Health Systems May Reduce Leukemia Survival Disparities in Low-Income Populations
Sustained improvements in leukemia outcomes in low- and middle-income countries are feasible with cross border programs, according to an expert from the University of California, San Diego.
Implementing health system models may help mitigate leukemia survival disparities in low- and middle-income countries, according to findings from a study that investigators will share at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting.
"Sustained improvements in cancer outcomes in low- and middle-income countries are feasible with innovative cross border programs, particularly in borders that are shared between a high-income country and a low-income country," according to an expert from the University of California, San Diego.
“Sustained improvements in cancer outcomes in low- and middle-income countries are feasible with innovative cross border programs, particularly in borders that are shared between a high-income country and a low-income country,” Paula Aristizabal, MD, MAS, associate professor of clinical pediatrics, Division of Pediatric Hematology/Oncology, University of California, San Diego (UCSD), said in a presentation of the data ahead of the meeting.
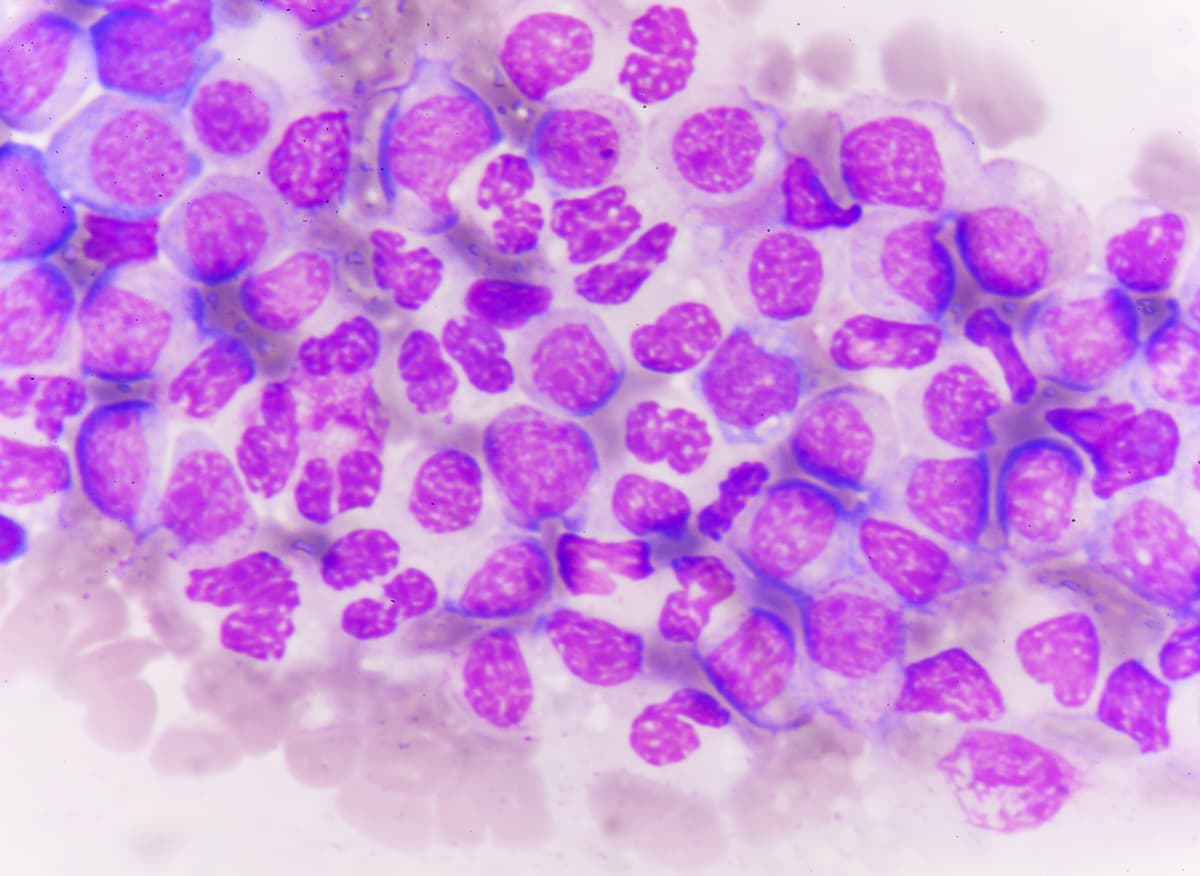
While the global burden of childhood cancer grows, survival rates remain stagnant in low- and middle-income countries, compared with high-income countries, “creating this huge survival gap,” Aristizabal said, adding that acute lymphoblastic leukemia is the most common pediatric cancer and is a leading cause of death among children in low- and middle-income countries.
As a result of significant health disparities that exist across the US border region, she noted that because their children's hospital is located only 23 miles from Tijuana, UCSD partners with the public sector in Baja California, Mexico, to improve outcomes in children with cancer across the border region.
Following this, UCSD partnered with St. Jude Children's Research Hospital to establish a “twinning approach” where a Center of Excellence in a high-income country collaborates and mentors a center in a low- and middle-income country, particular in this case, with a pediatric cancer center.
“The goal is to improve survival for children with cancer through sharing of knowledge, technology, and organizational skills; also consultation of clinical cases, education, and research and training; and other health systems strengthening models as our focus on capacity building and sustainability,” Aristizabal said, adding that for the program in Mexico, the main focus was on building capacity and sustainability for Hospital General-Tijuana.
Following this partnership, in 2013, the institutions implemented the WHO Framework for Action Health Systems Strengthening (HSS) comprised of 6 building blocks: health service delivery, health workforce, health information systems, access to essential medicines, financing, leadership, and governance.
“As the number of leukemia patients increase, we wanted to decrease that dependency on the international collaborators here in the US and ensure long-term sustainability,” Aristizabal said. “And the overall goal of implementing the WHO Framework for Action into the already existing training program was to improve survival for acute lymphoblastic leukemia, improve systems efficiency, provide timely access to care and ensure social and financial risk protection and sustainability over time.”
In the study, 109 children were treated at Hospital General-Tijuana. The median age was 7 years, and just over 50% were female. Further, 36 patients had standard risk disease and 73 had high-risk leukemia.
The pre-implementation phase was considered from 2008 to 2012, while the post-implementation phase was from 2013 to 2017.
The 5-year overall survival (OS) rate increased from 59% at pre-implementation to 65% during post-implementation, “and this was a significant improvement,” Aristizabal commented.
When stratified by risk, those who were at standard and high risk saw an improvement in OS from the pre-implementation and post-implementation phases (73% to 100% and 48% to 55%, respectively).
“This is really remarkable because the survival is the same as we have here in San Diego for high-risk patients,” Aristizabal said. “Still, this is an area of improvement and we're working on additional strategies to help improve this survival for high-risk patients.”
The investigators demonstrated that the Whole Framework for Action Model that was focused on sustainability in particular resulted in effectively reducing leukemia survival disparities in Tijuana. “Geographic proximity, mentor and data-driven projects to improve care led to better clinical outcomes, particularly survival, which was our main goal.” Aristizabal concluded. “And capacity building resulted in implementation of disease-specific treatment guidelines and a highly trained team able to provide high quality supportive care.”
Reference
Aristizabal P, Rivera Gomez R, Correa Ribeiro R, Roberts W. Childhood leukemia survival in the US-Mexico border: Building sustainable leukemia care using health systems strengthening models. J Clin Oncol. 2023;41:16. Abstract 1502