FDA Approval Alert: Amivantamab Plus Chemotherapy in Non-Small Cell Lung Cancer
Misako Nagasaka, MD, PhD, discussed the approval of amivantamab plus chemotherapy for patients with EGFR exon 20 insertion mutations non–small cell lung cancer.
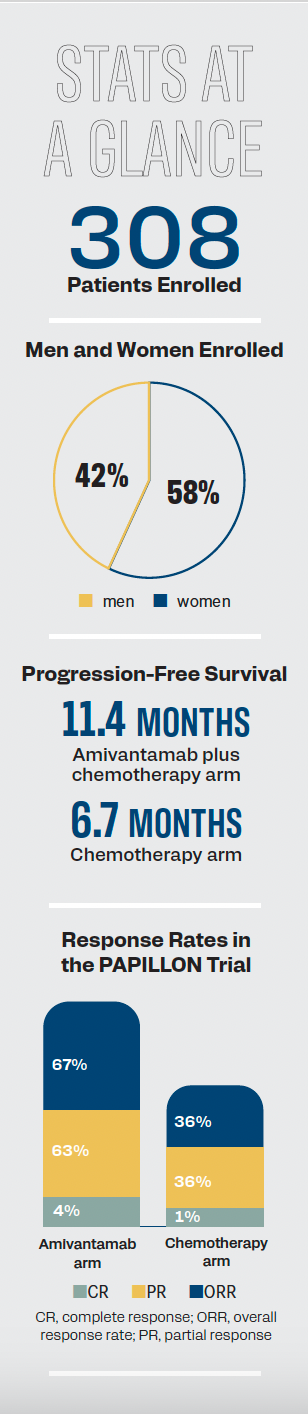
Statistics from the phase 3 PAPILLON trial.
In March 2024, the FDA approved frontline amivantamab-vmjw (Rybrevant) in combination with carboplatin and pemetrexed for adult patients with locally advanced or metastatic non–small cell lung cancer (NSCLC) harboring EGFR exon 20 insertion mutations.1 ONCOLOGY spoke with Misako Nagasaka, MD, PhD, associate clinical professor, Division of Hematology/Oncology, University of California, Irvine, and thoracic malignancies editorial advisory board member of ONCOLOGY, regarding the recent approval.
Q / How did the results of the PAPILLON trial help lead to
the approval?
Nagasaka / The phase 3 PAPILLON study [NCT04538664] was a study dedicated to patients with EGFR exon 20 insertions. This is a rare subtype of EGFR mutations that do not respond to the usual EGFR tyrosine kinase inhibitors, which is the default for sensitizing mutations [such as EGFR] exon 19 deletion or L858R. PAPILLON compared amivantamab plus chemotherapy with chemotherapy alone, and it [showed] positive [results]. Subsequently on March 1, 2024, that PAPILLON regimen gained FDA approval.
A total of 308 patients [were randomly assigned,] with 153 receiving amivantamab plus chemotherapy and 155 receiving chemotherapy alone. The progression-free survival [PFS] was significantly longer in the amivantamab plus chemotherapy group than in the chemotherapy [alone] group. The median PFS was 11.4 months in the amivantamab plus chemotherapy group and 6.7 months in the chemotherapy group. The hazard ratio for disease progression or death was 0.40. The overall response rates were 73% vs 47%, respectively. In the interim overall survival analysis, which was only at 33% maturity, the hazard ratio for deaths for amivantamab plus chemotherapy as compared with chemotherapy was 0.67. It’s trending in the right direction.
Q / What patient population is specified for this treatment combination?
Nagasaka / This is for [patients with] EGFR exon 20 insertion mutations. This indication is for the first line, and there are some patients who have not been treated previously, based on the forest plots that were available in The New England Journal of Medicine publication.2 Among all of the subgroups, whether it be gender, race, history of smoking, or having brain metastases or not, all of the subgroups benefited more from amivantamab and chemotherapy.
Q / Were any significant adverse effects (AEs) observed in the combination compared with standard-of-care chemotherapy?
Nagasaka / The predominant toxicities or AEs associated with amivantamab and chemotherapy were reversible hematologic changes and EGFR-related toxic events such as rash. Only 7% of patients discontinued amivantamab owing to AEs. When we think of amivantamab, we might think about infusion-related reactions. The rate of this was 42% in those in the amivantamab and chemotherapy group, and it was lower than what we saw in the phase 1 CHRYSALIS study [NCT02609776], probably due to the premedications that we give for chemotherapy.3 The rates of chemotherapy-related AEs such as febrile neutropenia were similar, so [there were] no additional chemotherapy-related AEs. Having treated patients on the combination using amivantamab, I feel that long-term rash management is most important.
Q / How did the efficacy of this combination compare with other targeted therapies that are now emerging for this population in the frontline setting?
Nagasaka / Looking at the PFS, this combination of amivantamab plus chemotherapy for first-line therapy and patients with EGFR exon 20 insertion is a fantastic result that we have. However, it is intravenous therapy, and it is combined with chemotherapy. We have to be cognizant of that. The overall survival data are not matured yet, but hopefully, we will see more data come through for the overall survival as well. The difficulty is that outside of EXCLAIM-2 [NCT04129502], which was the phase 3 study using mobocertinib [Exkivity] vs chemotherapy,4 I do not believe we have mature data on first-line specific treatment options for patients with EGFR exon 20 insertion, and as we all know, the EXCLAIM-2 study failed. There was no difference between using mobocertinib vs chemotherapy in the frontline setting.
Q / What are the next steps for this combination?
Nagasaka / Mobocertinib did fail the study, but it was an oral regimen. Having a pill option is an advantage to patients. Hopefully, the axis of the medications will get easier. As far as amivantamab and PAPILLON go, [researchers] are developing a subcutaneous version of amivantamab. That might decrease the time required to be at the infusion site, although we’re combining this with chemotherapy anyway. It’s not going to be a chemotherapy-free option. Overall, the long-term toxicities of rash management are…important to find out.
References
- FDA approves amivantamab-vmjw for EGFR exon 20 insertion-mutated non-small cell lung cancer indications. News release. FDA. March 1, 2024. Accessed March 1, 2024. https://tinyurl.com/msw4u5yk
- Zhou C, Tang K, Cho BC, et al; PAPILLON Investigators. Amivantamab plus chemotherapy in NSCLC with EGFR exon 20 insertions. N Engl J Med. 2023;389(22):2039-2051. doi:10.1056/NEJMoa2306441
- Park K, Haura EB, Leighl NB, et al. Amivantamab in EGFR exon 20 insertion–mutated non–small-cell lung cancer progressing on platinum chemotherapy: initial results from the CHRYSALIS phase I study. J Clin Oncol. 2021;39(30):3391-3402. doi:10.1200/JCO.21.00662
- Jänne PA, Wang BC, Cho BC, et al. EXCLAIM-2: phase III trial of first-line (1L) mobocertinib versus platinum-based chemotherapy in patients (pts) with epidermal growth factor receptor (EGFR) exon 20 insertion (ex20ins)+ locally advanced/metastatic NSCLC. Annal Oncol. 2023; 34(suppl 4):S1663-S1664. doi:10.1016/j.annonc.2023.10.586