Extranodal NK/T-Cell Lymphoma Misdiagnosed as Pulmonary Infection
This case report explores the diagnosis and treatment of extranodal NK/T-cell lymphoma, highlighting clinical challenges and advancements in pathology and therapy.
The authors
Abstract
Extranodal natural killer (NK)/T-cell lymphoma (ENKTL) is highly invasive. Its etiology and pathogenesis may be related to Epstein-Barr virus infection. In this article, we report a case of a man with ENKTL affecting the right vocal cord and right lung. Initially, the lesion was misdiagnosed as a pulmonary infection. However, subsequent histopathological examinations confirmed the diagnosis through analysis of a surgically resected specimen. Following 14 cycles of immune therapy and chemotherapy, the lesion in the right lung significantly shrank. This case underscored the importance of obtaining surgically resected specimens for pathology when ENKTL is suspected, which can improve diagnostic accuracy and mitigate misdiagnosis.
Introduction
The concept of extranodal natural killer (NK)/T-cell lymphoma (ENKTL) was initially proposed in 1996.1 In the 5th edition of the World Health Organization Classification of Hematolymphoid Tumors (WHO HAEM5), ENKTL is classified as a special type of Epstein-Barr virus (EBV)–positive NK/T-cell lymphoma in non-Hodgkin lymphoma (NHL), with the qualifier “nasal type” removed from its name.2 The etiology and pathogenesis of ENKTL may be closely linked to EBV infection and cytogenetic abnormalities. Risk factors also include working and living environment, as well as lifestyle.3 ENKTL cases can be categorized into those primarily occurring in the upper aerodigestive tract (UAT-ENKTL) and those primarily presenting outside the UAT (NUAT-ENKTL). The former typically manifests in the nasal cavity, nasopharynx, oropharynx, or Waldeyer ring, accounting for over 80% of all cases. The latter often presents in the skin, gastrointestinal tract, testis, lung, or liver, accounting for approximately 10% to 20% of total cases. NUAT-ENKTL demonstrates higher malignancy and poorer prognosis with lower overall survival (OS) and progression-free survival (PFS) compared with UAT-ENKTL.4,5 In this case report, we detailed a case of ENKTL, with the diagnosis ultimately confirmed through analysis of the surgically resected specimen. Additionally, we performed a literature review covering clinical and pathological characteristics, diagnosis, and treatment of ENKTL, aiming to enhance clinicians’ comprehension of this disease and minimize misdiagnoses.
Case report
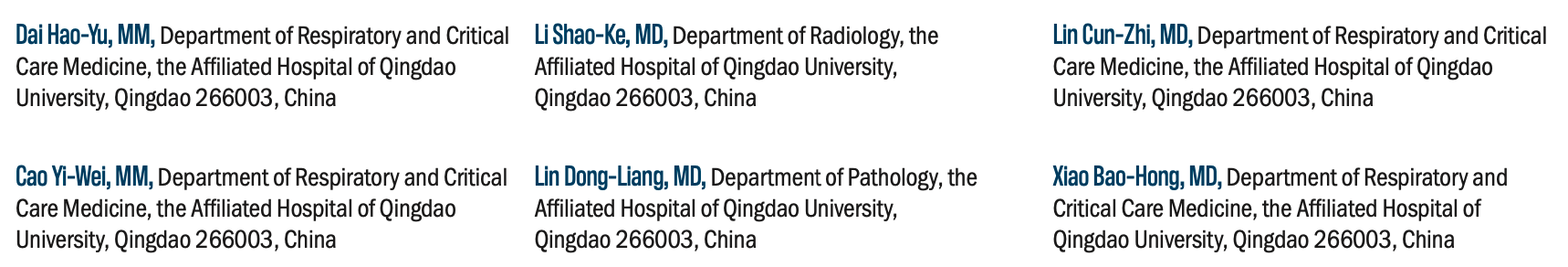
A 44-year-old man was admitted to the Affiliated Hospital of Qingdao University on October 24, 2020, due to “hoarseness of voice for more than 2 months.” Hoarseness initially appeared intermittently after the man drank alcohol and progressively worsened and became persistent. Electronic laryngoscopy revealed a right vocal cord tumor. The patient was healthy in the past and had no history of genetic predisposition to diseases. Physical examination did not reveal palpable superficial lymph nodes throughout the body, or enlarged liver and spleen. Peripheral blood tests of blood routine, liver and kidney function, electrolytes, thyroid tests, and male tumor markers showed no abnormalities. An enhanced CT scan of the neck indicated a space-occupying lesion on the right vocal cord and enlarged cervical lymph nodes (Figures 1A to 1C). The chest CT indicated an opacity in the right lung and slightly enlarged mediastinal lymph nodes (Figures 1D to 1I). Following the excision of the vocal cord lesion via suspension laryngoscopy, histopathological analysis demonstrated chronic inflammation in the mucosa with erosion and granulation tissue hyperplasia, and mildly atypical epithelium with bacterial clumps (Figures 1J to 1M). Bronchoscopy displayed white necrotic material adhering to the right vocal cord and obstructing the bronchial lumen of the posterior basal segment of the right lung. Transbronchial biopsy (TBB) from the posterior basal segment of the right inferior lobar bronchial mucosa showed atypical cells with large nuclei within the necrotic tissue (Figures 1L and 1N); however, it was difficult to make further diagnosis due to the low amount of tissue and severe necrosis (Figure 1). Subsequently, the patient was discharged.
FIGURE 1. CT Screening, Laryngoscopy, Bronchoscopy,
and Pathology in the First Admission
After being discharged, the patient developed an intermittently dry cough, accompanied by intermittent fever, with a maximum body temperature of 38 ℃, and was readmitted to the Affiliated Hospital of Qingdao University on November 6, 2020. Laboratory investigations showed the following results:
• Leukocyte count: 6.13×109/L (3.5-9.5×109/L)
• Eosinophil: 0.74×109/L (0.02-0.52×109/L)
• C-reactive protein (CRP): 32.99 mg/L (0-5mg/L)
• Ig E: 526.00 IU/mL (0-100IU/mL)
• IgG4: 0.80 g/L (0.03-2.01g/L)
• Absolute CD4 (+) T-cell count: 926.00 cells926.00 cells/μL (544~1212cells/μL)
• Serum lactate dehydrogenase (LDH): 251.0 U/L (120-250 U/L)
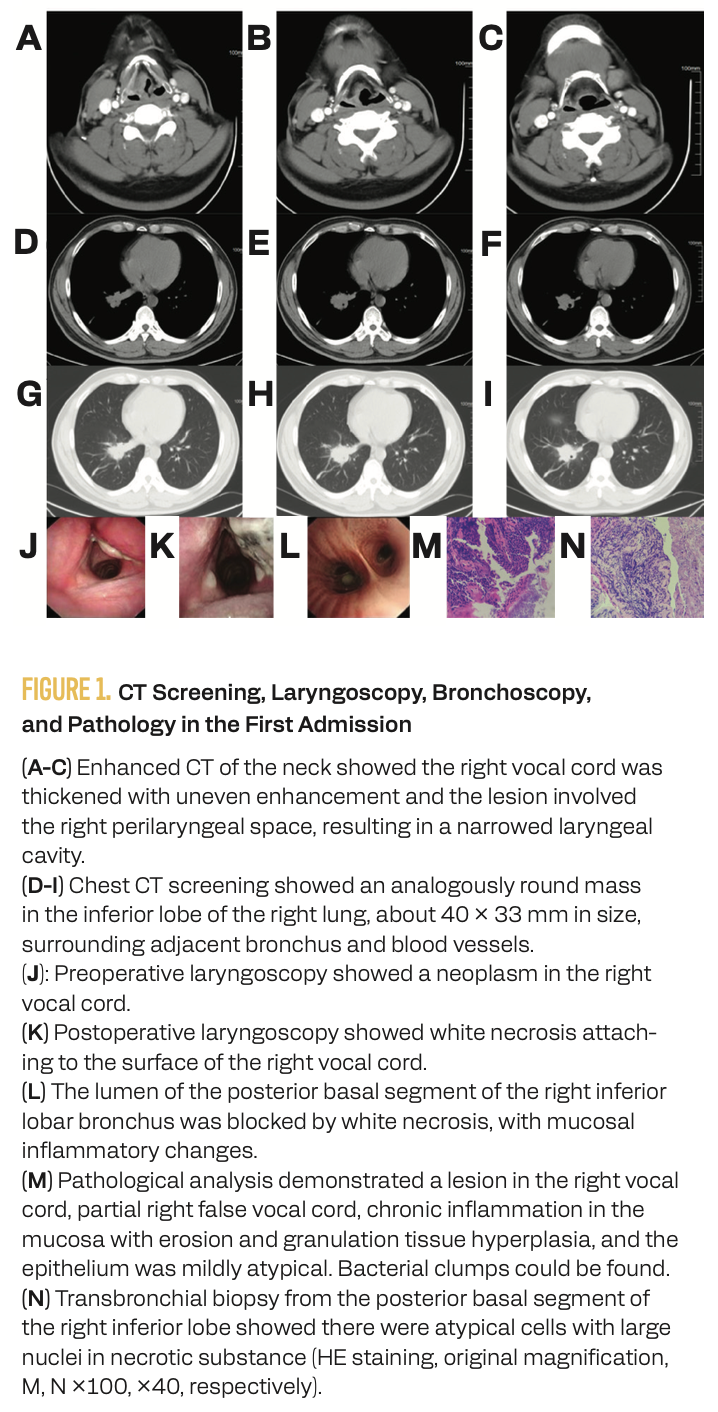
Autoantibodies such as extractable nuclear antigen (ENA), antinuclear antibodies (ANAs), antineutrophil cytoplasmic antibodies (ANCAs), and anticyclic citrullinated peptide antibody were negative. Given the presence of bacterial clumps in the biopsy obtained via laryngoscopy and that the patient had not previously received prior anti-infective therapy, moxifloxacin (400 mg once daily) was administered for 1 week (from November 6 to November 12, 2020). At the same time, a PET-CT scan was performed, and revealed the involvement of multiple systems and organs, suggesting the possibility of lymphoma, extensive metastasis of malignant tumors, or inflammatory diseases, such as tuberculosis (Figure 2). Pathological results from electronic bronchoscopy (TBB from the right inferior lobe) demonstrated a large number of necrotic and inflammatory exudates, with only a few bronchial mucosal tissues displaying chronic active inflammation (Figures 3A and 3B). Cells with large and hyperchromatic nuclei were found in the bronchoalveolar lavage fluid (BALF) of the inferior lobe of the right lung. A series of special stains, such as acid-fast bacteria staining, Grocott-Gomori methenamine-silver staining, mucicarmine staining, Gram staining, and periodic acid Schiff (PAS) staining, all yielded negative results. Next-generation sequencing (NGS) of BALF indicated Streptococcus constellatus. Hence, based on the bacterial susceptibility test, the patient was treated with piperacillin-tazobactam (4.5 g every 8 hours) in combination with moxifloxacin (400 mg once daily) for 5 days (from November 13 to November 17) and was discharged on November 18, 2020.
FIGURE 2. PET-CT Scan in the Second Admission
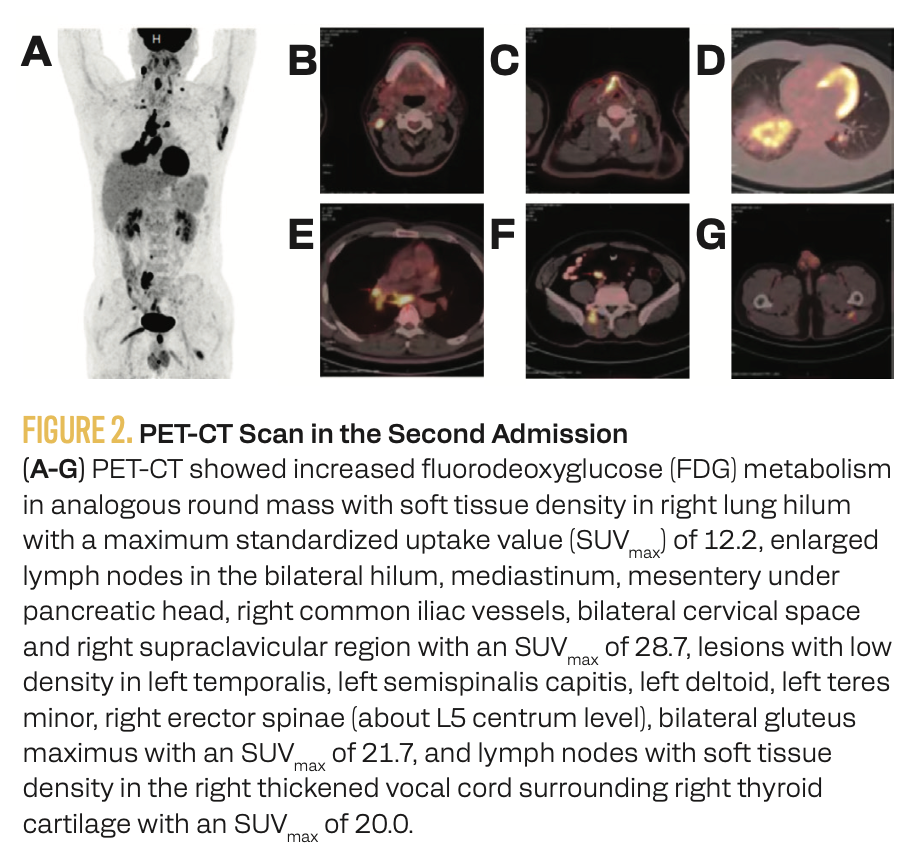
FIGURE 3. Bronchoscopy and Pathology in the Second Admission
After discharge, the patient experienced intermittent, low-grade fever. After anti-inflammatory treatment, the body temperature returned to normal levels. The patient was admitted for the third time on December 11, 2020. EBV antibody analysis revealed the following results:
• EBV-early antigen-IgG 33.54 AU/mL (< 2 AU/mL)
• EBV-viral capsid antigen (VCA)-IgA 4.34 AU/mL (< 4 AU/mL)
• EBV-VCA-IgG 104.2 AU/mL (< 2 AU/mL)
• EBV-nuclear antigen-IgG 48.25 AU/mL (<2 AU/mL)
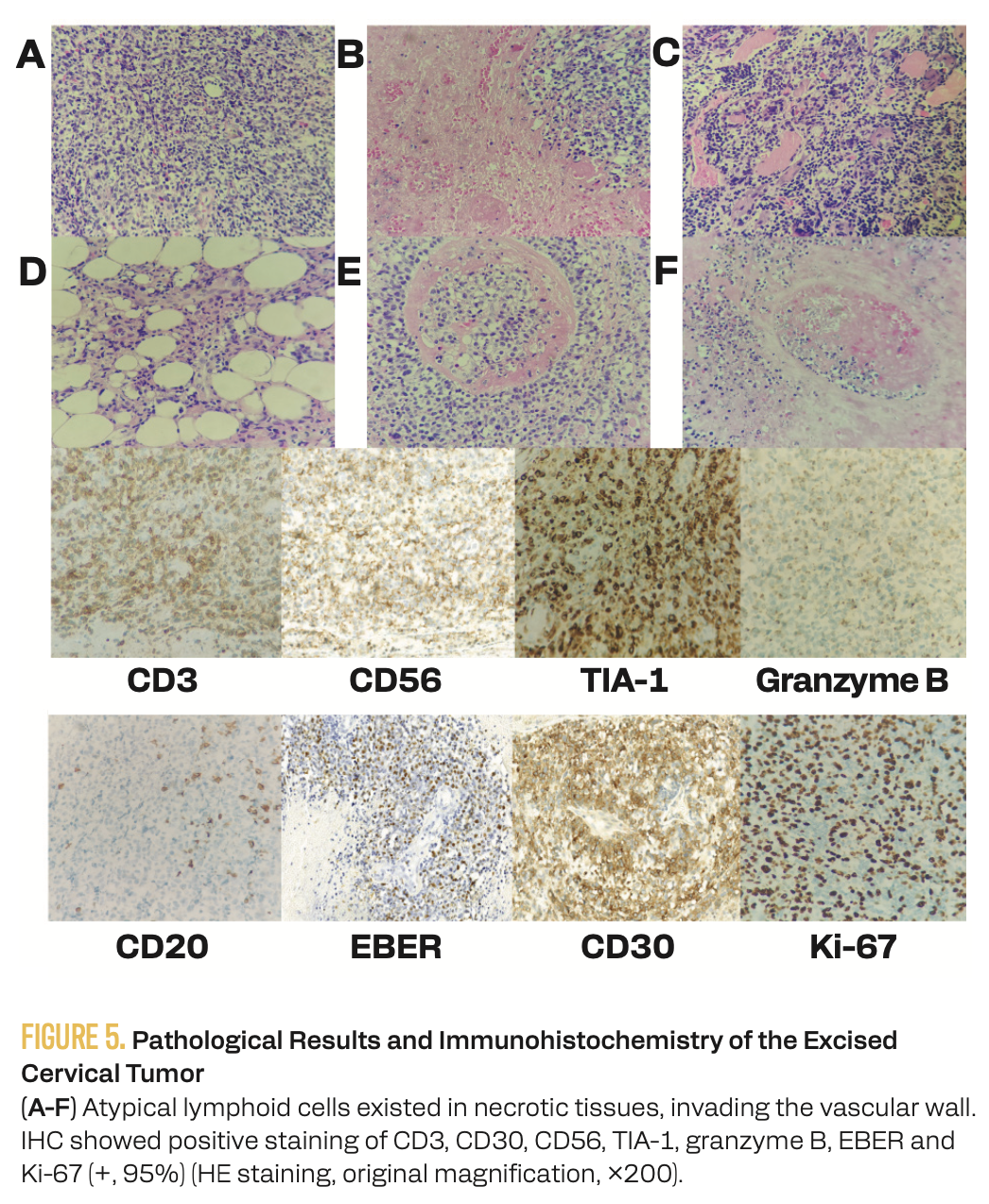
However, EBV DNA load in the whole blood was below the lower limit of detection, indicating that the patient might have been previously infected with EBV. Enhanced chest CT illustrated the progression of the right hilar space–occupying lesion (Figure 4). In view of the inadequate effect of previous anti-infective treatment, the application of antibacterial agents was halted. Subsequently, on December 24, 2020, right neck exploratory surgery and cervical tumor resection were performed. Pathology showed atypical lymphoid cells within areas of necrosis invading the vascular wall (Figures 5A to 5F). Immunohistochemistry (IHC) showed positive staining for CD3, CD30, CD56, TIA-1, and granzyme B, and negative staining for CD5, CD10, CD20, CD21, CD23, CD45RA, CD138, ALK (SP8), PAX5, and TDT. The Ki-67 hot spot region in the cells had a positive rate of 95%. Additionally, EBV-encoded small nuclear RNA (EBER) in situ hybridization was positive (Figure 5). The immunophenotypes were consistent with the diagnosis of ENKTL. The lesion in the right lung was considered to be of the same diagnosis. Bone marrow aspiration showed no tumor cell involvement. The patient was finally diagnosed as ENKTL, stage IV, with a nomogram-revised risk index (NRI) of 4 and a prognostic index of natural killer lymphoma (PINK) of 3.
FIGURE 4. Enhanced CT Screening of the Third Admission

FIGURE 5. Pathological Results and Immunohistochemistry of the Excised
Cervical Tumor
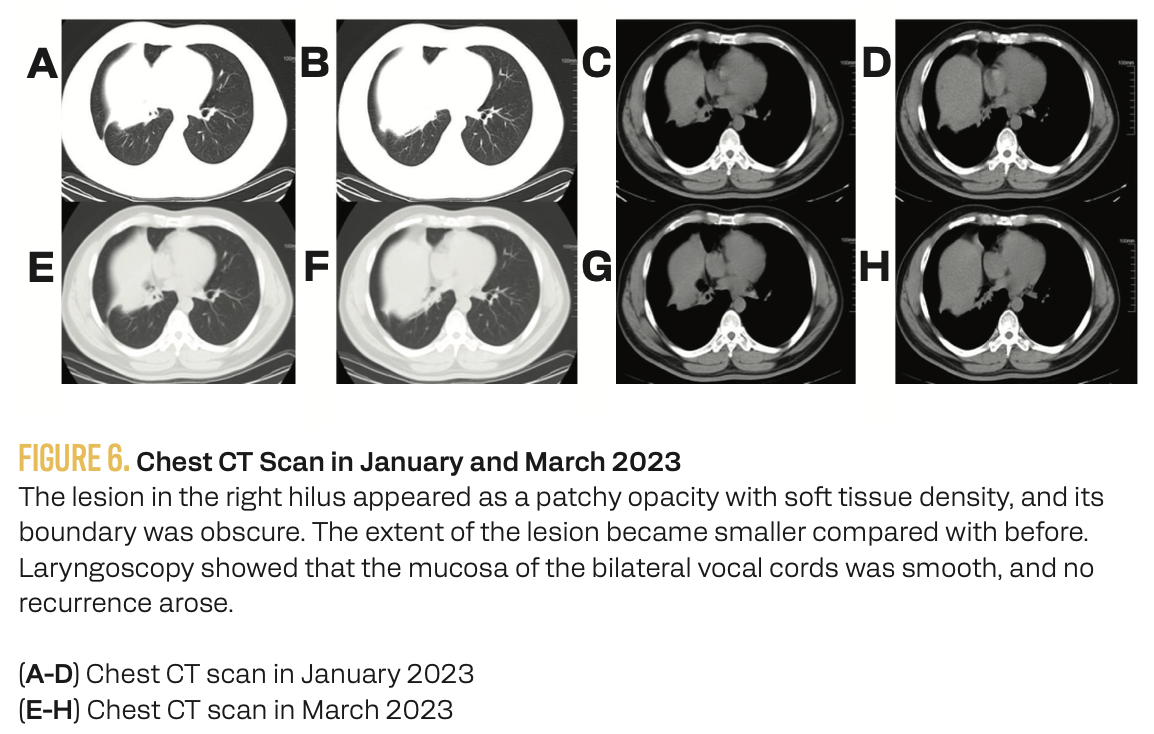
Later on, the patient underwent immunotherapy combined with chemotherapy for 14 cycles from January 2021. The treatment regimen from first to eighth cycles was sintilimab (200 mg on day 1) plus P-GemOx (pegaspargase 2000 IU day 1 plus gemcitabine 1000 mg on days 1 and 8 plus oxaliplatin 125 mg on day 1). The treatment regimen from 8th to 14th cycles was sintilimab (200 mg on day 1) plus chidamide (30 mg twice a week, and the dose was reduced to 15 mg from the 10th cycle). Sintilimab was applied every 3 months, and the dosage of chidamide was gradually reduced to 10 mg twice weekly. Periodic examination of whole blood EBV DNA load during the process of treatment revealed that it had been transiently elevated in November 2021 and December 2021, with exact values of 2.55 E+003 and 2.45E+002, respectively. Additionally, serum lactate dehydrogenase values were examined regularly during treatment and dropped to normal levels. Chest CT conducted in January and March 2023 indicated a remarkable reduction in the space-occupying lesion in the right lung and enlarged mediastinal lymph nodes (Figure 6). Upper abdomen, lower abdomen, and pelvis CT showed no discernible abnormalities or signs of recurrence.
FIGURE 6. Chest CT Scan in January and March 2023
Discussion
ENKTL is believed to originate from NK cells or γδT cells. The incidence is higher in East Asia and Latin America, constituting 2% to 15% of NHL, whereas it is less prevalent in Europe and North America, accounting for less than 1% of NHL.6 EBV infection may be closely associated with the onset of ENKTL. A clinical trial indicated that, compared with whole blood, evaluating EBV-DNA in the plasma provided a more accurate assessment of patient prognosis and response to treatment.7 Upregulation of cell proliferation–related signaling pathways, such as JAK-STAT and NF-κB signaling pathways, and mutation in antioncogenes, such as TP53, PRDM1, and FOXO3, may also play a role in the occurrence and development of ENKTL.6,8
18F-FDG PET-CT is increasingly utilized in both diagnosis and treatment due to its significant value in detecting metastases. A previous study indicated that 18F-FDG PET-CT had higher sensitivities and similar specificities in detecting early-stage ENKTL compared with nasopharyngeal MR.9 The definitive diagnosis of ENKTL relies on pathology. Pathologically, ENKTL is characterized by pleomorphic lymphocyte infiltration predominantly around blood vessels, often mixed with plasma cells, immunoblastic cells, eosinophils, and histiocytes, along with necrosis and vascular destruction. Immunological phenotypes often reveal positive staining of CD56, CD2, cytoplasmic CD3, CD43, TIA-1, granzyme B, EBER, and CD30 (partial), and negative staining of surface CD3 and CD5. A cohort study showed that there were no significant differences in OS and PFS between patients who were CD3 positive and CD30 negative, suggesting that whether CD30 staining was positive or not may not have a clear relationship to the prognosis of ENKTL.10
At present, 2 risk stratification models, the NRI and PINK, are mostly used for judgment of prognosis and guidelines for therapy.11,12 Recently, some biomarkers have been explored. A cohort study showed that plasma circulating tumor DNA sequence analysis could become a novel ENKTL tumor marker for genetic typing in the diagnosis of ENKTL, evaluating tumor burden, and monitoring patients’ response to therapy.13 Another study showed that EBV infection caused tumor cells to encode an oncoprotein called LMP1, which could upregulate the expression of CD70 in ENKTL tumor cells. With CD27 as the ligand for CD70, serum soluble CD27 (sCD27) in patients with ENKTL was significantly higher than that in healthy individuals, suggesting that sCD27 may serve as a novel biomarker for diagnosing and evaluating the application of CD27/CD70-targeted therapies.14
In terms of treatment, intensity-modulated radiotherapy and involved-site radiotherapy can limit the volume of radiation therapy (RT) to the region of involvement to a large extent, thereby reducing the damage to normal tissues and organs.15,16 High expression of P-glycoprotein leads to resistance to traditional anthracyclines.17 Most chemotherapy regimens are based on asparagine, such as the SMILE (dexamethasone, methotrexate, ifosfamide, L-asparaginase, and etoposide) or P-GemOx regimens.18 In a cohort study, 202 Chinese patients with early-stage ENKTL, the sequential P-GemOx regimen and RT achieved better outcomes than monotherapy.19 Another retrospective study found that the “sandwich” regimen of methotrexate, gemcitabine, Lasparaginase, and dexamethasone combined with RT showed better efficacy and lower toxicity in patients with localized ENKTL.20 PD-1 antibodies, such as sintilimab and pembrolizumab, are increasingly used in advanced or relapsed/refractory ENKTL, and have achieved satisfactory therapeutic effects.21,22 Chidamide, a histone deacetylase inhibitor, can inhibit ENKTL cell proliferation and promote cell apoptosis.23
In this case, the patient was first admitted to the department of otolaryngology and then the department of respiratory and critical care medicine due to respiratory symptoms, such as hoarseness, fever, and cough. Clinicians first considered the diagnosis as laryngocarcinoma, lung cancer, or lung infection according to the symptoms and imagological examinations. Some laboratory examinations and NGS of BALF suggested the possibility of infection. It might be related that patients with ENKTL were prone to immune system dysfunction, leading to opportunistic bacterial infection, such as S constellatus in BALF. However, anti-infection treatment did not achieve satisfactory effects. In other words, for some patients with fever of unknown origin, in conditions where anti-infective treatment did not have a satisfactory effect, clinicians need to take into consideration the possibilities of hematological disorders, such as ENKTL, etc. Later, PET-CT indicated multiple systemic involvements with a high possibility of malignancy. Therefore, this patient underwent pathological examinations, and the diagnosis was confirmed by surgical resection of the cervical tumor. IHC showed EBER in situ hybridization was positive.
The difficulties of pathological analysis may be associated with inflammation resulting from tumor cell necrosis. Because of a large amount of secretion and necrotic tissue on the surface of the tumor, more acute or chronic reactive inflammatory cells could be found under the microscope, and tumor cell infiltration was difficult to find. Therefore, although some atypical cells could be found at the edge of the tissues, typical pathological characteristics of ENKTL were difficult to find. In the meanwhile, although bronchoscopy, a minimally invasive and relatively safe operation, has been widely used in the diagnosis of lung tumors, it is important for us to realize the limitations, for example, small amounts of tissue obtained, which might cause difficulties for pathologists to observe typical pathological changes. The small amounts of biopsied tissues, as well as the extrusion and deformation of the tissues, led to difficulties in pathologic diagnosis.
Therefore, for suspected patients with ENKTL, in the process of biopsy, clinicians should be aware of the following: first, if available, surgical resection specimens are preferred because only a small number of samples can be obtained through needle or endoscopic biopsy, leading to difficulty in diagnosis. If clinicians have difficulty obtaining surgical resection specimens and have to perform needle biopsy or endoscopic biopsy, they should be aware that tissues on the surface may exhibit chronic inflammation. Therefore, necrosis needs to be removed first, and tissues from multiple sites should be taken repeatedly from the junction of necrosis and diseased tissues to maximize the accuracy of the biopsy. Second, axillary lymph nodes and inguinal lymph nodes should be avoided for pathological examination, because these sites are susceptible to physiological factors, and the structure of these lymph nodes is complex. Third, lymph nodes or diseased tissues with high 18F-FDG metabolism on PET-CT or large size should be selected to take biopsies first. Last, biopsy specimens should be fixed in 3.7% neutral formaldehyde in time (no more than 30 minutes after separation) and extrusion should be avoided. The operation should be gentle and the use of the electrotome should be avoided, because tissues are easily damaged and seriously deformed, affecting the accuracy of diagnosis. In conclusion, surgical resection specimens should be obtained as much as possible to improve the accuracy of diagnosis and reduce misdiagnosis and missed diagnosis.
Declaration
The author(s) declared that there were no potential conflicts of interest with respect to the article, authorship, and/or publication of this article. Consent for publication have been obtained from the patient. No funding was received. Acknowledgements are not applicable. The data or images used and/or analyzed during the article are available from the corresponding author on reasonable request. DHY was the major contributor in writing the original manuscript. CYW and LSK provided and analyzed the medical records of the patient. LDL performed pathological analysis of the patient. LCZ and XBH confirmed the authenticity of all the data and images in this manuscript and were responsible for editing and reviewing. All authors read and approved the final manuscript. Ethics approval and consent to participate are not applicable.
Author affiliations
Dai Hao-Yu, MM
Department of Respiratory and
Critical Care Medicine, the Affiliated
Hospital of Qingdao University,
Qingdao 266003, China,
E-mail: dai9827@126.com
Cao Yi-Wei, MM
Department of Respiratory and
Critical Care Medicine, the Affiliated
Hospital of Qingdao University,
Qingdao 266003, China,
E-mail: cyw13198@163.com
Li Shao-Ke, MD
Department of Radiology,
the Affiliated Hospital of Qingdao University,
Qingdao 266003, China,
E-mail: lsk224@163.com
Lin Dong-Liang, MD
Department of Pathology,
the Affiliated Hospital of Qingdao University,
Qingdao 266003, China,
E-mail: lindongliang@outlook.com
Lin Cun-Zhi, MD
Department of Respiratory and
Critical Care Medicine, the Affiliated
Hospital of Qingdao University,
Qingdao 266003, China,
E-mail: lindoc@126.com
Corresponding Author:
Xiao Bao-Hong, MD
Department of Respiratory and
Critical Care Medicine, the Affiliated
Hospital of Qingdao University,
16 Jiangsu Road,
Qingdao 266003, China,
E-mail: xiao-1997@outlook.com
References
- Jaffe ES, Chan JK, Su IJ, et al. Report of the workshop on nasal and related extranodal angiocentric T/natural killer cell lymphomas. Definitions, differential diagnosis, and epidemiology. Am J Surg Pathol. 1996;20(1):103-111. doi:10.1097/00000478-199601000-00012
- Alaggio R, Amador C, Anagnostopoulos I, et al. The 5th edition of the World Health Organization Classification of haematolymphoid tumours: lymphoid neoplasms. Leukemia. 2022;36(7):1720-1748. doi:10.1038/s41375-022-01620-2
- Sanchez-Romero C, Bologna-Molina R, Paes de Almeida O, et al. Extranodal NK/T cell lymphoma, nasal type: an updated overview. Crit Rev Oncol Hematol. 2021;159:103237. doi:10.1016/j.critrevonc.2021.103237
- Au WY, Weisenburger DD, Intragumtornchai T, et al. Clinical differences between nasal and extranasal natural killer/T-cell lymphoma: a study of 136 cases from the International Peripheral T-Cell Lymphoma Project. Blood. 2009;113(17):3931-3937. doi:10.1182/blood-2008-10-185256
- Fox CP, Civallero M, Ko YH, et al. Survival outcomes of patients with extranodal natural-killer T-cell lymphoma: a prospective cohort study from the international T-cell Project. Lancet Haematol. 2020;7(4):e284-e294. doi:10.1016/s2352-3026(19)30283-2
- Montes-Mojarro IA, Fend F, Quintanilla-Martinez L. EBV and the pathogenesis of NK/T cell lymphoma. Cancers (Basel). 2021;13(6): 1414. doi:10.3390/cancers13061414
- Ha JY, Cho H, Sung H, et al. Superiority of Epstein-Barr virus DNA in the plasma over whole blood for prognostication of extranodal NK/T cell lymphoma. Front Oncol. 2020;10:594692. doi:10.3389/fonc.2020.594692
- de Mel S, Hue SS, Jeyasekharan AD, Chng WJ, Ng SB. Molecular pathogenic pathways in extranodal NK/T cell lymphoma. J Hematol Oncol. 2019;12(1):33. doi:10.1186/s13045-019-0716-7
- Guo R, Xu P, Cheng S, et al. Comparison of nasopharyngeal MR, 18F-FDG PET/CT, and 18F-FDG PET/MR for local detection of natural killer/T-cell lymphoma, nasal type. Front Oncol. 2020;10:576409. doi:10.3389/fonc.2020.576409
- Kawamoto K, Miyoshi H, Suzuki T, et al. Frequent expression of CD30 in extranodal NK/T-cell lymphoma: potential therapeutic target for anti-CD30 antibody-based therapy. Hematol Oncol. 2018;36(1):166-173. doi:10.1002/hon.2482
- Chen SY, Yang Y, Qi SN, et al. Validation of nomogram-revised risk index and comparison with other models for extranodal nasal-type NK/T-cell lymphoma in the modern chemotherapy era: indication for prognostication and clinical decision-making. Leukemia. 2021;35(1):130-142. doi:10.1038/s41375-020-0791-3
- Kim SJ, Yoon DH, Jaccard A, et al. A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: a multicentre, retrospective analysis. Lancet Oncol. 2016;17(3):389-400. doi:10.1016/S1470-2045(15)00533-1
- Kim JJ, Kim HY, Choi Z, et al. In-depth circulating tumor DNA sequencing for prognostication and monitoring in natural killer/T-cell lymphomas. Front Oncol. 2023;13:1109715. doi:10.3389/fonc.2023.1109715
- Nagato T, Komatsuda H, Hayashi R, et al. Expression of soluble CD27 in extranodal natural killer/T-cell lymphoma, nasal type: potential as a biomarker for diagnosis and CD27/CD70-targeted therapy. Cancer Immunol Immunother. 2023;72(7):2087-2089. doi:10.1007/s00262-023-03394-7
- Qi SN, Li YX, Specht L, et al. Modern radiation therapy for extranodal nasal-type NK/T-cell lymphoma: risk-adapted therapy, target volume, and dose guidelines from the international lymphoma radiation oncology group. Int J Radiat Oncol Biol Phys. 2021;110(4):1064-1081. doi:10.1016/j.ijrobp.2021.02.011
- Wu T, Yang Y, Zhu SY, et al. Risk-adapted survival benefit of IMRT in early-stage NKTCL: a multicenter study from the China Lymphoma Collaborative Group. Blood Adv. 2018;2(18):2369-2377. doi:10.1182/bloodadvances.2018021311
- Xue W, Zhang M. Updating targets for natural killer/T-cell lymphoma immunotherapy. Cancer Biol Med. 2021;18(1):52-62. doi:10.20892/j.issn.2095-3941.2020.0400
- Horwitz SM, Ansell S, Ai WZ, et al. T-cell lymphomas, version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2022;20(3):285-308. doi:10.6004/jnccn.2022.0015
- Zhang Y, Ma S, Cai J, et al. Sequential P-GEMOX and radiotherapy for early-stage extranodal natural killer/T-cell lymphoma: a multicenter study. Am J Hematol. 2021;96(11):1481-1490. doi:10.1002/ajh.26335
- Chaubard S, Marouf A, Lavergne D, et al. Efficacy of a short sandwich protocol, methotrexate, gemcitabine, L-asparaginase and dexamethasone chemotherapy combined with radiotherapy, in localised newly diagnosed NK/T-cell lymphoma: a French retrospective study. Br J Haematol. 2023;201(4):673-681. doi:10.1111/bjh.18689
- Tao R, Fan L, Song Y, et al. Sintilimab for relapsed/refractory extranodal NK/T cell lymphoma: a multicenter, single-arm, phase 2 trial (ORIENT-4). Signal Transduct Target Ther. 2021;6(1):365. doi:10.1038/s41392-021-00768-0
- Li X, Cheng Y, Zhang M, et al. Activity of pembrolizumab in relapsed/refractory NK/T-cell lymphoma. J Hematol Oncol. 2018;11(1):15. doi:10.1186/s13045-018-0559-7
- Zhou J, Zhang C, Sui X, et al. Histone deacetylase inhibitor chidamide induces growth inhibition and apoptosis in NK/T lymphoma cells through ATM-Chk2-p53-p21 signalling pathway. Invest New Drugs. 2018;36(4):571-580. doi:10.1007/s10637-017-0552-y
Highlighting Insights From the Marginal Zone Lymphoma Workshop
Clinicians outline the significance of the MZL Workshop, where a gathering of international experts in the field discussed updates in the disease state.