Data Show Need for Specialized Expertise in Advanced Ovarian Cancer Surgery
Future research may explore predictors of interval debulking surgery success and the scope of required surgery in advanced ovarian cancer.
"These results emphasize the need for clinical trials to demonstrate when minimally invasive approaches can be employed without jeopardizing oncologic goals," according to the study authors.
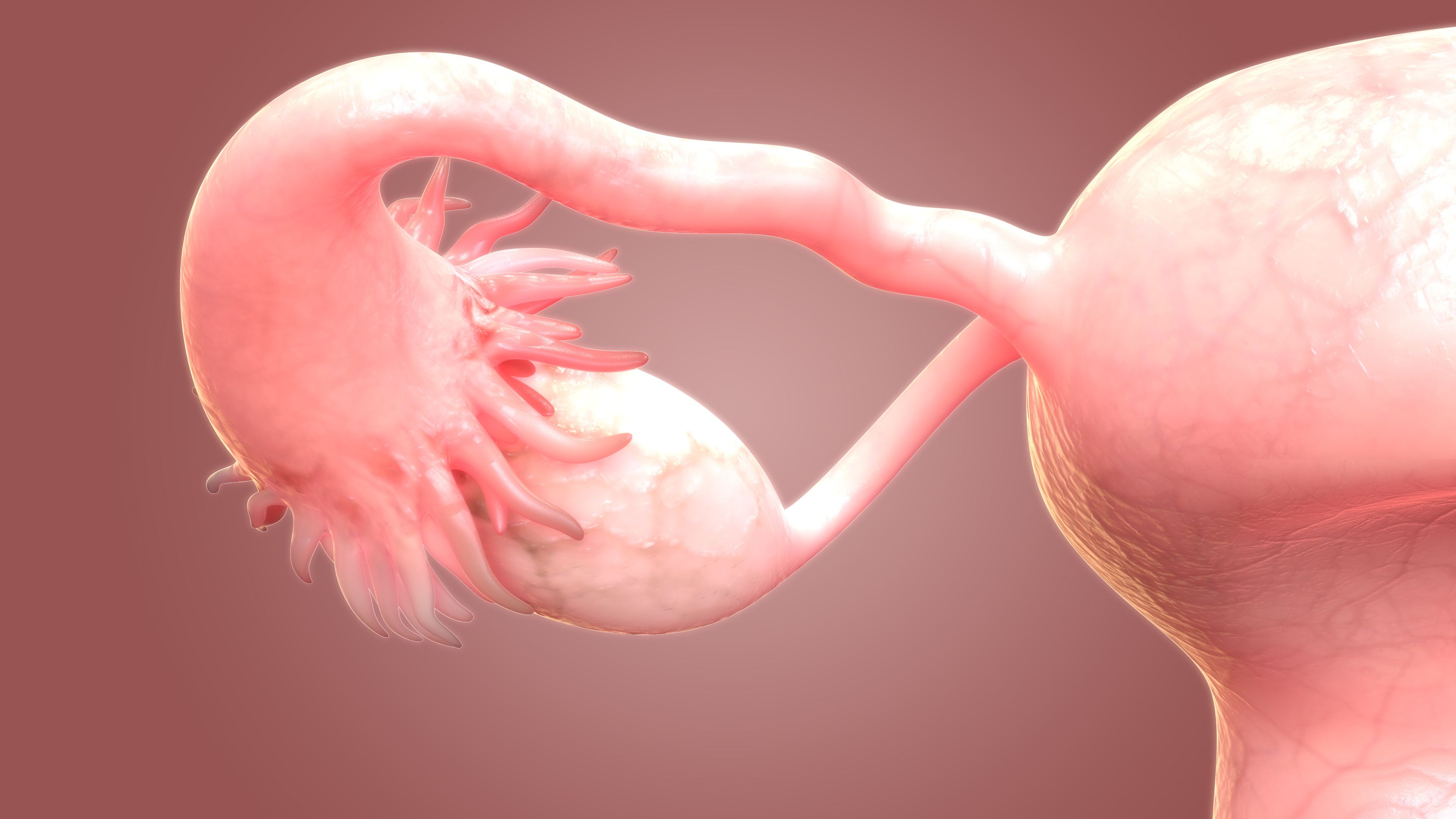
Approximately half of patients who underwent interval debulking surgery (IDS) for advanced ovarian cancer required complex procedures, indicating a need for improving specialized expertise in surgical care for this population, according to findings from a poster presentation at the 2025 Society of Gynecologic Oncology Annual Meeting on Women’s Cancer.1
In a cohort of 612 patients who received neoadjuvant chemotherapy (NACT) in combination with IDS, 50.5% required any complex procedure and 41.2% had any upper abdominal procedure. Specific surgical procedures in this cohort included diaphragm stripping or resection (36.3%), bowel resection (25.3%), splenectomy (9.3%), suprarenal and/or cardiophrenic lymph node resection (5.2%), and liver resection (2%).
Among 558 patients who received primary debulking surgery (PDS), any complex procedure was administered to 82.6% and 71.1% received any upper abdominal procedure. The most common surgical procedures included diaphragm stripping or resection (68.6%), bowel resection (60%), splenectomy (24.9%), suprarenal and/or cardiophrenic lymph node resection (16.1%), and live resection (2%).
In the IDS and PDS cohorts, 32.7% and 48.0% underwent appendectomy, respectively (P < .01). Other surgical procedures in each respective cohort included low anterior resection or reanastomosis (19.0% vs 52.9%; P < .01), other large bowel resection (9.3% vs 16.1%; P < .01), small bowel resection (5.6% vs 13.8%; P < .01), and cardiophrenic lymphadenectomy (2.9% vs 12.5%; P < .01).
“Data from 2 independent referral centers are supportive of a prior single institution study, showing that roughly half of IDS cases require complex procedures, including upper abdominal surgery,” lead study author Chiara Ainio, MD, a research fellow and resident in gynecology and obstetrics at the Mayo Clinic in Rochester, Minnesota, wrote with coauthors.1,2 “Given the critical survival benefit of complete gross resection [CGR] at IDS, these observations highlight the need for maintaining, if not expanding, specialized expertise including advanced surgical training for gynecologic oncology fellows.”
According to the study authors, surgical practice in advanced ovarian cancer has shifted from predominant PDS use to a higher frequency of administering NACT in combination with IDS. Highlighting an expectation that surgical practice in advanced ovarian cancer would infrequently require high-complexity surgery, investigators aimed to evaluate the complexity of procedures needed at IDS vs PDS to clarify the necessary surgical preparedness within the specialty.
As part of a multicentric, retrospective cohort study, investigators collected demographics, preoperative and surgical characteristics, surgical complexity scores, and surgical procedures based on anatomic location among 612 patients who received NACT plus IDS and 558 who underwent PDS. Patients with stage IIIC or IVB advanced ovarian cancer and receipt of surgery from 2016 to 2021 at the Mayo Clinic in Rochester, Minnesota, or the European Institute of Oncology in Milan, Italy, were eligible for inclusion.
The mean age was 63.3 years (SD, 10.4) in the IDS cohort compared with 59.4 (SD, 10.7) in the PDS cohort (P < .01). In each respective cohort, most patients had International Federation of Gynecology and Obstetrics stage IIIC disease (50.8% vs 68.1%), no residual disease (61.9% vs 70.4%; P < .01), and intermediate or high surgical complexity scores (56.7% vs 88.4%; P < .01). The median operative time was 238 minutes (IQR, 179-298) for IDS and 304 minutes (IQR, 244-361) for PDS (P < .01).
“Future research, including imaging and molecular studies, will explore predictors of IDS success and scope of surgery required,” the study authors added.1 “Additionally, these results emphasize the need for clinical trials to demonstrate when minimally invasive approaches can be employed without jeopardizing oncologic goals.”
References
- Ainio C, Rosanu MN, Ribero L, et al. Redefining cytoreductive surgery for advanced ovarian cancer in the neoadjuvant chemotherapy era. Poster presented at: Society of Gynecologic Oncology 2025 Annual Meeting on Women’s Cancer; March 14-17, 2025; Seattle, WA. Poster 1290.
- Filippova OT, Boecking K, Broach V, et al. Trends in specific procedures performed at the time of cytoreduction for ovarian cancer: is interval debulking surgery truly less radical? a Memorial Sloan Kettering Cancer Center Team Ovary study. Gynecol Oncol. 2024;187:80-84. doi:10.1016/j.ygyno.2024.05.009