Evaluating the Rapidly Changing ADC Landscape in HR+/HER2– Breast Cancer
"The data, even in fast progressors and within 6 months of endocrine therapy, [show it] is working," stated Monica Khunger Malhotra, MD.
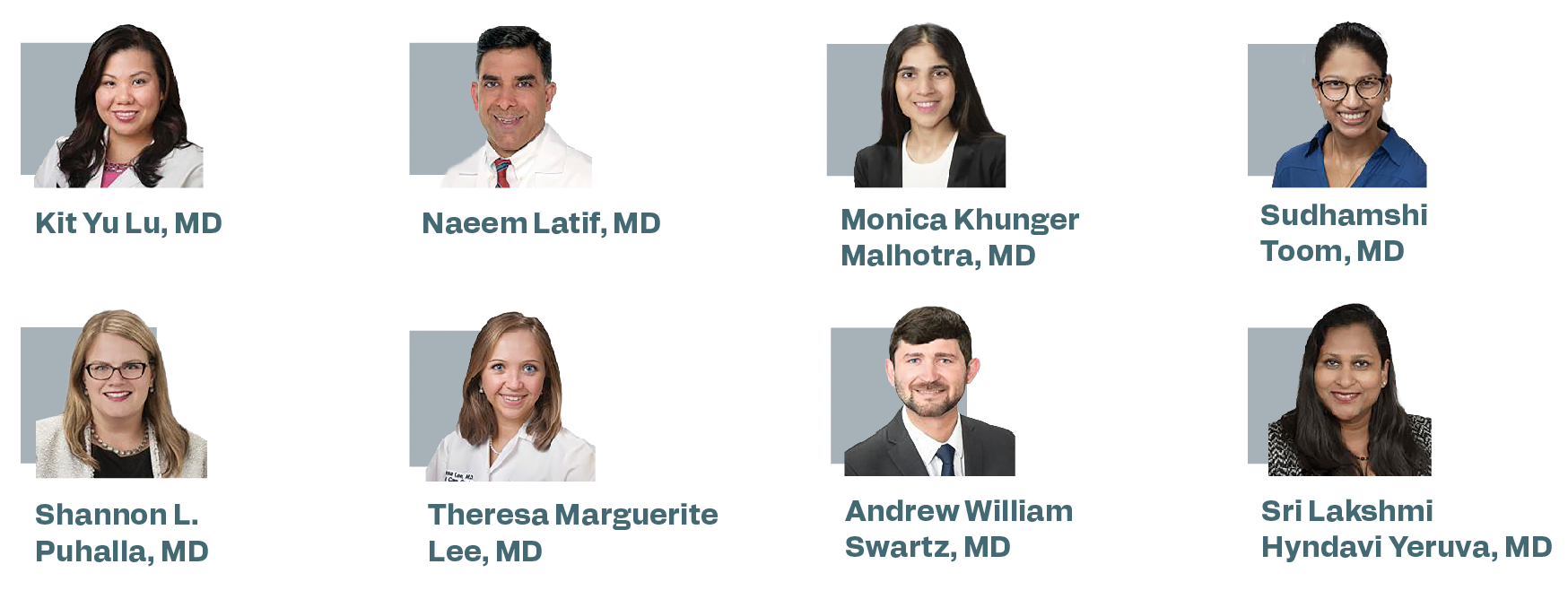
The expert panel.
During a CancerNetwork-hosted Satellite Sessions program at the University of Pittsburgh Medical Center (UPMC) Hillman Cancer Center, a panel of experts discussed the role of antibody-drug conjugates (ADCs) in triple-negative breast cancer and hormone receptor (HR)–positive, HER2-negative breast cancer. ADCs of note were sacituzumab govitecan-hziy (Trodelvy), fam-trastuzumab deruxtecan-nxki (T-DXd; Enhertu), and datopotamab deruxtecan-dlnk (Dato-DXd; Datroway), with an added focus on sacituzumab govitecan and T-DXd use from the phase 3 TROPiCS-02 trial (NCT03901339) and the phase 3 DESTINY-Breast06 trial (NCT04494425), respectively.1,2
The panel was led by Kit Yu Lu, MD, a hematology and breast medical oncologist, and Shannon L. Puhalla, MD, an assistant professor of medicine at the University of Pittsburgh School of Medicine, and a medical oncologist and hematologist at UPMC. They were joined by Monica Khunger Malhotra, MD, a medical oncologist; Andrew William Swartz, MD, a hematology oncologist; Naeem Latif, MD, a medical oncologist; Theresa Marguerite Lee, MD, a breast and hematology medical oncologist; Sudhamshi Toom, MD, a medical oncologist and hematologist; and Sri Lakshmi Hyndavi Yeruva, MD, a medical oncologist and hematologist, all at UPMC Hillman Cancer Center.
The ADC Landscape in Breast Cancer
Puhalla / We have [many] ADCs that are available. Right now, for [estrogen receptor (ER)]–positive, HER2-negative, HER2-low, and HER2-ultralow [disease], the 3 drugs that we have commercially available, similar to triple-negative [breast cancer], are sacituzumab govitecan, T-DXd, and Dato-DXd, [which was recently approved] for patients who are ER positive and HER2 negative.
The differences, as you can see, are in the targets where we have HER2 with T-DXd and then TROP2 with the sacituzumab govitecan and the Dato-DXd. I think of these drugs as being similar, certainly in their mechanism of action. I think of them as similar in the payload we’re seeing. [There are] these differences in the target, but I do think they’ve changed the way we treat metastatic ER-positive, HER2-low disease, and trying to decide the sequencing is a clinical challenge.
In clinical practice, how do you differentiate between a patient who has developed endocrine resistance but may still benefit from endocrine-based combination therapy vs [a patient who is] endocrine refractory? When you’ve got a patient who’s had a first-line CDK4/6 inhibitor, and now you’re thinking about what to do in the second line, what are the things you’re [considering] if you’re trying a second CDK4/6 inhibitor? If you’ve got someone who has a PIK3CA mutation, are you going straight to those drugs? In which circumstances would you potentially go straight to an ADC or consider an ADC?
Malhotra / The way I think about this is, “How long were they on the first-line CDK4/6 inhibitor?” If they were on it for 2 or 3 years, and if it’s bone-only or very mild progression, then I know there are data from the [phase 3 MAINTAIN trial (NCT02632045)].3 If they were on palbociclib [Ibrance], I switch them to ribociclib [Kisqali] or switch to fulvestrant [Faslodex], provided they don’t have PIK3CA or any other mutation. That’s if somebody has been on a frontline CDK4/6 inhibitor for a while and only has small bone-only [metastases]. If [there are] no other [mutations], and I checked for ESR1 [and] PIK3CA, and I don’t find anything else—if I find ESR1 or PIK3CA, then I try to switch to targeted [therapy], only if they’re not in visceral crisis.
Puhalla / T-DXd is probably much easier to tolerate than alpelisib [Vijoice]. We think of sometimes trying to avoid [intravenous] treatment at all costs, but there are certainly a lot of patients who have a lot of toxicity in the PIK3CA inhibitor space. Those are things that I think about, too.
If it’s somebody [who] I’m worried [has] a metabolic syndrome or is diabetic or prediabetic, where I’m worried about hyperglycemia, those are things [to consider]. As far as a hard and fast rule, I completely agree with [Dr Malhotra]. When we have someone who’s on a CDK4/6 inhibitor—and when these drugs came out, we were all spoiled with these long [progression-free survival (PFS) rates] in these patients—but there are certainly still those few patients who are ER-positive, metastatic and who have that PFS that’s under the 24 months that you’re looking for. Those are the patients [about whom] I’m thinking, “Yeah, this is probably not somebody where I’m going to get years and years on various endocrine therapy combinations.”
Analyzing TROPiCS-02 Data
Puhalla / Looking at data for sacituzumab govitecan in patients who were endocrine resistant and ER positive, HER2 negative, these patients had received at least 1 prior endocrine therapy, a taxane, and a CDK4/6 inhibitor. They could have had 2 to 4 prior lines of chemotherapy, similar to the heavily pretreated patients in the triple-negative breast cancer data. These patients were [randomly assigned] to receive sacituzumab govitecan at the standard dose vs the treatment of physician’s choice, which included typical treatments after taxane in patients with metastatic disease.
Most patients had a good performance status, with a significant number having visceral and liver metastases. Only a minority had de novo metastatic disease. The median time from metastatic diagnosis to randomization was approximately 4 years, indicating a heavily pretreated population. Many patients had prior adjuvant chemotherapy, and prior CDK4/6 inhibitor use was greater than 12 months in a significant portion. The median number of prior chemotherapy regimens was 3.
In the ER-positive/HER2-negative population, [PFS] rates at 6, 12, and 18 months showed a minority of patients achieving an 18-month PFS. Patients receiving sacituzumab govitecan had improved PFS compared with the treatment of physician’s choice at 6 and 12 months. The median PFS was 5.5 months in the sacituzumab govitecan arm vs 4 months in the treatment of physician’s choice arm, with a hazard ratio of 0.65 that was statistically significant. Overall survival (OS) was also improved with sacituzumab govitecan-hziy at 14 months vs 11 months with a hazard ratio of 0.79 that was also statistically significant.
An analysis based on HER2 immunohistochemistry status(1+ vs 0) showed similar benefits with sacituzumab govitecan compared with the physician’s choice in both PFS and OS.
TROP2 expression did not appear to be a predictive biomarker for sacituzumab govitecan efficacy in this ER-positive/HER2-negative population. Patients experienced similar benefits regardless of TROP2 status.
Dr Yeruva, are you able to comment on what you’ve seen with sacituzumab govitecan in your patients who are ER positive/HER2 negative, and when you might be using that [treatment]?
Yeruva / [For] my patients with HR-positive disease after the first line, in the duration of [CKD4/6] inhibitors, it’s dependent on that. We would like the molecular testing to look for PIK3CA mutations and ESR1 mutations to see if we can use any of those medications [that target] those mutations if none are [present]. If these patients have progressed quickly on the [CDK4/6] inhibitor and endocrine therapies, those would be the patients [who would] go on to the targeting of the HER2-low part of the tumor type. Regarding my experience right now, I have 2 patients doing very well on the sacituzumab govitecan in the HR-positive setting, 2 years [ongoing] with stable disease.
Puhalla / That’s a nice response. As far as the tolerability, have you seen that once you had a plan for neutropenia and diarrhea management, then it was smooth sailing for those patients?
Yeruva / It has been. One of my patients loves the medication. On the days she has to get off because of a vacation or a treatment break, she feels so poorly. Over all these years, she’s the one patient who has asked me to keep her on schedule with her treatments. She hates delaying [them] because she feels so good. We had a rough time initially with the management of the adverse effects, but after 2 or 3 months had gone by, [they began to resolve]. She’s been on it for 2 years and is doing [well].
Puhalla / What about compared with capecitabine? I would say capecitabine is always my go-to drug for ER-positive, metastatic disease. I realized that both of the ADCs, or all of the ADCs we have now with ER-positive disease, included capecitabine in their physician’s choice arm. Normally, I feel like I do get a much longer PFS from capecitabine, but I would say there are still a lot of patients [for whom] I’m going to go to that oral agent as a next step where you’re not getting the hair loss. I have some variability in hair loss with both T-DXd and with sacituzumab govitecan, but with capecitabine [hair loss] is typically well-tolerated. I would say that’s maybe the one situation where I might not go straight to an ADC when I’m looking at making that jump to chemotherapy for metastatic ER-positive disease.
Does anyone else have any thoughts on when you might go to the intravenous ADC vs going to something like capecitabine in your patients who [have] ER-positive [disease]?
Malhotra / We regularly go to capecitabine first, unless there’s a significant volume of disease or visceral crisis. I’ve had sacituzumab clear out the marrow twice, in people with their visceral crisis being the marrow. We have great efficacy with sacituzumab govitecan. I feel like the pace of disease picks up terribly once it’s resistant to the sacituzumab govitecan, though. We string that along as long as possible. There are only a few [options] after it, and I get much shorter disease-free survival with subsequent agents.
Deciding When to Use T-DXd
Puhalla / Specifically, looking at that HER2-ultralow population, you can see very similar [PFS] with 13.2 months with T-DXd vs 8.1 months with the physician’s choice.1 Then looking at this 12-month OS rate—84.0% with T-DXd compared with 78.7% [with the physician’s choice]—a lot of these patients are going to have years of OS after switching to chemotherapy. Importantly, [patients who are] HER2 ultralow did not do any worse compared with our standard [patients who are] HER2-low. It is important to try to push your pathologist to identify that small proportion of patients who are HER2 0, who could derive benefit.
Looking at adverse events, when you’re moving from endocrine therapy with CDK4/6 to an intravenous agent, this is something to think about. Nausea, everyone’s probably aware that the emetogenic potential of the drug has changed since it’s been approved…I do see fatigue, and I tend to do a lot of dose modification for fatigue, particularly in patients who’ve had a number of cycles and are getting tired. I’ve had a lot of variability in alopecia in my patients—I’ve had some patients who’ve not lost a single hair on their head…. Any-grade neutropenia [occurs in] up to 40% of patients but then we’re seeing [cases] higher than grade 3. I have had some patients [who] I’ve had to put on pegfilgrastim [Neulasta] with T-DXd if they need it, and that usually keeps them on track.
Looking at these patients who come off first-line CDK4/6 inhibitors who you’re concerned about and want to switch to T-DXd, [are there] any thoughts on efficacy and what you’re seeing in this group?
Swartz / I haven’t put anybody on T-DXd in the setting of CDK4/6 inhibitor and [aromatase inhibitor] progression. It’s always been after chemotherapy, but the data are impressive. I don’t think I would be opposed to trying it.
Latif / Generally, I try this medicine in the third or fourth line.
Lee / I started using it earlier. I haven’t used it in the [HER2- ultralow] setting yet, but certainly [in the] second line.
Lu / I had this one patient for the first line after a CDK4/6 inhibitor, but she had a [high] burden of disease so that propelled me to use [T-DXd] rather than capecitabine. Looking at the data though, I’m impressed. This is comparing standard single-agent chemotherapy, including capecitabine, and the outcome [with T-DXd] is better than with capecitabine in this setting. There was a post hoc analysis looking at PFS2 [time to second disease progression], and they looked at how the patient did after the first progression, and it seems like patients who receive T-DXd in the first line did better with their second and subsequent lines of therapy. I am more compelled to use T-DXd in the first line based on this data. Certainly, the quality of life, tolerability, and hair loss are all factors. For someone with a single bone progression, it would be capecitabine for me, but if they have a visceral metastasis or a bit heavier burden of disease, I would consider T-DXd in the first line.
Malhotra / The data, even in fast progressors and within 6 months of endocrine therapy, [show it] is working. That is very good to see. [They tell] me it works even with bad biology.
Puhalla / Everybody deserves a trial of T-DXd in their metastatic setting.... A couple of older, frailer ladies had been reluctant to use it, and then they progressed, and you just hate for somebody not to have tried it. Where I’ve pushed it off until later, before within my practice, I might be moving it up because I don’t want somebody not to be able to have it. Now, if you’ve got a couple of bone [metastases], probably not, but I think when you’ve switched into liver [metastases], or you’re seeing these faster progressors, it does make sense to push it up.
Toom / I had a patient who I was talking [to], and then I cut off [treatment]. Seven to 9 months into CDK4/6 [inhibitors in the] first line [with] de novo metastatic progress, she has bone-only progression, but that’s so significant that she’s having compression fraction. Her entire spine is full of metastases, she has a HER2 score of 2+, and she is [fluorescence in situ hybridization] negative. I spoke to her about all the options—I’m [thinking] BRCA mutation because she had somatic BRCA on [the Caris blood test], so I’m getting genetic [testing]. I’m looking for ESR1 and PIK3CA, but if she has none of those, my go-to is T-DXd, then capecitabine. Because she’s young, I want to see that benefit, and I discussed the DESTINY-Breast06 trial with her.
References
- Bardia A, Hu X, Dent R, et al. Trastuzumab deruxtecan after endocrine therapy in metastatic breast cancer. N Engl J Med. 2024;391(22):2110-2122. doi:10.1056/NEJMoa2407086
- Rugo HS, Bardia A, Marmé F, et al. Overall survival with sacituzumab govitecan in hormone receptor-positive and human epidermal growth factor receptor 2-negative metastatic breast cancer (TROPiCS-02): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2023;402(10411):1423-1433. doi:10.1016/S0140-6736(23)01245-X
- Kalinsky K, Accordino MK, Chiuzan C, et al. Randomized phase II trial of endocrine therapy with or without ribociclib after progression on cyclin-dependent kinase 4/6 inhibition in hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer: MAINTAIN trial. J Clin Oncol. 2023;41(24):4004-4013. doi:10.1200/JCO.22.02392
