Geographical Information Systems: Applications and Limitations in Oncology Research
This review describes the development and technical capabilities of GIS, potential applications of Geographical Informational Systems in cancer research, and the limitations of such work.
The relationship between geography and cancer incidence and treatment is a critical area of health outcomes research. Geographical information systems (GIS) are software packages designed to store and analyze data related to geographic locations. Although more commonly associated with the social sciences and urban planning, the use of GIS software in medical research has been increasing.[1] Moreover, since the 1999 establishment of the Geographical Informational Systems Special Interest Group (GISSIG) at the National Cancer Institute, oncology has been at the forefront of GIS-related health research. In this review, we discuss the potential applications and limitations of GIS software in oncology research. Our aims are to help clinicians and policy makers interpret studies generated using GIS, and to help clinical investigators implement GIS in future research.
Introduction
The relationship between geography and cancer incidence and treatment is a critical area of health outcomes research, and Geographical Informational Systems (GIS) is a tool increasingly used for research in this area. GIS software programs can describe the geographic distribution of oncology care. GIS can effectively evaluate the supply of treatment resources within a given area relative to cancer prevalence and, more importantly, monitor for potential geographic variations in cancer outcomes and highlight potential disparities in cancer care. Because of this, GIS is becoming increasingly relevant in policy-oriented research focused on optimizing limited oncology resources within large underserved areas. This review describes the development and technical capabilities of GIS, potential applications of GIS in cancer research, and the limitations of such work.
Development and Capabilities of GIS Software
Developed in the 1960s by Dr. Roger Tomlinson of the Canadian Department of Forestry and Rural Development, the first GIS was originally constructed for surveying and development in rural parts of Canada. The original program, known as "Canada Geographical Information System" (CGIS), eventually grew to encompass datasets that spanned the entire country and became a useful tool in resource planning and management.[2] By the 1970s, universities and government organizations around the world had developed alternative GIS programs, and GIS-based research emerged as an independent multidisciplinary field. In 1982, as personal computer use began to increase, the Environmental Systems Research Institute (ESRI) developed the first commercially available GIS package, known as ARC/INFO.[3] The advent of commercially available GIS packages drastically increased the use of GIS worldwide. Users began to create open-use, publicly editable map data. The influx of map data into the public domain has only increased in recent years with the advent of new GIS technology and has allowed GIS to permeate many research fields.[4]
The functional capabilities of GIS software are a combination of modern cartography and database management. GIS programs are traditionally comprised of at least three functional components. First, GIS software permits users to input data that corresponds to a geographic location. Second, GIS software enables users to create maps to visually display integrated georegistered data. Third, GIS has database capability that allows users to store and manipulate entered data and maps.
Although found commercially in a variety of different software packages, our discussion of the technical aspects of GIS software will be limited to ESRI's ArcGIS. ArcGIS is the GIS software most widely used in health services research; it is used by more than 300,000 organizations worldwide, including most federal agencies, all 50 United States health departments, and over 24,000 state and local governments.[5] Data is stored in ArcGIS using shapefile packages. Shapefile packages are storage formats that house geographic location and associated attribute data. For example, a standard shapefile package could contain cancer incidence data, organized by county within the United States.
Regardless of GIS software type, the functional capabilities of GIS software can be effectively used in many areas of health services research. In addition to the ability to store and display regional data, several other functionalities of GIS software are worth noting. GIS software allows users to create their own maps and geographic units that can be tailored to more accurately describe healthcare patterns. Examples of this method in practice are maps developed by the Dartmouth Institute of Health Policy and Clinical Practice describing Hospital Referral Regions and Hospital Service Areas.[6] GIS software also allows users to freely aggregate data between different geographic units of analysis. For example, users can combine the individual cancer incidences within counties to estimate the cancer incidence of an entire state.
Finally, GIS software allows for the quantitative analysis of geographic patterns through "spatial analysis." Prior to the advent of GIS software, mapping in medical research was mainly a qualitative examination of data. In "spatial analysis," GIS software allows users to find statistically significant geographic relationships. GIS can employ spatial autocorrelation to find statistically significant geographic clustering of a variable. For example, a user could employ spatial autocorrelation to test whether there is statistically significant clustering of cancer incidences among neighboring counties. [7] Additionally, GIS can calculate geographically weighted regressions (GWR) to evaluate spatial heterogeneity among independent and dependent variables. Finally, GIS can employ spatial interpolation to estimate the geographic distribution of a variable within a region given the geographic distribution of the variable in surrounding regions.
Potential Applications of GIS in Cancer Research
GIS software allows for a rigorous assessment of the unique role geography plays in clinical oncology. Many types of studies are possible using GIS, and our description and examples of the potential applications of GIS to cancer research are not meant to be exhaustive. However, four broad categories of study come to mind. The first type of study is also perhaps the simplest: a graphical representation of cancer incidence and mortality. The second type of study is one that centers on the distribution of oncology resources. The third type of study is an investigation of geographic practice patterns. The fourth type of study is one that takes these geographic variations in oncology resources and practice patterns and relates them to socioeconomic disparity in cancer outcomes.
GIS for the surveillance of cancer incidence and mortality
TABLE 1
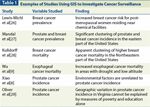
Examples of Studies Using GIS to Investigate Cancer Surveillance
Examples of this type of study are listed in Table 1. In one of these studies, Mandal et al utilized GIS and GWR to find a statistically significant increase in the clustering of breast and prostate cancer incidences in the eastern half of the United States. GIS software has also been used to explore the relationship between geographic environmental factors and cancer incidence and mortality rates.[8,9] Moreover, because GIS software can manipulate stored data, users can potentially calculate the changes in cancer incidence and mortality rates, in an effort to better understand geographic trends in the distribution of cancer. The ability of GIS software to display manipulated data allows users to create "heat maps" that visually display regions where cancer mortality is changing the most rapidly.
GIS for the study of oncology resources
TABLE 2
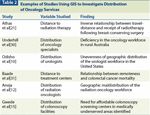
Examples of Studies Using GIS to Investigate Distribution of Oncology Services
Studies in this category are listed in Table 2. GIS software allows for the graphical representation of the distribution of oncology services and technology, and helps identify potential geographic disparities in cancer care. Moreover, GIS can help relate geographic resource disparities to cancer outcomes. Examples of GIS-aided investigation of oncology resources include the recent studies published by Odisho et al. In their initial work, published in 2009, the authors found geographic variation in the distribution of urologists across counties in the United States.[10] In a subsequent study, the same authors discovered that the uneven distribution of urologists is associated with variations in urologic cancer mortalities. Specifically, they found that the addition of one urologist to a county is associated with a significant reduction in urologic cancer mortalities.[11] Similar studies have used GIS to show an analogous maldistribution of radiation therapy services associated with increased mortality for prostate and gastrointestinal malignancies in the United States.[12-14]
In addition to relating disparity to outcomes, GIS can inform public health and health policy efforts by highlighting geographic areas where oncology resources are lacking. By isolating geographic disparities related to cancer treatment, GIS software provides clinicians with important information concerning potential areas in which to establish new practices or satellite clinics. In a study published by Gwede et al, a research team working in conjunction with community leaders in Florida, GIS software was used to identify potential areas in need of colorectal cancer screening services.[15] Additionally, GIS software can isolate regions with high incidences of cancer that need more vigilant clinical focus, distinguishing such regions from others with lower incidences of cancer, in which resources might currently be misallocated. The Dartmouth Institute of Health Policy and Practice has successfully employed GIS to evaluate geographic variation in Medicare spending as it relates to oncology.[16,17] The Institute continues to use GIS to evaluate ways to make our healthcare system as efficient as possible in providing cancer treatment given limited resources. GIS software is increasingly relevant in clinically oriented policy planning focused on improving cancer outcomes.
GIS for the study of variations in clinical practice patterns in oncology
TABLE 3

Examples of Studies Using GIS to Investigate Oncology Practice Patterns
Studies of this type are listed in Table 3. GIS has typically been used to evaluate cancer-screening patterns across geographic regions; for example, GIS software has been utilized to investigate potential determinants of varying mammography and colonoscopy rates across the country.[18-20] Another potential avenue GIS software could explore is the relationship between geography and oncology treatment. An interesting study by Anthas et al highlights the ability of GIS to illustrate potential variations in treatment that are associated with geography. The authors found an inverse relationship between travel distance to a radiation therapy center and receipt of radiation therapy following breast-conserving surgery.[21] Along with the varying opinions concerning which treatment modality is the most appropriate for a given oncologic situation, it is important to evaluate the extent to which geography plays a role in clinical decision making.
GIS to relate geographic disparities in oncology to other causes of inequality
TABLE 4

Examples of Studies Using GIS to Investigate Other Known Cancer Disparities
Finally, GIS software allows for the investigation of geographic disparities in the context of other known disparities that may influence cancer outcomes, such as race and socioeconomic status (Table 4). Specifically, one could investigate whether geographic variations in cancer-related outcomes are associated with demographic variables like race and socioeconomic status. For example, GIS software permits researchers to evaluate whether disparities in cancer outcomes remain when looking specifically at more racially and socioeconomically homogenous regions. This is particularly important, since geographic disparity has emerged as a factor that can mask or be a surrogate for racial and socioeconomic disparities.[22,23] Therefore, careful and in-depth study of geographic disparity is critical to unearthing the root causes of healthcare disparities.
Limitations
Several limitations of GIS must be acknowledged. Many of the limitations of GIS software revolve around inferences drawn from GIS-related research and concerns about the quality of GIS data. First, analyses that employ GIS software merely highlight associative relationships. Any hypothesis regarding a potential causal relationship established on the basis of a GIS-aided study would be premature. Like other research tools, results from GIS-aided analysis provide impetus for further inquiry to identify a potential causal relationship between associated variables. Second, although GIS software can aggregate data from different geographic units, such functionalities inherently allow for ecological fallacies. Findings concerning larger geographic units should not be extrapolated to derive inferences concerning individuals residing in that area. Third, because of the increased migration in the modern world, a patient's healthcare is no longer isolated to a definable geographic location. For this reason, conclusions drawn using GIS software must be approached cautiously. Fourth, resource limitations are a constant problem in all GIS-related research. Researchers are often restricted by the data that are available to them. GIS software requires georegistered data that are not easily available given the cost and professional training required for accurate data collection.[24] Moreover, data that are available for public use are often based on geographic units that are unrelated to healthcare and arbitrarily established for legislative purposes. However, with the ability to create unique shapefiles that correspond to more health-related geographic units, data limitations have been somewhat attenuated. Finally, georegistered data must be accurate and complete. Although data accuracy is a limitation in any research project, it remains an important issue in GIS-related research because resource-deprived geographic areas tend to potentiate data inaccuracies.[25]
Conclusion
GIS software is a powerful and increasingly utilized resource for evaluating both the clinical and policy problems related to oncology. Because it allows users to store, manipulate and display geographic health data, GIS software has many potential research applications in the field of oncology. GIS software can help in isolating potential geographic disparities in cancer care. Specifically, GIS allows investigation of these geographic disparities as they relate to oncology services, cancer incidence and mortality, practice patterns, and other known cancer disparities. However, as with any emerging technology, GIS-related research has several limitations. Potential ecological fallacies and issues concerning data accuracy are difficult to negotiate when studying any observational database, and these must be carefully monitored when using GIS software. Nevertheless, the relevance of GIS in clinical cancer research and policy discussions cannot be ignored, and it remains a potentially prolific resource for the future.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
REFERENCES
1. Clarke KC, McLafferty SL Tempalski BJ. On epidemiology and geographic information systems: a review and discussion of future directions. Emerg Infect Dis. 1996;2:85-92.
2. Fisch S. A history of GIS. Design Manage. 1992;16.
3. Grelot J-P. Cartography in the GIS age. Cartograph J. 1994;31:56-60.
4. Foresman TW, editor. The history of GIS (geographic information systems): perspectives from the pioneers. Prentice Hall; 1997.
5. ERSI: The language of geography: health and human services. Available from: http://www.esri.com/library/brochures/pdfs/health-brochure.pdf. Accessed January 25, 2011.
6. Dartmouth atlas of healthcare. Available from: http://www.dartmouthatlas.org/tools/downloads.aspx. Accessed January 25, 2011.
7. Fotheringham AS, Rogerson PA. GIS and spatial analytical problems. Intl J Geogr Inf Systems. 1993;7:3-19.
8. Xiao H, Gwede CK, Kiros G, Milla K. Analysis of prostate cancer incidence using geographic information system and multilevel modeling. J Natl Med Assoc. 2007;99:218-25.
9. Wu KS, Huo X, Zhu GH. Relationships between esophageal cancer and spatial environment factors by using Geographic Information System. Sci Total Environ. 2008;393:219-25.
10. Odisho AY, Fradet V, Cooperberg MR, et al. Geographic distribution of urologists throughout the United States using a county level approach. J Urol. 2009;181:760-5; discussion 65-6.
11. Odisho AY, Cooperberg MR, Fradet V, et al. Urologist density and county-level urologic cancer mortality. J Clin Oncol. 2010;28:2499-504.
12. Aneja S, Smith BD, Gross CP, et al. Geographic analysis of the radiation oncology workforce. Int J Radiat Oncol Biol Phys. 2011 Apr12. [Epub ahead of print]
13. Aneja S, Yu JB. Radiation oncologist density and prostate cancer mortality. J Clin Oncol. 2011;29(suppl 7):abstr 72.
14. Aneja S, Yu JB. Radiation oncologist density and colorectal cancer mortality. J Clin Oncol. 2011;29(suppl 4): abstr 605.
15. Gwede CK, Ward BG, Luque JS, et al. Application of geographic information systems and asset mapping to facilitate identification of colorectal cancer screening resources. Online J Public Health Inform. 2010;2:2893.
16. Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288-98.
17. Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273-87.
18. Mobley LR, Kuo TM, Urato M, Subramanian S. Community contextual predictors of endoscopic colorectal cancer screening in the USA: spatial multilevel regression analysis. Int J Health Geogr. 2010;9:44.
19. Mobley L, Kuo TM, Urato M, et al. Predictors of endoscopic colorectal cancer screening over time in 11 states. Cancer Causes Control. 2010;21:445-61.
20. Elkin EB, Ishill NM, Snow JG, et al. Geographic access and the use of screening mammography. Med Care. 2010;48:349-56.
21. Athas WF, Adams-Cameron M, Hunt WC, et al. Travel distance to radiation therapy and receipt of radiotherapy following breast-conserving surgery. J Natl Cancer Inst. 2000;92:269-71.
22. Chandra A, Skinner J. Geography and racial health disparities. National Bureau of Economic Research (NBER). NBER Working Paper Series. Vol w9513. Feb 2003. Available from http://ssrn.com/abstract=382444.
23. Chandra A. Who you are and where you live: race and the geography of healthcare. Med Care. 2009;47:135-7.
24. Tim US. The application of GIS in environmental health sciences: opportunities and limitations. Environ Res. 1995;71:75-88.
25. White E, Aldrich TE. Geographic studies of pediatric cancer near hazardous waste sites. Arch Environ Health. 1999;54:390-7.
26. Lewis-Michl EL, Melius JM, Kallenbach LR, et al. Breast cancer risk and residence near industry or traffic in Nassau and Suffolk Counties, Long Island, New York. Arch Environ Health. 1996;51:255-65.
27. Mandal R, St-Hilaire S, Kie JG, Derryberry D. Spatial trends of breast and prostate cancers in the United States between 2000 and 2005. Int J Health Geogr. 2009;8:53.
28. Kulldorff M, Feuer EJ, Miller BA, Freedman LS. Breast cancer clusters in the northeast United States: a geographic analysis. Am J Epidemiol. 1997;146:
161-70.
29. Oliver MN, Smith E, Siadaty M, et al. Spatial analysis of prostate cancer incidence and race in Virginia, 1990-1999. Am J Prev Med. 2006;30:S67-76.
30. Underhill C, Bartel R, Goldstein D, et al. Mapping oncology services in regional and rural Australia. Aust J Rural Health. 2009;17:321-9.
31. Baade PD, Turrell G, Aitken JF. A multilevel study of the determinants of area-level inequalities in colorectal cancer survival. BMC Cancer. 2010;10:24.
32. Engelman KK, Hawley DB, Gazaway R, et al. Impact of geographic barriers on the utilization of mammograms by older rural women. J Am Geriatr Soc. 2002;50:62-8.
33. Powell TM, Thompsen JP, Virgo KS, et al. Geographic variation in patient surveillance after radical prostatectomy. Ann Surg Oncol. 2000;7:339-45.
34. Vinnakota S, Lam NS. Socioeconomic inequality of cancer mortality in the United States: a spatial data mining approach. Int J Health Geogr. 2006;5:9.
35. Tian N, Gaines Wilson J, Benjamin Zhan F. Female breast cancer mortality clusters within racial groups in the United States. Health Place. 2010;16:209-18.
36. Eide MJ, Weinstock MA, Clark MA. The association of physician-specialty density and melanoma prognosis in the United States, 1988 to 1993. J Am Acad Dermatol. 2009;60:51-8.