HIV+ Veterans Have Higher Rates of Unusual Cancers
CHICAGO-For many years, researchers have known that individuals who are seropositive for the human immunodeficiency virus (HIV) are at much greater risk of developing two forms of cancer-Kaposi’s sarcoma and non-Hodgkin’s lymphoma.
CHICAGOFor many years, researchers have known that individuals who are seropositive for the human immunodeficiency virus (HIV) are at much greater risk of developing two forms of cancerKaposi’s sarcoma and non-Hodgkin’s lymphoma.
A large-scale study of veterans for the first time shows that HIV-positive men also have a higher incidence of other unusual types of malignancies, compared with HIV-negative veterans or the male population as a whole, Adam J. Gordon, MD, reported at the Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC abstract 249).
The unusual malignancies with high rates in HIV-positive men involved the oral cavity and pharynx, digestive and respiratory systems, skin, and genitalia as well as cancers that are ill-defined, said Dr. Gordon, assistant professor of medicine, VA Pittsburgh Health System Center for Health Services Research.
The study authors did not compile enough evidence to determine why the rates of these cancers were higher in HIV-positive veterans. Dr. Gordon said it might be because men in the study have engaged in risky behaviors, such as excessive alcohol consumption or smoking. The magnitude of the increased risk also suggests that HIV infection or treatment may play a role.
Early Cancer Screening
"This type of information gives physicians an idea of what to look for in terms of other diseases that may be affecting the HIV population so they may institute some kinds of cancer screening early," he said.
The study included 868 HIV-positive men between the ages of 27 and 79 who were treated at HIV clinics in the Cleveland, Manhattan, and Houston VA hospitals between July 1999 and June 2000 as part of the Veterans HIV/AIDS Cohort Study (VACS 3).
Cancer incidence rates for these men were compared with malignancy rates for HIV-negative men between the ages of 25 and 84 who were treated at the same three VA hospitals during the same time period. Malignancy rates also were computed for men between the ages of 25 and 84 included in 1996-1997 Surveillance, Epidemiology, and End Results (SEER) data.
Overall, 12% of the men in VACS 3 had at least one type of cancer, excluding Kaposi’s sarcoma. When compared with HIV-negative veterans, VACS 3 men had a significantly higher incidence of cancer in three age groups: 25-34, 35-44, and 45-54. The difference in cancer incidence was significantly higher for VACS 3 men than for SEER men across all age groups.
Except for leukemia, which was often found in HIV-negative men, the HIV-positive men in VACS 3 had higher rates of cancer at all body sites than did HIV-negative veterans and SEER men.
Incidence rates were significantly higher in HIV-positive men than in the other two groups for five specific cancer types: oral, digestive, respiratory, skin, and genital.
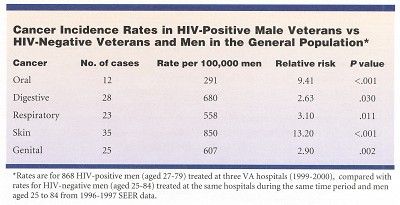
Of all cancer types, anal cancer had the highest rate ratio when HIV-positive veterans were compared with HIV-negative veterans and the general population. The authors suggested that since anal cancer has been associated with human papillomavirus (HPV), further study of HIV-positive veterans’ HPV status might reveal a relationship between HIV infection, its treatment, and the development of this form of cancer.
Ill-Defined Cancers
The rates of ill-defined and total cancers also were elevated in HIV-positive veterans. There were 24 cases of ill-defined cancer, for a rate of 583 per 100,000 and 185 total cancers, for a rate of 4,491 per 100,000. The relative risk of ill-defined malignancies in the HIV-positive group was 30.8 (P < .001), and for all cancers, it was 4.8 (P < .001).
VACS 3 is an ongoing cohort study that is following HIV-positive veterans on a longitudinal basis to monitor their health as they age, similar to the Framingham study. By providing a better understanding of the types of cancer that may be associated with HIV infection, VACS 3 is demonstrating that clinicians need to look beyond HIV.
"HIV is a serious disease, a serious infection, obviously. However, physicians who have HIV patients shouldn’t be conscious only of HIV; they should be diligent about surveillance for tumors," Dr. Gordon said.
Sarcoma Awareness Month 2023 with Brian Van Tine, MD, PhD
August 1st 2023Brian Van Tine, MD, PhD, speaks about several agents and combination regimens that are currently under investigation in the sarcoma space, and potential next steps in research including immunotherapies and vaccine-based treatments.