Fall Risk Assessment and Prevention
Patient falls are a common cause of morbidity and are the leading cause of injury deaths in adults age 65 years and older. Injuries sustained as result of falls in a cancer hospital are often severe, regardless of patient age, due to the nature of the underlying cancer.
ABSTRACT: Patient falls are a common cause of morbidity and are the leading cause of injury deaths in adults age 65 years and older. Injuries sustained as result of falls in a cancer hospital are often severe, regardless of patient age, due to the nature of the underlying cancer. Falls are a nursing-sensitive indicator and nurses are in a unique position to assess, design, implement, and evaluate programs for fall risk reduction. We analyzed our nursing processes related to falls and fall prevention in conjunction with an evidence-based review, a research study to improve our fall risk–assessment process, and development of a comprehensive fall-reduction program. This article outlines how our institution developed a fall risk assessment for the oncology patient population, and utilized this assessment in a comprehensive nursing approach to fall prevention in both inpatient and outpatient settings.
Patient falls are the most frequently reported adverse event in hospitals, and they are the leading cause of injury deaths in adults 65 years of age and older.[1,2] Injuries sustained as result of patient falls in a cancer hospital are often severe, due to the nature of the underlying medical condition. For example, patients may be predisposed to fractures because of bony metastases or to uncontrollable bleeding from thrombocytopenia or medications used to prevent deep vein thrombosis. In 2005, our institution prioritized patient falls as one of the most important safety threats to our patients. Falls are a nursing-sensitive indicator and nurses are in a unique position to assess, design, implement, and evaluate programs for fall risk reduction. We analyzed our current nursing processes related to falls and fall prevention in conjunction with an evidence-based review, a research study to improve our falls risk–assessment process, and development of a comprehensive fall-reduction program.

Instrument Development and Testing
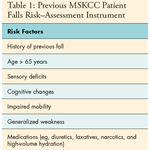
At the time the project started, it became apparent that the instrument that we were using to assess falls risk had been used for many years in the institution without any scientific rationale (Table 1). We therefore conducted an evidence-based review to identify reliable and valid falls risk–assessment instruments to consider adopting for use. Because the vast majority of these instruments were developed for use in long-term-care facilities, however, we decided that they were not useful for our acute-care population, as we had determined that the median age of our adult patients who were falling was 56 years (range, 21–91 years).
To facilitate the development of a falls risk–assessment instrument appropriate for our patient population, we conducted a case-control study to determine risk factors: each of the 73 patients who fell in the first quarter of 2005 was matched with 2 patients of the same age (± 2 years) from the same nursing unit (indicating a similar diagnosis). In total, the charts of 219 patients (73 cases, 146 controls) were reviewed. A list of variables was developed from factors commonly named in the literature as well as those identified in clinical practice. The list included gender; number of secondary diagnoses; hearing loss; cognitive impairment; cognitive impairment within 48 hours of fall; motor deficits; procedure within 48 hours of fall; use of assistive devices; history of falls within the past year; intravenous fluid; high-volume hydration within 48 hours of fall; use of patient-controlled analgesics; medical equipment attached to the patient (IV pole, chest tube, Foley catheter, etc); number of medications; and presence of psychotropic, antihypertensive, anticonvulsant, diuretic/cathartic, narcotic, and/or analgesic medications.[3]
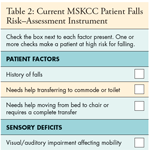
The pilot instrument was tested from February to June 2006 on four inpatient units (neurology/orthopedics, leukemia/lymphoma, gastrointestinal surgery, head and neck). In addition, assessment using the Katz Index of Independence in Activities of Daily Living was performed on all patients. The Katz Index assesses activities of daily living-bathing, dressing, toileting, transferring, continence, and feeding-by assigning one point for independent completion of each activity.[4] Patients with higher Katz scores are considered to be more independent, and thus, it is hypothesized, less likely to fall. Inter-rater reliability of the pilot instrument was 87%. A second prospective case-control study was conducted during the pilot, and statistically significant variables from the first case-control study were reconfirmed and used in development of the final instrument (Table 2).[3]
The Memorial Sloan-Kettering Cancer Center Falls Risk Assessment instrument is not scored or summed. Intuitively it did not make sense to try to assign points to each of the risk factors and calculate a cut score to determine risk for falling if the results suggested that each variable increased the patient’s risk of falling. We found that the positive-predictive value (PPV) of the new instrument was 91%, whereas the PPV of the previous instrument was 66%, indicating that we were now able to assess patient risk for falling much more accurately.[3]
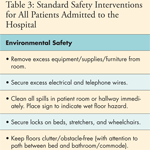
While the new instrument was an improvement in identifying patients at risk for falls, this alone was not going to reduce falls: targeted interventions for specific risk variables were clearly needed. The nursing care plan for the patient at high-risk of falling was thus revised. Standard safety interventions were designated for all patients and grouped into categories: environmental safety, patient safety, and daily routines (Table 3). Specific interventions were added for the high-risk patient according to risk factor category from the new instrument (Table 4). Subsequently, a patient safety program was initiated in March 2007. The aim of this program was to provide intensive training regarding patient safety. Program content included the design and implementation of a new model of care delivery to reduce patient falls and falls with injury.
Inpatient Safety Program Agenda
The overriding goal of the program was to identify the staff’s responsibilities in ensuring patient safety. The four objectives that drove the agenda were describing elements of a safe culture and the internal and external forces that influence patient safety; discussing latent issues that contribute to unsafe patient conditions; discussing the responsibilities of team members in ensuring patient safety through teamwork, communication, and delegation; and describing changes in practice to improve patient safety. The team designed a full-day training agenda that included morning didactic presentations with small group activities in the afternoon. Didactic presentations covered safety and change theory, unit-specific falls and falls with injury data, teamwork, accountability, communication, delegation, and a unit-specific safety model. In the afternoon, the small groups spent time studying patient scenarios to identify safety hazards and developing interventions for the unit-specific patient safety model.[3] The safety program was conducted throughout all inpatient units between 2007 and 2008. Overall patient falls rates have decreased from 5.8/1,000 patient days in Q2 2007 to 2.79/1,000 patient days as of Q4 2010. Falls with moderate to severe injury rates are 0.82/1,000 patient days as of Q4 2010.
Ambulatory Falls Program
In mid-2007, a representative group of ambulatory nurses formed a task force to develop a falls-prevention program targeted to outpatients. The goal was to complement the inpatient program and ensure communication of falls risk throughout our institution. Using an evidence-based methodology, the group reviewed the literature, the published guidelines, and the standards of care from other organizations regarding outpatient falls risk assessment, but little was applicable to the ambulatory oncology setting. Standard nursing interventions and safety precautions were developed for all ambulatory patients.
Uniform identification and screening for patients at high risk of falling was more difficult. All reports on falls within ambulatory for the past year were reviewed and the risk factors were found to be similar to those of inpatients. Most outpatient falls were related to toileting or patient history of sensory or motor deficits, so a decision was made to use the MSKCC falls risk–assessment tool. This instrument was translated to a patient-report format, to be more compatible with our ambulatory nursing practice model rather than traditional RN assessment. Pilot testing on 66 patients with nurse assessment and patient self-assessment was conducted in July 2007 in six ambulatory clinics (radiation oncology, neurology, breast medicine, gynecologic surgery, chemotherapy, and a medical oncology practice at one of our regional sites). Inter-rater reliability (nurse assessment vs patient self-report) was established at 97%, indicating that the instrument could be completed accurately by patients.
Guidelines for initial and ongoing ambulatory falls risk–assessment now needed to be established. For inpatients, falls risk–assessment during every shift is commonplace; the question of how often to assess outpatients, however, was difficult to determine. As little information was available from the literature, it was decided that ambulatory falls risk–assessment would be incorporated into our newly revised Adult Ambulatory Health Screening tool, used to assess a variety of patient risk factors and initiate appropriate referrals. This tool is completed by all patients who are new to our institution, by patients at the time of a change in treatment modality (ie, a patient who has had surgical resection and is starting adjuvant chemotherapy or radiation therapy), or on an as-needed basis, based on clinician discretion (ie, due to disease progression, change in mental status, or significant life change). A positive answer to any of the identified falls risk factors requires nursing action. The use of psychotropic medications (those for anxiety or seizures, or sleeping pills) is a factor to be considered, but it was not selective enough for outpatients to be designated as a significant risk factor by itself. In ongoing follow-up of ambulatory patient falls, these medications have not been observed to contribute to patient falls.
Once a patient is identified as being at high risk of falling, interventions are implemented based on the specific identified risk. Patients and their families are educated about the risk and our falls-prevention patient education card is provided and reviewed. Patients are also "flagged" in our electronic chart. The risk flag is displayed in the header of our electronic chart and is readily visible to all staff, both inpatient and in ambulatory. The flag, which lists specific risk factors for falls (eg, neuropathy, motor weakness), can be removed when the falls risk is resolved.
Conclusions
Our approach to fall prevention is evidence-based, comprehensive, and evolving. Currently all new hires (nurses and assistive personnel) receive the didactic portion of the program as a half-day session during orientation. Patient falls and falls with injury data are provided to each nursing unit on a quarterly basis and "days since last fall" are posted on an internal hospital dashboard so that staff can see how their data compare to national benchmarks and other nursing units within the institution. Since the inception of our online event-reporting system in May 2007, we have access to consistent data regarding each patient fall and the narrative description of each event. A Falls Reading Group meets quarterly to review every fall within the institution to assure accurate reporting of severity level. We recently acquired SPSS Text Analytics for Surveys, and moving forward will able to identify trends in the narrative reports.
While the "nursing" part of this program (patient assessment, education, and risk-reduction interventions) is now well established, our plan is to broaden our program to educate and include nonclinical staff. We are developing standard falls risk–and-prevention training program and establishing ongoing interventions to enhance communication, with the goal of empowering all staff with fall-prevention strategies. We hope to create a hospital-wide culture of safety by preventing patient falls and falls with injury.
We acknowledge the contributions of those who developed the patient safety program and who continue to educate staff: Patricia Brosnan, MPH, RN, Wayne Quashie, MSN, MPH, RN, OCN, and the Ambulatory Nursing Team who have implemented the falls program in the outpatient setting.
References:
References1. Eldridge C: Evidence-based Falls Prevention: A Study Guide for Nurses. Marblehead, Massachusetts, HCPro, 2004.
2. Centers for Disease Control and Prevention: Falls Among Older Adults: An Overview. June 2007. Available at: http://www.cdc.gov/ncipc/factsheets/adultfalls.htm. Page last reviewed on September 13, 2010. Page last updated on December 8, 2010. Accessed on January 21, 2011.
3. Kline NE, Thom B, Quashie W, et al: A model of care delivery to reduce falls in a major cancer center, in Henricksen K, Battles JB, Keyes MA, et al (eds): Advances in Patient Safety: New Directions and Alternative Approaches. vol 1. Assessment AHRQ Publication No. 08-0034-1. Rockville, MD, Agency for Healthcare Research and Quality, 2008.
4. Katz S, Ford AB, Moskowitz RW, et al: Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA 185:914â919, 1963.