Diagnosis of Venous Thromboembolic Disease in Cancer Patients
Venous thromboembolic disease is a common but likely underdiagnosedcondition in the cancer patient population. Timely and accuratediagnosis of venous thromboembolism is imperative due to the unacceptablemorbidity and mortality associated with a misdiagnosis.Because diagnosis of the condition based on clinical grounds alone isunreliable, physicians should select an appropriate objective diagnostictest to confirm or refute their clinical impressions. Compressionduplex ultrasound is the best initial imaging test for both suspectedupper- and lower-extremity deep venous thrombosis. Magnetic resonancevenography (MRV) is a valid alternative when ultrasound isinconclusive, but contrast venography remains the “gold standard.”Suspected pulmonary embolism should be initially evaluated by helical(spiral) computed tomography (CT) or ventilation/perfusion lungscintigraphy, the former being preferred in cases of obvious pulmonaryor pleural disease. Indeterminate studies should prompt performanceof contrast pulmonary angiography. Inferior vena cava thrombosis isalso best assessed by contrast venography, with MRV and CT reservedas alternative imaging modalities. Evidence to date suggests thatD-dimer assays remain unreliable in excluding venous thromboembolismin cancer patients. A newer latex agglutination D-dimer assay mayprove to be clinically useful in this setting.
ABSTRACT: Venous thromboembolic disease is a common but likely underdiagnosed condition in the cancer patient population. Timely and accurate diagnosis of venous thromboembolism is imperative due to the unacceptable morbidity and mortality associated with a misdiagnosis. Because diagnosis of the condition based on clinical grounds alone is unreliable, physicians should select an appropriate objective diagnostic test to confirm or refute their clinical impressions. Compression duplex ultrasound is the best initial imaging test for both suspected upper- and lower-extremity deep venous thrombosis. Magnetic resonance venography (MRV) is a valid alternative when ultrasound is inconclusive, but contrast venography remains the "gold standard." Suspected pulmonary embolism should be initially evaluated by helical (spiral) computed tomography (CT) or ventilation/perfusion lung scintigraphy, the former being preferred in cases of obvious pulmonary or pleural disease. Indeterminate studies should prompt performance of contrast pulmonary angiography. Inferior vena cava thrombosis is also best assessed by contrast venography, with MRV and CT reserved as alternative imaging modalities. Evidence to date suggests that D-dimer assays remain unreliable in excluding venous thromboembolism in cancer patients. A newer latex agglutination D-dimer assay may prove to be clinically useful in this setting.
Selection of the most appropriate and effective treatment for a patient's cancer is predicated on a timely and accurate assessment of tumor histology, disease stage, and patient performance status. In similar fashion, prescription of the most appropriate and effective treatment for a patient's cancer-associated venous thromboembolic event is dependent on a timely and accurate diagnosis.
Failure to surpass a minimum threshold of anticoagulant intensity (activated partial thromboplastin time > 1.5 times control for intravenous heparin) within 24 hours of acute deep venous thrombosis (DVT) diagnosis is associated with a markedly increased risk of late thrombosis recurrence.[1] It thus makes sense that patients with acute DVT in whom a proper diagnosis is significantly delayed should have similar suboptimal outcomes. Classification of venous thromboses as superficial vs deep and distal vs proximal, differentiation between acute and remote thrombotic events, and distinction between a venous filling defect and extrinsic vessel compression are required to ensure that patients are both effectively and safely treated.
Incidence of Venous Thromboembolism in Cancer Patients
The true magnitude of venous thromboembolism in the setting of active malignancy is likely underestimated. The incidence of clinically apparent (ie, symptomatic) venous thromboembolism in cancer patients has been reported to be approximately 15%.[2] This value pales in comparison to venous thromboembolism detection rates as high as 50% in autopsy series.[2]
Limiting factors in the proper antemortem detection of venous thromboembolism in cancer patients include an inadequate index of suspicion by many clinicians and idiosyncrasies of various diagnostic imaging modalities. The former is exacerbated by the fact that venous thromboembolism is often asymptomatic or minimally symptomatic. Even when symptoms are present, they are often nonspecific or attributed to the underlying malignancy. Worsening dyspnea in a lung cancer patient, abdominal pain postcolectomy in a colon cancer patient, and limb edema in a patient with bulky pelvic or axillary adenopathy are examples of situations in which venous thromboembolism may mimic, be confused with, or be coexistent with the underlying cancer process.
Compared to noncancer patients, cancer patients have a higher rate of recurrent venous thromboembolism while receiving treatment-intensity oral warfarin anticoagulation ("warfarin failure"), in part due to a shorter time spent within the target international normalized ratio (INR) of 2.0 to 3.0 during standard therapeutic monitoring.[3,4] They also have a three- to sixfold higher frequency of treatment-related complications (ie, bleeding during oral warfarin administration) compared to patients without cancer.[5] T
he combination of high venous thromboembolism incidence, pronounced recurrent venous thromboembolism rates, and higher rates of hemorrhage while receiving anticoagulant therapy makes venous thromboembolism management in the cancer patient a challenge. For these reasons, proper diagnosis of the disease in this special population is of the utmost importance. A missed diagnosis may result in significant morbidity and mortality due to recurrent thrombosis, while empiric therapy without a confirmed thrombosis may expose the patient to unnecessary risk in the absence of any tangible benefit.
Evolution of Diagnostic Approaches
Over the past 2 decades, we have seen venous thromboembolism diagnostic approaches shift from being purely clinical (insensitive and nonspecific) and angiography-based (invasive and expensive) to being dependent primarily on readily available non- or minimally invasive imaging modalities. When confronted with diagnosing venous thromboembolism in a cancer patient, it is important to take into consideration the limitations inherent to the various diagnostic tests and how test interpretation may be affected by unique problems related to specific malignancies. The presence of a bulky tumor or adenopathy causing extrinsic vascular structure compression and altered blood flow characteristics, direct tumor invasion of blood vessels, and the coexistence of "old" and "new" thromboses in the same venous segment can all affect the accuracy and interpretation of imaging tests.
The hypercoagulability of malignancy and unique challenges of treating venous thromboembolism in cancer patients have been addressed elsewhere in the medical literature. This article focuses on the diagnostic challenges that can have an impact on those treatment decisions. The diagnostic accuracy, advantages, and limitations of available diagnostic tests used to evaluate cancer patients for venous thrombosis are addressed, with particular attention paid to diagnostic algorithms for acute DVT and pulmonary embolism.
TABLE 1
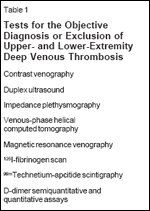
Tests for the Objective Diagnosis or Exclusion of Upper- and Lower-Extremity Deep Venous Thrombosis
Upper- and Lower-Extremity DVT
Because the diagnosis of venous thromboembolism solely on clinical grounds is insensitive and nonspecific, objective diagnostic confirmation is mandatory.[6] Currently available modalities for the objective diagnosis and exclusion of upper- and lowerextremity DVT include imaging techniques and biochemical assays (Table 1). Of these, impedance plethysmography (insensitive in cancer patients) and iodine-125- fibrinogen scanning have largely been replaced by duplex ultrasound and will not be discussed in this review. Venous duplex ultrasound is the most widely used test due to the combination of accuracy, noninvasiveness, short examination time, portability of newer equipment, and lower cost.
Contrast Venography
Venography remains the gold standard for the diagnosis of upperand lower-extremity DVT (including calf vein thrombosis) due to its ability to outline the deep venous system following the injection of radiopaque contrast medium into an antecubital or dorsal foot vein. A central deep venous access (eg, common femoral or brachial vein) may be necessary for adequate opacification of large, more central veins such as the iliac and brachiocephalic. The presence of an intraluminal filling defect in at least two distinct projections is the most reliable diagnostic criterion.[7]
• Limitations-Study limitations may include inadequate technique (in 4%-12% of all examinations) and interpretation.[7] A number of anatomic variants and the converging nature of the central venous anatomy in the upper extremity can lead to flow turbulence artifacts that may complicate interpretation.[8] The finding of complete occlusion of the iliac or brachiocephalic veins during contrast venography in cancer patients with known pelvic or intrathoracic masses is insufficient to confirm the diagnosis of an intraluminal thrombus.
Deep venous thrombosis, extrinsic venous compression by tumor, or both, may result in indistinguishable venographic appearances. In addition, such findings make the assessment of inferior vena cava (IVC) or superior vena cava (SVC) patency difficult. An alternative method, such as computed tomography (CT) or magnetic resonance imaging (MRI), should be considered to rule out the presence of extrinsic vascular compression by a tumor mass.
Duplex Ultrasound
A venous duplex ultrasound study combines real-time B-mode ultrasound with pulsed color Doppler flow imaging. The former provides direct visualization of the vessels and surrounding tissues, whereas the latter detects blood flow when the emitted ultrasound energy is reflected by red blood cells and sensed at a different frequency (Doppler shift).[9]
The diagnosis of DVT by duplex ultrasound relies on a combination of the following findings: vein noncompressibility, vein dilatation, visualization of echogenic intraluminal material, and lack of spontaneous and augmented blood flow.[10] The most reliable, validated criterion is lack of vein wall compressibility on B-mode ultrasound.[9-11] The other criteria are relatively inaccurate when applied individually.[11]
The lower-extremity deep venous segments that can routinely be examined by duplex ultrasound include the very distal external iliac, common femoral, superficial femoral, popliteal, and calf veins. The internal jugular, subclavian, axillary, and brachial veins can be routinely visualized in the neck and arms. The medial two-thirds of the subclavian veins may not be easily compressible due to their anatomic location behind the clavicles.[9]
• Limitations-An important limitation of duplex ultrasound is the inability to adequately perform compression maneuvers in the veins above the inguinal ligament (IVC, common iliac, and proximal external iliac veins) and the central veins in the upper chest (SVC and brachiocephalic veins). Even if these segments are visualized, duplex ultrasound has not been validated as a tool for the detection or exclusion of DVT in these locations.
This is of particular relevance to cancer patients with limb edema, high clinical suspicion of DVT, and unrevealing duplex ultrasound. In this clinical scenario, it is appropriate to pursue contrast venography, CT, or MRI to confirm or rule out more proximal DVT and venous compression by tumor. In a study of 37 cancer patients with leg edema and negative compression duplex ultrasound, there was 100% correlation between a monophasic waveform in the common femoral vein by spectral duplex ultrasound and the presence of either more proximal, not directly visualized DVT or extrinsic pelvic venous compression by a mass.[12]
FIGURE 1

Assessment for Extremity Deep Venous Thrombosis
It should also be noted that extrinsic venous compression can lead to DVT, and these conditions may in fact coexist. Vessel compression by a bulky tumor was demonstrated to be present in 51% of all patients with high-grade non-Hodgkin's lymphoma and venous thromboembolism.[13] Therefore, besides considering contrast- enhanced CT and/or MRI to assess for a mass effect, physicians should not hesitate to proceed with contrast venography to evaluate for DVT (Figure 1).
Although duplex ultrasound provides high sensitivity and specificity for acute femoropopliteal DVT (89%-95% and 92%-100%, respectively), it is somewhat less impressive in the setting of acute upper-extremity DVT (78% and 92%, respectively).[ 9,14] In addition, despite its high diagnostic accuracy in symptomatic patients, duplex ultrasound lacks adequate sensitivity when used for screening of asymptomatic individuals, and controversy exists with regard to its ability to properly detect calf DVT.[10]
Another controversial issue is the need for bilateral lower-extremity duplex ultrasound in patients with unilateral lower-extremity symptoms. Two studies (one performed exclusively in cancer patients) had similar results: Giess et al and Naidich et al found that 1% of patients had isolated DVT in the asymptomatic, contralateral leg and another 7% had bilateral DVT despite unilateral symptoms.[15,16] A third study, by Garcia et al, involving hospitalized DVT patients, found a 5% prevalence of DVT in the asymptomatic leg and another 5% involving both legs.[17]
Lack of documentation of acute DVT in an asymptomatic limb could have a negative impact on patient management by leading to a false diagnosis of recurrent venous thromboembolism and "warfarin failure" in future duplex ultrasound examinations. Thus, a cancer patient should always undergo bilateral duplex ultrasound for suspected lower-extremity DVT, even if the symptoms are unilateral.
Finally, the accuracy and utility of duplex ultrasound (compression method) in the setting of suspected recurrent DVT is unclear. The ability to distinguish acute from remote (chronic) DVT is hampered by the fact that 50% of patients with prior lower-extremity DVT have some degree of residual vein obstruction.[18] Old, organized thrombi may appear hyperechoic and heterogeneous sonographically, but this may not help to differentiate acute from remote DVT.[10] Unless the new DVT is found in a previously normal venous segment, compression duplex ultrasound may be unreliable.[10]
Although evaluation of vein diameters and comparison with prior duplex ultrasound measurements has been proposed as an alternative means of diagnosing recurrent DVT (with an incremental increase in vein diameter being attributed to recent DVT),[19,20] this method has not been validated by a large-scale prospective comparison with contrast venography. Given the high rate of venous thromboembolism recurrence and "warfarin failure" in cancer pa tients, it is advisable to pursue contrast venography in cases of suspected DVT recurrence (Figure 1).
Contrast-Enhanced CT
Because CT has not been validated as a method of DVT diagnosis, it should not be routinely utilized for this purpose. However, given that cancer patients frequently undergo body CT as a component of initial tumor staging, as an assessment of cancer recurrence and surveillance, or as a work-up for persistent fever, physicians are frequently faced with the dilemma of an incidental finding of filling defects involving the pelvic veins or common femoral veins. In this situation, it is imperative that the diagnosis be confirmed by a validated method, such as duplex ultrasound or contrast venography (Figure 1). CT is also not ideal in evaluating the SVC because the convergence of the central veins in the upper chest is frequently associated with flow artifacts.[ 21]
The use of combined helical CT pulmonary angiography with CT venography (venous phase CT) of the pelvis and proximal legs has been studied as a means of detecting DVT in patients with suspected pulmonary embolism. A recent retrospective study showed that this technique for CT diagnosis of DVT was as specific as, but less sensitive than duplex ultrasound in patients with lower-extremity DVT.[22] The appropriateness of this technique in cancer clinical practice is unclear at this time.
Magnetic Resonance Venography
Magnetic resonance angiography to evaluate the venous system (MRV) can be performed with time-of-flight and phase-contrast techniques. The most commonly employed is an axial, two-dimensional (2D) time-offlight technique based on standard 2D gradient echo imaging, with or without gadolinium enhancement.[ 23] A variety of techniques, such as 3D time-of-flight, 2D cine MRI, and spin echo MRI, may have advantages or disadvantages depending on the specific vascular bed under investigation.[23]
MRV was shown to be as accurate as duplex ultrasound for diagnosing lower-extremity DVT in three prospective studies that compared the two methods with contrast venography (100% sensitivity, 95%-100% specificity).[24-26] False-positive diagnoses were made in patients with extrinsic compression of the iliac veins.[25] A study in selected patients with upper-extremity central venous abnormalities showed 100% correlation between 3D gadoliniumenhanced MRV and contrast venography for detecting SVC and brachiocephalic vein stenosis or compression.[8]
Advantages of MRV include the lack of need for intravenous iodinated contrast and the ability to assess for the presence of extrinsic venous compression when combined with soft-tissue-weighted MRI. Disadvantages of MRV include cost and the fact that it is not widely available.
Nuclear Scintigraphy
Activated platelets expressing glycoprotein (GP) IIb/IIIa that become incorporated into acute evolving venous thromboses serve as the physiologic target for technetium-99m- apcitide (AcuTect) in the diagnosis of lower-extremity DVT. 99mTc-apcitide is an avid synthetic GP IIb/IIIa receptor-binding peptide that can be administered intravenously while images are collected at 10, 60, and 120-180 minutes following the injection.[ 27] As a functional rather than anatomic imaging diagnostic method for lower-extremity DVT, 99mTc-apcitide scintigraphy has the theoretical potential to discern acute from chronic (without activated platelets) thrombus. This hypothesis has not been validated.
A recent phase III prospective clinical trial in 280 patients who underwent 99mTc-apcitide scintigraphy as well as the gold-standard, contrast venography, demonstrated an overall sensitivity and specificity of 75.5% and 72.8%, respectively, for imaging acute lower-extremity DVT. Superior sensitivity and specificity (90.6% and 83.9%, respectively) were observed in patients presenting with their first lower-extremity DVT event and signs and symptoms of less than 3 days' duration. False-negative diagnoses occurred more frequently in patients with calf vein thrombosis.[ 27] In cancer patients, thrombocytopenia of any etiology and tumor-associated platelet activation likely limit the usefulness of this technique.
D-dimer
D-dimer is a degradation product resulting from the plasmin-mediated lysis of cross-linked fibrin. There are three common techniques for assaying D-dimer: enzyme-linked immunosorbent assay (ELISA), plasma-based latex agglutination assay, and wholeblood hemagglutination assay. Qualitative latex agglutination assays are relatively inexpensive to perform, widely available, and rapidly performed, but are not sufficiently sensitive to exclude venous thromboembolism.[ 28]
Both ELISA and whole-blood hemagglutination assays have been prospectively studied in clinical management trials and found to have high negative predictive values in outpatients with suspected venous thromboembolism.[ 29,30] These studies suggest that lack of D-dimer elevation combined with a negative noninvasive imaging test reliably excludes lower-extremity DVT, but D-dimer elevation alone neither rules in nor rules out thrombosis.
In general, these D-dimer assays are excellent screening tests for venous thromboembolism, but the whole-blood hemagglutination D-dimer assay lacks acceptable performance characteristics for excluding venous thromboembolism in cancer patients.[31] In the retrospective analysis by Lee et al, the negative predictive value for acute lower-extremity DVT was 78.9% in cancer patients, compared with 96.5% in those without cancer.[31] This difference can be explained by either a higher prevalence of thrombosis or higher D-dimer levels at baseline in the cancer population, even in the absence of acute thrombosis.[31]
Conversely, false-negative D-dimer results have been described in cancer patients with pulmonary embolism and baseline impaired endogenous fibrinolysis.[32] More recently, however, a subgroup analysis from a retrospective cohort study showed that the negative predictive value of a new latex agglutination assay remained high and useful in patients with known cancer.[33] Until conclusive evidence from larger studies is available, we feel that D-dimer assays should not be used to exclude venous thromboembolism in cancer patients.
Extremity DVT Algorithm
Clinical suspicion of lower-extremity DVT or an incidental finding of DVT on CT should be initially evaluated by duplex ultrasound or, if DVT proximal to the common femoral vein is suspected, contrast venography (Figure 1). A nondiagnostic duplex ultrasound should prompt further evaluation with contrast venography. The findings of a noncompressible vein by duplex ultrasound or an intraluminal filling defect by venography in the setting of new clinical signs and symptoms are diagnostic for acute DVT.
If the patient is known to have a pelvic or intrathoracic mass, MRV may be considered in combination with duplex ultrasound or venography due to its ability to visualize both extravascular and vascular structures. More studies are needed to specifically determine the role of 99mTc-apcitide scintigraphy for the diagnosis of DVT in cancer patients.
Pulmonary Embolism
TABLE 2
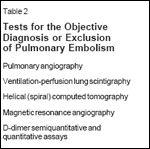
Tests for the Objective Diagnosis or Exclusion of Pulmonary Embolism
Currently available tests for the diagnostic confirmation or exclusion of pulmonary embolism include blood-based biochemical assays (eg, D-dimer) and a variety of imaging tests (Table 2). D-dimer testing has already been discussed and in our opinion is not reliable for the exclusion of pulmonary embolism in the cancer setting. Ventilation/perfusion scintigraphy and helical (spiral) CT are the most commonly used tests, whereas magnetic resonance angiography is a promising technique but of limited use in current routine clinical practice. Pulmonary arteriography remains the gold standard despite the fact that many feel it is no more accurate than helical CT.
Pulmonary Angiography
Pulmonary angiography is typically performed via common femoral vein access (or internal jugular or brachial vein) and can include selective catheterization of either or both the right and left main pulmonary arteries. The pulmonary vascular tree is visualized after an injection of iodinated contrast medium.
For the diagnosis of pulmonary embolism, pulmonary angiography offers a specificity approaching 100% when a filling defect or abrupt "cutoff' of a pulmonary artery branch is present.[33,34] Ancillary findings that may be present but are not specific for pulmonary embolism include abnormal distribution of flow to the different lobes, delayed venous return and partially opacified, tortuous vessels.[34]
Because of the invasive nature of the procedure, it has the potential for minor and major complications as well as death, which were observed in 5%, 1%, and 0.5%, respectively, in 1,111 patients who underwent pulmonary angiography in the Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED).[35] Usually, other noninvasive methods are performed as the initial work-up of patients with suspected pulmonary embolism, but the risks of pulmonary angiography are sufficiently low to justify its use in the appropriate clinical setting (Figures 2 and 3).[35]
Ventilation/Perfusion Lung Scintigraphy
Ventilation/perfusion (V/Q) lung scanning combines ventilation and perfusion nuclear medicine imaging techniques. The ventilation (V) study involves the inhalation of a radioactive gas (typically xenon-133 or -127, krypton-81, or aerosolized technetium- 99m), which provides an image of all ventilated portions of the lung. The perfusion (Q) study consists of an intravenous injection of 99mTclabeled macroaggregated human serum albumin particles with the patient in supine position. The particles become trapped in approximately 0.1% of the pulmonary capillary bed.[34] Any obstruction to arterial flow is viewed as an area of "perfusion defect" on gamma-camera images. The presence of multiple segmental perfusion defects increases the test specificity for pulmonary embolism. Based on the presence and extent of matched (absence of both perfusion and ventilation) and unmatched (absence of perfusion but preserved ventilation) defects, the V/Q scan can be interpreted using PIOPED published criteria as either normal or low, intermediate, or high probability for pulmonary embolism.[36,37]
Because it provides indirect evidence of pulmonary embolism, V/Q scans are most clinically useful when considered in combination with an assessment of pretest clinical suspicion.[ 36] While detailed analysis of the PIOPED results is beyond the scope of this article, some of the key findings include: (1) a normal V/Q scan essentially rules out clinically significant pulmonary embolism, (2) a high-probability V/Q scan alone had a high positive predictive value (88%) for pulmonary embolism, (3) 96% of patients with high pretest clinical suspicion and a high-probability V/Q scan had pulmonary embolism docu- mented by angiography, and (4) only 4% of patients with both a low-probability V/Q scan and low clinical suspicion had pulmonary embolism on angiography.[36] Low- and intermediate- probability scans are now considered together as being "indeterminate" scans.
A plain chest radiograph is necessary prior to interpretation of a V/Q scan. Pleural effusions, bullous disease, pulmonary infiltrates or masses, and atelectasis have been associated with a higher frequency of indeterminate scans and a lower positive predictive value of highprobability findings.[34]
A V/Q scan has the advantage of not using iodinated contrast. Its greatest limitation as a diagnostic tool for pulmonary embolism is the fact that it provides a definitive result in a minority of patients. In the PIOPED series, only 13% had a normal study and 14% had a high-probability scan.[36] Therefore, it can be expected that the majority (as many as 77%) of all patients undergoing a V/Q scan will have a nondiagnostic, indeterminate scan that warrants further testing such as pulmonary angiography to confirm or exclude pulmonary embolism.
Pitfalls in the interpretation of V/Q scintigraphy may represent a significant problem in the cancer population, particularly when primary or secondary (metastatic) pulmonary involvement is present. Patients with a prior history of pulmonary embolism may have a high-proba- bility V/Q scan that does not reflect a new, acute event but rather the old pulmonary embolism instead.[36] False high-probability scans may occur as a consequence of an abnormal perfusion scan due to pulmonary artery invasion or compression, regional hypoventilation secondary to bronchial compromise, pulmonary vein obstruction by hilar masses or adenopathy, or pulmonary leukostasis.[ 38-41] The unique finding of unilateral absence of pulmonary artery perfusion has been described in such conditions as such conditions as lymphoma, lung carcinoma, and pulmonary artery sarcomas.[ 38,39,42,43] Areas of V/Q mismatch may also be the result of prior administration of radiation therapy to the chest.[44]
Helical CT Angiography
Contrast-enhanced spiral CT is performed by scanning a distance of 10 to 12 cm from the aortic arch to 2 cm below the inferior pulmonary veins during a single 30-second breath hold while the pulmonary vasculature is opacified by the automated injection of iodinated contrast medium.[ 45] Technical parameters such as collimation, rate and timing of contrast administration and scanning delay, as well as breathing, motion artifacts, and even central venous catheters, can influence the timing and quality of opacification of the pulmonary arteries, thereby potentially compromising the quality of the study.[45]
Spiral CT has an overall sensitivity of 53% to 100% and specificity of 78% to 100% for the diagnosis of pulmonary embolism.[34,45] These rates approach 95% to 100% for the central and segmental pulmonary arterial branches, but are lower (sensitivity, 53%-63%) for pulmonary embolism involving the subsegmental branches.[34,45,46] This can be, in part, explained by the fact that older techniques (5-mm collimation, pitch of 1) resulted in an effective section thickness of 6.57 mm, as opposed to newer, currently available scanning parameters that result in effective section thickness of 2.65 mm (2-mm collimation, pitch of 1.7) and improved visualization of the subsegmental arterial bed.[45]
FIGURE 2

Assessment for Pulmonary Embolism by CT Scan
Nonetheless, studies with the highest frequency of isolated subsegmental pulmonary embolism (and hence, lowest spiral CT sensitivity) have been reported in patients who also had a nondiagnostic V/Q scan, and data from PIOPED suggested that only 6% of pulmonary embolisms are subsegmental.[36,46] Whether subsegmental pulmonary embolism is clinically relevant and needs to be definitively detected is a matter of great, unresolved controversy. Therefore, it is important to keep in mind that a normal spiral CT does not exclude pulmonary embolism and, in the setting of a high pretest suspicion, the performance of the gold standard, pulmonary angiography, is indicated (Figure 2).
The major strengths of spiral CT include the rapid nature of data acquisition and the lower percentage of nondiagnostic studies (due to its ability to simultaneously evaluate vascular and nonvascular intrathoracic structures). In patients evaluated for pulmonary embolism, spiral CT has been shown to provide an alternative diagnosis that either suggested or supported the final clinical diagnosis in up to 67% of examinations.[47]
Specific oncologic applications of the test include detection of endobronchial lesions, pulmonary artery invasion, and venoatrial extension of bronchogenic carcinoma.[45] Interpretative pitfalls may occur in some cases, including unilateral pulmonary artery extrinsic compression or endoluminal obstruction and unilateral bronchial obstruction, which may produce ipsilateral delayed opacification of the arterial tree.[45]
Magnetic Resonance Angiography
Magnetic resonance angiography is a promising technique in patients with suspected pulmonary embolism, particularly with the use of 3D, gadolinium- enhanced imaging.[23,34] In a preliminary study of 30 patients (8 of whom had pulmonary angiography- proven pulmonary embolism), magnetic resonance angiography had a sensitivity of 75% to 100% and specificity of 95% to 100% for diagnosing pulmonary embolism.[48] In cases of suspected pulmonary artery sarcoma, magnetic resonance angiography may be more useful than CT because the presence of gadolinium enhancement suggests tumor instead of thrombus.[43]
Pulmonary Embolism Algorithm
Physicians should have a high index of suspicion for pulmonary embolism in cancer patients and low threshold for pursuing a diagnostic work-up. When a cancer patient is suspected of having pulmonary embolism, a chest radiograph should be performed to exclude other conditions that may require immediate intervention, such as a central line-related tension pneumothorax. Otherwise, the chest x-ray should not be used as a means of supporting or refuting the need for specific diagnostic testing for pulmonary embolism.
FIGURE 3

Assessment for Pulmonary Embolism by V/Q Lung Scan
When the chest x-ray is abnormal, we prefer an initial diagnostic evaluation by spiral CT because of the high likelihood that a V/Q scan will have an indeterminate result (Figures 2 and 3). In the cancer patient, the ability to evaluate intrathoracic structures also makes spiral CT the preferred initial diagnostic test. If the chest x-ray is normal, a V/Q scan approach may be chosen, but it is important that physicians clearly establish and document the perceived pretesting clinical suspicion of pulmonary embolism. Otherwise, PIOPED probability criteria may not be applicable.
Regardless of the initial diagnostic approach, an indeterminate or negative scan should be followed by a duplex ultrasound of the legs and arms, in those with upper-extremity symptoms of pain, swelling, or an indwelling catheter. A positive duplex ultrasound does not confirm pulmonary embolism, but detection of acute DVT will prompt and justify acute systemic anticoagulation. In the absence of acute DVT, pulmonary angiography is necessary to confirm or exclude pulmonary embolism, particularly in those with an indeterminate V/Q scan or spiral CT. With the spiral CT-based approach to pulmonary embolism diagnosis, the presence of an alternative diagnosis that does not fully explain the patient's symptoms should be considered an indeterminate finding, in which case further work-up with pulmonary angiography is indicated.
IVC and Other Abdominal Vein DVT
Many cancer patients undergo serial imaging with CT as a means of assessing cancer therapy efficacy, disease stage or progression, and nonspecific abdominal symptoms. Incidental findings of what appears to be DVT should not affect patient treatment and prompt the reflexive placement of an IVC filter. Immediate and proper diagnostic imaging is especially needed in such a situation.
Contrast Venography
Contrast venography is the reference standard to conclusively show the presence or absence of IVC thrombosis. Therefore, an incidental finding of an IVC "filling defect" by CT should be confirmed by venography. However, in cancer patients, not all intraluminal filling defects represent thrombus, and the distinction between intravascular tumor and thrombus may require further investigation with CT or MRI and, in selected cases, transvenous catheter-guided biopsy. The diagnosis of portal or ovarian vein thromboses is even more challenging because of limited ability to perform selective venography.
Contrast-Enhanced CT
CT remains a nonvalidated method to assess for the presence of thrombus in the IVC. Indirect signs that have been described in cases of IVC thrombosis include IVC enlargement, reduced IVC lumen density compared to the aorta, and rim enhancement.[ 49] However, these signs may occur as a result of contrast flow phenomena mimicking an intraluminal filling defect and have also been described in patients with renal cell or adrenal cortical carcinoma extending into the renal veins and IVC to produce a "tumor thrombus."[49]
The above-mentioned characteristic features of a thrombosed vein are also used in the diagnosis of portal vein thrombosis by CT. These signs are of little value in a patient with prior history of portal vein thrombosis who is suspected of having a new thrombotic event involving the same vein. Despite the fact that the true sensitivity of contrastenhanced CT in diagnosing portal vein thrombosis is unknown, its specificity has been suggested to be quite high.[50] The presence of cavernous transformation-a "mass-like" network of collateral veins-suggests a remote thrombosis.[50]
Only one study on the diagnostic imaging of ovarian vein thrombosis in cancer patients has been published.[ 51] This was a retrospective series of six patients with the condition in association with breast cancer, pancreatic carcinoma, or adenocarcinoma of unknown primary. CTbased diagnosis was made by the detection of an enlarged ovarian vein containing low-attenuation thrombus. Unlike most patients with puerperal ovarian vein thrombosis, none of the patients in this small series had the related CT findings of uterine enlargement and other pelvic masses.[51]
Magnetic Resonance Venography
MRV is a highly accurate noninvasive method for diagnosing IVC and portal vein thrombosis, particularly when spin echo and cine MRI techniques are used in combination.[ 23] The usefulness of MRV for the diagnosis of ovarian vein thrombosis is unknown. MRV may help differentiate acute from chronic thrombus based on differences in patterns of signal intensity.[23,52]
Artifacts created by flow phenomena may cause signal voids at the junction of the renal vein and the IVC, because this is an area of slow, convergent blood flow. This may lead to a false-positive diagnosis of IVC thrombosis.[53] MRV is also limited in distinguishing true portal vein thrombosis from tumor invasion of the portal vein unless an adjacent mass is seen.[23] In this setting, contrast- enhanced color Doppler ultrasound may be a reliable diagnostic tool.[54]
The rare IVC leiomyosarcoma can be equally well demonstrated by CT or MRI, although MRI is superior because it seems to be capable of differentiating tumor (homogeneous, intermediate signal intensity on T1- weighted images) from thrombus (hyperintense on T1- and T2-weighted images).[55]
Conclusions
Key elements for the diagnosis of venous thromboembolism in the cancer patient are a high index of suspicion coupled with appropriate selection of an initial diagnostic workup. The results of the diagnostic workup need to be interpreted according to the individual patient's clinical presentation and associated medical conditions.
A rational and efficient diagnostic strategy should include the most appropriate tests to confirm or exclude venous thromboembolism, with the ultimate goal of defining the need for antithrombotic therapy in a timely fashion. Although the preferred initial diagnostic approach to venous thromboembolism is clearly based on noninvasive imaging, physicians should not hesitate to pursue the gold standard invasive procedures when the initial work-up is inconclusive, as the findings may have a significant impact on patient management and outcomes.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1.
Hull RD, Raskob GE, Brant RF, et al: Theimportance of initial heparin treatment on longtermclinical outcomes of antithrombotic therapy:the emerging theme of delayed recurrence.Arch Intern Med 157:2317-2321, 1997.
2.
Luzzatto G, Schafer AI: The prothromboticstate in cancer. Semin Oncol 17:147-159,1990.
3.
Hutten BA, Prins MH, Gent M, et al:Incidence of recurrent thromboembolic andbleeding complications among patients withvenous thromboembolism in relation to bothmalignancy and achieved international normalizedratio: A retrospective analysis. J Clin Oncol18:3078-3083, 2000.
4.
Bona RD, Sivjee KY, Hickey AD, et al:The efficacy and safety of oral anticoagulationin patients with cancer. Thromb Haemost74:1055-1058, 1995.
5.
Levine MN, Lee AYY: Treatment ofvenous thromboembolism in cancer patients.Semin Thromb Hemost 25:245-249, 1999.
6.
Hull R, Raskob G, Leclerc J, et al: Thediagnosis of clinically suspected venous thrombosis.Clin Chest Med 5: 439-456, 1984.
7.
Lensing AWA, Buller HR, Prandoni P, etal: Contrast venography, the gold standard forthe diagnosis of deep vein thrombosis: Improvementin observer agreement. Thromb Haemost67:8-12, 1992.
8.
Thornton MJ, Ryan R, Varghese JC, et al:A three-dimensional gadolinium-enhanced MRvenography technique for imaging centralveins. Am J Roentgenol 173:999-1003, 1999.
9.
Cronan JJ: Venous thromboembolic disease:The role of US. Radiology 186:619-630,1993.
10.
Dauzat M, Laroche JP, Deklunder G, etal: Diagnosis of acute lower limb deep venousthrombosis with ultrasound: Trends and controversies.J Clin Ultrasound 25:343-358, 1997.
11.
Lensing AWA, Prandoni P, Brandjes D,et al: Detection of deep-vein thrombosis byreal-time B-mode ultrasonography. N Engl JMed 320:342-345, 1989.
12.
Bach AM, Hann LE: When the commonfemoral vein is revealed as flattened on spectralDoppler sonography: Is it a reliable sign fordiagnosis of proximal venous obstruction? AmJ Roentgenol 168:733-736, 1997.
13.
Ottinger H, Belka C, Kozole G, et al:Deep venous thrombosis and pulmonary arteryembolism in high-grade non-Hodgkin’s lymphoma:Incidence, causes and prognostic relevance.Eur J Haematol 54:186-194, 1995.
14.
Knudson GJ, Wiedemeyer DA, EricksonSJ, et al: Color Doppler sonographic imagingin the assessment of upper-extremity deepvenous thrombosis. Am J Roentgenol 154:399-403, 1990.
15.
Giess CS, Bach AM, Hann LE: Lowerextremity venous sonography in the high-riskcancer population: One leg or two? Am J Roentgenol176:1049-1052, 2001.
16.
Naidich JB, Torre JR, Pellerito JS, et al:Suspected deep venous thrombosis: Is US ofboth legs necessary? Radiology 200:429-431,1996.
17.
Garcia ND, Morasch MD, Ebaugh JL, etal: Is bilateral ultrasound scanning of the legsnecessary for patients with unilateral symptomsof deep vein thrombosis? J Vasc Surg34:792-797, 2001.
18.
Heijboer H, Jongbloets LMM, BullerHR, et al: Clinical utility of real-time compressionultrasonography for diagnostic managementof patients with recurrent venousthrombosis. Acta Radiol 33:297-300, 1992.
19.
Prandoni P, Cogo A, Bernardi E, et al: Asimple ultrasound approach for the detectionof recurrent proximal-vein thrombosis. Circulation88(part I):1730-1735, 1993.
20.
Prandoni P, Lensing AWA, Bernardi E,et al: The diagnostic value of compression ultrasonographyin patients with suspected recurrentdeep vein thrombosis. Thromb Haemost88:402-406, 2002.
21.
Moncada R, Cardella R, Demos TC, etal: Evaluation of superior vena cava syndromeby axial CT and CT phlebography. Am J Roentgenol143:731-736, 1984.
22.
Peterson DA, Kazerooni EA, WakefieldTW, et al: Computed tomographic venographyis specific but not sensitive for diagnosis ofacute lower-extremity deep venous thrombosisin patients with suspected pulmonary embolism.J Vasc Surg 34:798-804, 2001.
23.
Link KM, Lesko NM: Magnetic resonanceangiography: Great vessels and abdomen,in Stark DD, Bradley WG Jr (eds):Magnetic Resonance Imaging, pp 373-383.Mosby, 1999.
24.
Laissy JP, Cinqualbre A, Loshkajian A,et al: Assessment of deep venous thrombosis inthe lower limbs and pelvis: MR venographyversus duplex Doppler sonography. Am J Roentgenol167:971-975, 1996.
25.
Carpenter JP, Holland GA, Baum RA:Magnetic resonance venography for the detectionof deep venous thrombosis: Comparisonwith contrast venography and duplex Dopplerultrasonography. J Vasc Surg 18:734-741,1993.
26.
Evans AJ, Sostman HD, Knelson MH, etal: Detection of deep venous thrombosis: Prospectivecomparison of MR imaging withcontrast venography. Am J Roentgenol 161:131-139, 1993.
27.
Taillefer R, Edell S, Innes G, et al: Acutethromboscintigraphy with 99mTc-apcitide:Results of the phase 3 multicenter clinical trialcomparing 99mTc-apcitide scintigraphy withcontrast venography for imaging acute DVT. JNucl Med 41:1214-1223, 2000.
28.
Brill-Edwards P, Lee A: D-dimer testingin the diagnosis of acute venous thromboembolism.Thromb Haemost 82:688-694, 1999.
29.
Ginsberg JS, Kearon C, Douketis J, et al:The use of D-dimer testing and impedanceplethysmographic examination in patients withclinical indications of deep vein thrombosis.Arch Intern Med 157:1077-1081, 1997.
30.
Bernardi E, Prandoni P, Lensing AW, etal: D-dimer testing as an adjunct to ultrasonographyin patients with clinically suspected deepvein thrombosis: Prospective cohort study. TheMulticenter Italian D-dimer Ultrasound StudyInvestigators Group. Br Med J 317:1037-1040,1998.
31.
Lee AYY, Julian JA, Levine MN, et al:Clinical utility of a rapid whole-blood D-dimerassay in patients with cancer who present withsuspected acute deep venous thrombosis. AnnIntern Med 131:417-423, 1999.
32.
Deitcher SR, Lucore CL, Eisenberg PR:Impaired resolution of massive pulmonary embolismassociated with an inhibited fibrinolyticresponse. Am J Med 96:483-484, 1994.
33.
Bates SM, Grand’Maison A, JohnstonM, et al: A latex D-dimer reliably excludesvenous thromboembolism. Arch Intern Med161:447-453, 2001.
34.
Gotway MB, Edinburgh KJ, FeldsteinVA, et al: Imaging evaluation of suspected pulmonaryembolism. Curr Probl Diag Radiol28:132-184, 1999.
35.
Stein PD, Athanasoulis C, Alavi A, et al:Complications and validity of pulmonary angiographyin acute pulmonary embolism. Circulation85:462-468, 1992.
36.
The Prospective Investigation of PulmonaryEmbolism Diagnosis (PIOPED) Investigators:Value of the ventilation/perfusion scanin acute pulmonary embolism. JAMA 263:2753-2759, 1990.
37.
Gottschalk A, Sostman HD, ColemanRE, et al: Ventilation-perfusion scintigraphy inthe PIOPED study. Part II. Evaluation of thescintigraphic criteria and interpretations. J NuclMed 34:1119-1124, 1993
38.
Veatch MD, Lewin JM, O’Brien RF, etal: Small cell carcinoma as the cause for anondiagnostic V/Q lung scan. Am J Emerg Med14:183-185, 1996.
39.
Martino J, Allende J, Herrero A, et al:Nonembolic high-probability perfusion lungscan for pulmonary thromboembolism. Am JEmerg Med 12:664-666, 1994.
40.
Mendelson DS, Train JS, Goldsmith SJ,et al: Ventilation-perfusion mismatch due toobstruction of pulmonary vein. J Nucl Med22:1062-1063, 1981.
41.
Kaminsky DA, Hurwitz CG, OlmsteadJI: Pulmonary leukostasis mimicking pulmonaryembolism. Leuk Research 24:175-178,1999.
42.
Chow B, Wittram C, Lee VW: Unilateralabsence of pulmonary perfusion mimickingpulmonary embolism. Am J Roentgenol176:712, 2001.
43.
Cox JE, Chiles C, Aquino SL, et al:Pulmonary artery sarcomas: A review of clinicaland radiologic features. J Comput AssistTomogr 21:750-755, 1997.
44.
Chin BB, Welsh JS, Kleinberg L, et al:Nonsegmental ventilation-perfusion scintigraphymismatch after radiation therapy. Clin NuclMed 24:54-56, 1999.
45.
Remy-Jardin M, Remy J: Spiral CT angiographyof the pulmonary circulation. Radiology212:615-636, 1999.
46.
Goodman LR, Curtin JJ, Mewissen MW,et al: Detection of pulmonary embolism inpatients with unresolved clinical and scintigraphicdiagnosis: Helical CT versus angiography.Am J Roentgenol 164:1369-1374,1995.
47.
Kim KI, Muller NL, Mayo JR: Clinicallysuspected pulmonary embolism: Utility of spiralCT. Radiology 210:693-697, 1999.
48.
Meaney JFM, Weg JG, Chenevert TL, etal: Diagnosis of pulmonary embolism withmagnetic resonance angiography. N Engl J Med336:1422-1427, 1997.
49.
Breda AV, Rubin BE, Druy EM: Detectionof inferior vena cava abnormalities by computedtomography. J Comput Assist Tomogr3:164-169, 1979.
50.
Marn CS, Francis IR: CT of portal venousocclusion. Am J Roentgenol 159:717-726, 1992.
51.
Jacoby WT, Cohan RH, Baker ME, et al:Ovarian vein thrombosis in oncology patients:CT detection and clinical significance. Am JRoentgenol 155:291-294, 1990.
52.
Soler R, Rodriguez E, Lopez MF, et al:MR imaging in inferior vena cava thrombosis.Eur J Radiol 19:101-107, 1995.
53.
Cheng HC, Chu WC, Chai JW: Convergentflow phenomenon mimics the appearanceof venous thrombosis in gradient-echo imageswith or without the presence of a contrast agent.Magnet Reson Imag 15:863-867, 1997.
54.
Ricci P, Cantisani V, Biancari F, et al:Contrast-enhanced color Doppler US in malignantportal vein thrombosis. Acta Radiol41:470-473, 2000.
55.
Blum U, Wildanger G, Windfuhr M, etal: Preoperative CT and MR imaging of inferiorvena cava leiomyosarcoma. Eur J Radiol20:23-27, 1995.
Oncology Peer Review On-The-Go: Cancer-Related Fatigue Outcome Measures in Integrative Oncology
September 20th 2022Authors Dori Beeler, PhD; Shelley Wang, MD, MPH; and Viraj A. Master, MD, PhD, spoke with CancerNetwork® about a review article on cancer-related fatigue published in the journal ONCOLOGY®.
Late Hepatic Recurrence From Granulosa Cell Tumor: A Case Report
Granulosa cell tumors exhibit late recurrence and rare hepatic metastasis, emphasizing the need for lifelong surveillance in affected patients.