note, both of these retrospective administrative database studies had not controlled for major confounding factors including CYP2D6 genotype status.[39,40] While no definitive conclusions can be drawn in regard to CYP2D6 inhibitor use and breast cancer outcomes, both studies agree that weak CYP26D inhibitors appear safe in tamoxifen-treated patients.
Impact of CYP2D6 Genotype on Hot Flashes and Tamoxifen Adherence
While we understand the absence of side effects to be a good thing, several studies have addressed the question of whether, in the case of tamoxifen, hot flashes are a sign of high drug metabolism and thus potentially a marker of drug efficacy. In the study cited above by Goetz and colleagues, women with the (*4/*4) genotype appeared to have lower rates of hot flashes.[17] This has been identified in subsequent studies and appears to also correlate with lower endoxifen levels among poor metabolizers.[22,23,41]
A recent report by Henry and colleagues suggests a need for caution in assuming that absence of hot flashes is indicative of a PM CYP2D6 genotype. In a study of close to 300 women, they detected a trend for correlation between severity of hot flashes and PM status, but there was large variation within groups and, surprisingly, EM and PM patients had similarly lower levels of hot flashes compared to IM patients.[42] This finding may be explained in part by the possibility that patients with greater side effects may have higher levels of tamoxifen metabolism but also lower tamoxifen adherence.[43] Lack of adherence may well minimize the potential differences between extensive and poor metabolizers and is another reason for caution in interpretation of the current retrospective CYP2D6 genotype studies.[43]
What Is the Current Strength of the Evidence and Clinical Utility of CYP2D6 Testing?
Having established that there are genetic differences in metabolism of tamoxifen as well as concurrent medications that can impact metabolism, and that these differences may correlate with breast cancer outcomes, the question of whether to test all patients who are on tamoxifen or who are candidates for tamoxifen therapy must be addressed. Key considerations in addressing this question are:
(1) How solid is the evidence for differences in metabolism contributing to differences in breast cancer outcomes?
(2) How will we use genotype information if it is obtained?
(3) Are there proven alternative therapies for patients who are poor or intermediate metabolizers?
(4) In the face of evolving evidence, what role should physician discretion and patient autonomy play in the decision to test or not test for CYP2D6 genotype?
FIGURE 2

Summary of Evidence Regarding the Potential Impact of CYP2D6 or CYP2D6 Inhibitors on Breast Cancer Outcomes With Tamoxifen Therapy
Not all of these questions have easy answers, nor is there likely to be consensus among all physicians or patients on these issues at this time. The current level of evidence of the impact of tamoxifen metabolism on breast cancer outcomes could best be described as preliminary and hypothesis-generating in nature (Figure 2). To date, all the evidence for correlation between genotype and outcomes among patients on adjuvant tamoxifen therapy comes from retrospective analyses of small to moderately sized cohort studies or tumor registries and one nested case-control study drawn from a randomized controlled trial. Similar to early-phase data from therapeutic trials, the chance for false-positive or biased results among retrospective analyses of predictive factors remains high, particularly in studies with limited ability to evaluate and adjust for major prognostic and confounding factors (eg, HER2 status, estrogen receptor status, lymph node status, tumor size and grade, age, chemotherapy and radiation therapy, concomitant CYP2D6 inhibitor use, and tamoxifen adherence).
In addition, current data are contradictory, with several studies finding no clear association between CYP2D6 genotype and patient outcomes and at least two studies suggesting that reduced tamoxifen metabolism may correlate with a decreased-not increased-risk of recurrence (Table 3). Few studies evaluated control populations to ensure the predictive nature of their findings specific to tamoxifen. All studies limited genotyping to a subgroup of patients and a subset of CYP2D6 polymorphisms. Given the retrospective nature of the data in this field thus far, the potential effect of publication bias cannot be excluded, favoring small positive studies compared to small negative studies.
While the evidence in this area is still evolving, the association between CYP2D6 genotype or endoxifen levels and patient outcomes has yet to be clearly demonstrated in a prospective study, in which all relevant factors can be recorded and evaluated. Evidence from the retrospective analysis of some of the large randomized trials of tamoxifen vs aromatase inhibitors is forthcoming, and prospective studies are underway that should provide more definitive data in this area.
Should Patients Considering or Taking Tamoxifen Be Routinely Tested for CYP2D6 Genotype?
REFERENCE GUIDE
Therapeutic Agents
Mentioned in This Article
Amiodarone
Anastrozole (Arimidex)
Buproprion
Cimetidine
Citalopram
Diphenhydramine
Duloxetine
Fluoxetine
Paroxetine
Quinidine
Sertraline
Tamoxifen
Trazodone
Venlafaxine
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
The value of testing would presumably be to identify poor metabolism patients and to treat them with an alternative to the current tamoxifen regimen. Given the conflicting results, the lack of definitive trials, and the potential for significant bias in currently available studies, CYP2D6 testing should not yet be part of routine practice, especially in settings where tamoxifen is the only well established therapy, or alternative therapies may convey additional toxicity without clear demonstration of benefit. In addition, we must contend with data suggesting that poor metabolizers have a better outcome on tamoxifen than placebo, and some data even suggesting superior outcomes for patients with lower levels of tamoxifen metabolism. However, despite the uncertainties in this area, CYP2D6 testing may be appropriate for select women with an appropriate alternative standard treatment option and a comparable side-effect profile.
For postmenopausal patients, an aromatase inhibitor is a clear alternative, and some models suggest that the benefits of AI therapy may be confined to patients with low tamoxifen metabolism,[44] but there are no data directly addressing this question from randomized trials. Many postmenopausal patients will be treated with AI alone, but in those for whom tamoxifen is considered, testing is a reasonable option. In the setting of an appropriate alternative, CYP2D6 testing and even changes in management based on unconfirmed CYP2D6 genetic data is unlikely to do harm.
For premenopausal patients, the issue is more complex given the additional side effects and potential for long-term adverse events that may be conveyed with ovarian function suppression. It is possible that testing will lead to management changes that will improve outcomes, if definitive trials clarify the importance of the CYP2D6 genotype. However, it is also possible that patients may be harmed through testing if a proven treatment, such as tamoxifen, is abandoned in favor of unproven or more toxic strategies.
Should We Avoid Strong to Moderate CYP2D6 Inhibitors Concurrent With Tamoxifen?
While studies looking at the clinical impact of CYP2D6 inhibitors are limited and also conflicting, it currently seems prudent to avoid strong to moderate CYPD6 inhibitors for patients receiving tamoxifen. Especially in cases where there are effective alternatives such as venlafaxine or citalopram for hot flashes or depression, it seems reasonable to err on the side of patient safety, without risking potential drug interactions that may affect outcomes.
Should Physicians Who Do Not Advocate CYP2D6 Testing Inform Patients About Its Availability?
One thorny question is whether, in the face of uncertainly, patients should be informed of the availability of CYP2D6 testing and of the controversy in this area. We are in an era of rapidly emerging molecular information in both pharmacogenetics, genomic predictors of prognosis and response to therapy, and biomarkers of response. Increasingly, tests are becoming available before they are validated and before we know how best to use them in clinical practice or how differences in management will change outcomes.
There is currently no consensus on when information on novel molecular tests should be shared with patients, and debates over these issues are just beginning. Similar to early-phase data or other nonstandard practice in the adjuvant setting, physicians may or may not routinely discuss the availability of CYP2D6 testing. Physicians should be prepared to discuss the emerging evidence with inquiring patients, including the limitations of current evidence in this area. Given the uncertainties in this area, any management decisions should be based on the individual patient’s risk, preferences, alternatives, and the best available evidence at the time.
Conclusions
While personalizing care through pharmacogenetic testing lies clearly in our future and CYP2D6-guided tamoxifen therapy will hopefully be among the first settings in oncology for this to take place, evidence in this area remains preliminary and evolving, despite promising early results. More clinical research is needed before we can recommend routine CYP2D6 testing and we can rationally and safely use this test to guide practice. We hope to have data in the near future based on retrospective analyses from several of the large adjuvant tamoxifen randomized trials that will begin to clarify the association between metabolizer status and outcomes for patients on tamoxifen.
Financial Disclosure: The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article. Dr. Kuderer is supported by a grant from the National Cancer Institute (NCI 5T32 CA009307-30). Dr. Peppercorn is supported by the American Society of Clinical Oncology, Breast Cancer Research Foundation, and the Greenwall Foundation.
References:
1. Beatson G: On the treatment of inoperable cases of carcinoma of the mammary: Suggestions for a new method of treatment, with illustrative cases. Lancet 2:104-107, 1896.
2. Osborne CK: Tamoxifen in the treatment of breast cancer. N Engl J Med 339:1609-1618, 1998.
3. Early Breast Cancer Trialists’ Collaborative Group: Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: An overview of the randomised trials. Lancet 365:1687-1717, 2005.
4. Fisher B, Costantino JP, Wickerham DL, et al: Tamoxifen for prevention of breast cancer: Report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 90:1371-1388, 1998.
5. Fisher B, Dignam J, Wolmark N, et al: Tamoxifen in treatment of intraductal breast cancer: National Surgical Adjuvant Breast and Bowel Project B-24 randomised controlled trial. Lancet 353:1993-2000, 1999.
6. Ribeiro G, Swindell R: Adjuvant tamoxifen for male breast cancer (MBC). Br J Cancer 65:252-254, 1992.
7. Paik S, Shak S, Tang G, et al: A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 351:2817-2826, 2004.
8. Ingle JN, Dowsett M, Cuzick J, et al: Aromatase inhibitors versus tamoxifen as adjuvant therapy for postmenopausal women with estrogen receptor positive breast cancer: Meta-analyses of randomized trials of monotherapy and switching strategies (abstract 12). Cancer Res 69(suppl 2):66s, 2009.
9. Howell A, Cuzick J, Baum M, et al: Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365:60-62, 2005.
10. Forbes JF, Cuzick J, Buzdar A, et al: Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the ATAC trial. Lancet Oncol 9:45-53, 2008.
11. Thurlimann B, Keshaviah A, Coates AS, et al: A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med 353:2747-2757, 2005.
12. Jordan VC, Collins MM, Rowsby L, et al: A monohydroxylated metabolite of tamoxifen with potent antioestrogenic activity. J Endocrinol 75:305-316, 1977.
13. Mahgoub A, Idle JR, Dring LG, et al: Polymorphic hydroxylation of Debrisoquine in man. Lancet 2:584-586, 1977.
14. Beverage JN, Sissung TM, Sion AM, et al: CYP2D6 polymorphisms and the impact on tamoxifen therapy. J Pharm Sci 96:2224-2231, 2007.
15. Dalen P, Dahl ML, Bernal Ruiz ML, et al: 10-Hydroxylation of nortriptyline in white persons with 0, 1, 2, 3, and 13 functional CYP2D6 genes. Clin Pharmacol Ther 63:444-452, 1998.
16. Bradford LD: CYP2D6 allele frequency in European Caucasians, Asians, Africans and their descendants. Pharmacogenomics 3:229-243, 2002.
17. Goetz MP, Rae JM, Suman VJ, et al: Pharmacogenetics of tamoxifen biotransformation is associated with clinical outcomes of efficacy and hot flashes. J Clin Oncol 23:9312-9318, 2005.
18. Loprinzi CL, Sloan JA, Perez EA, et al: Phase III evaluation of fluoxetine for treatment of hot flashes. J Clin Oncol 20:1578-1583, 2002.
19. Stearns V, Beebe KL, Iyengar M, et al: Paroxetine controlled release in the treatment of menopausal hot flashes: A randomized controlled trial. JAMA 289:2827-2834, 2003.
20. Stearns V: Clinical update: New treatments for hot flushes. Lancet 369:2062-2064, 2007.
21. Love N: Patterns of Care in Medical Oncology 2(3), 2005.
22. Stearns V, Johnson MD, Rae JM, et al: Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst 95:1758-1764, 2003.
23. Jin Y, Desta Z, Stearns V, et al: CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 97:30-39, 2005.
24. Langan-Fahey SM, Tormey DC, Jordan VC: Tamoxifen metabolites in patients on long-term adjuvant therapy for breast cancer. Eur J Cancer 26:883-888, 1990.
25. Lash TL, Lien EA, Sorensen HT, et al: Genotype-guided tamoxifen therapy: Time to pause for reflection? Lancet Oncol 10:825-833, 2009.
26. Ingle JN, Suman VJ, Mailliard JA, et al: Randomized trial of tamoxifen alone or combined with fluoxymesterone as adjuvant therapy in postmenopausal women with resected estrogen receptor positive breast cancer. North Central Cancer Treatment Group Trial 89-30-52. Breast Cancer Res Treat 98:217-222, 2006.
27. Goetz MP, Knox SK, Suman VJ, et al: The impact of cytochrome P450 2D6 metabolism in women receiving adjuvant tamoxifen. Breast Cancer Res Treat 101:113-121, 2007.
28. Goetz MP, Suman V, Ames M, et al: Tamoxifen pharmacogenetics of CYP2D6, CYP2C19, and SULT1A1: Long term follow-up of the North Central Cancer Treatment Group 89-30-52 adjuvant trial (abstract 6037). Cancer Res 69(suppl), 2009.
29. Schroth W, Antoniadou L, Fritz P, et al: Breast cancer treatment outcome with adjuvant tamoxifen relative to patient CYP2D6 and CYP2C19 genotypes. J Clin Oncol 25:5187-5193, 2007.
30. Kiyotani K, Mushiroda T, Sasa M, et al: Impact of CYP2D6*10 on recurrence-free survival in breast cancer patients receiving adjuvant tamoxifen therapy. Cancer Sci 99:995-999, 2008.
31. Xu Y, Sun Y, Yao L, et al: Association between CYP2D6 *10 genotype and survival of breast cancer patients receiving tamoxifen treatment. Ann Oncol 19:1423-1429, 2008.
32. Goetz MP, Ames M, Gnant M, et al: Pharmacogenetic (CYP2D6) and gene expression profiles (HOXB13/IL17BR and molecular grade index) for prediction of adjuvant endocrine therapy benefit in the ABCSG 8 trial (abstract 57). Cancer Res 69(suppl), 2009.
33. Ramon y Cahal T, Altes A, Pare L, et al: Impact of CYP2D6 polymorphisms in tamoxifen adjuvant breast cancer treatment. Breast Cancer Res Treat (epub February 3, 2009).
34. Lim HS, Ju Lee H, Seok Lee K, et al: Clinical implications of CYP2D6 genotypes predictive of tamoxifen pharmacokinetics in metastatic breast cancer. J Clin Oncol 25:3837-3845, 2007.
35. Bonanni B, Macis D, Maisonneuve P, et al: Polymorphism in the CYP2D6 tamoxifen-metabolizing gene influences clinical effect but not hot flashes: Data from the Italian Tamoxifen Trial. J Clin Oncol 24:3708-3709; author reply 3709, 2006.
36. Wegman P, Vainikka L, Stal O, et al: Genotype of metabolic enzymes and the benefit of tamoxifen in postmenopausal breast cancer patients. Breast Cancer Res 7:R284-R290, 2005.
37. Nowell SA, Ahn J, Rae JM, et al: Association of genetic variation in tamoxifen-metabolizing enzymes with overall survival and recurrence of disease in breast cancer patients. Breast Cancer Res Treat 91:249-258, 2005.
38. Okishiro M, Taguchi T, Jin Kim S, et al: Genetic polymorphisms of CYP2D6 10 and CYP2C19 2, 3 are not associated with prognosis, endometrial thickness, or bone mineral density in Japanese breast cancer patients treated with adjuvant tamoxifen. Cancer 115:952-961, 2009.
39. Aubert RE, Stanek EJ, Yao J, et al: Risk of breast cancer recurrence in women initiating tamoxifen with CYP2D6 inhibitors (abstract CRA508). J Clin Oncol 27(18S), 2009.
40. Dezentjé V, Van Blijderveen NJ, Gelderblom H, et al: Concomitant CYP2D6 inhibitor use and tamoxifen adherence in early stage breast cancer: A pharmaco-epidemiological study (CRA509). J Clin Oncol 27(18S), 2009.
41. Borges S, Desta Z, Li L, et al: Quantitative effect of CYP2D6 genotype and inhibitors on tamoxifen metabolism: Implication for optimization of breast cancer treatment. Clin Pharmacol Ther 80:61-74, 2006.
42. Lynn Henry N, Rae JM, Li L, et al: Association between CYP2D6 genotype and tamoxifen-induced hot flashes in a prospective cohort. Breast Cancer Res Treat 117:571-575, 2009.
43. Rae J, Sikora MJ, Henry NL. Cytochrome P450 2D6 activity predicts adherence to tamoxifen therapy (abstract). Breast Cancer Res Treat 106(suppl 1):S21, 2007.
44. Punglia RS, Burstein HJ, Winer EP, et al: Pharmacogenomic variation of CYP2D6 and the choice of optimal adjuvant endocrine therapy for postmenopausal breast cancer: A modeling analysis. J Natl Cancer Inst 100:642-648, 2008.
45. Wegman P, Elingarami S, Carstensen J, et al: Genetic variants of CYP3A5, CYP2D6, SULT1A1, UGT2B15 and tamoxifen response in postmenopausal patients with breast cancer. Breast Cancer Res 9(1):R7, 2007.
46. Newman WG, Hadfield KD, Latif A, et al: Impaired tamoxifen metabolism reduces survival in familial breast cancer patients. Clin Cancer Res 14:5913-5918, 2008.
47. Desta Z, Ward BA, Soukhova NV, et al: Comprehensive evaluation of tamoxifen sequential biotransformation by the human cytochrome P450 system in vitro: prominent roles for CYP3A and CYP2D6. J Pharmacol Exp Ther 310:1062-1075, 2004.