Immune Targeting in Breast Cancer
The immune system is active in breast cancer, playing a dual role in tumor progression and in immune surveillance. Infiltrating immune cells are both prognostic and predictive of response to standard breast cancer therapies.
Figure 1: The Inflammatory Tumor Microenvironment
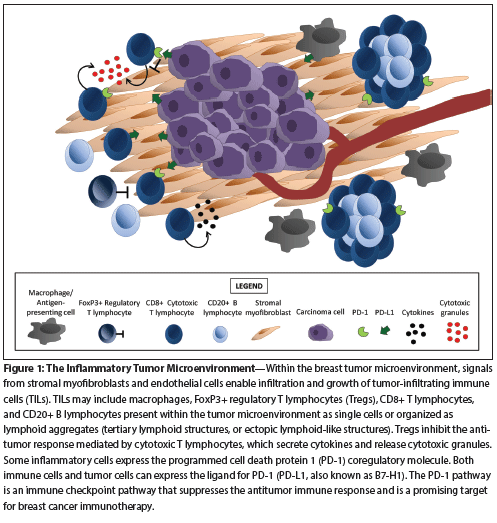
Figure 2: Receptor-Ligand Interactions That Regulate T-Cell Activation at the Immune Synapse
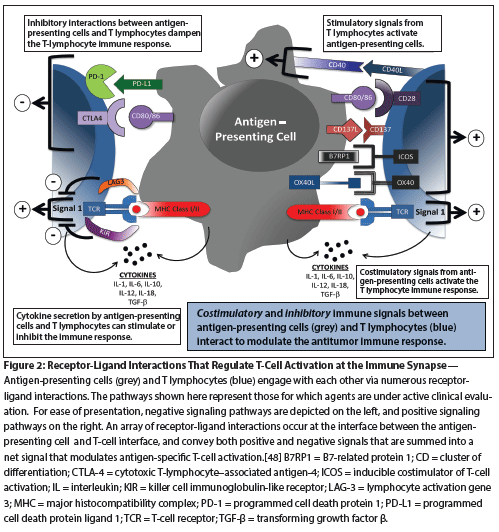
Table 1: Trials of Agents Targeting Immune Checkpoint Pathways in Breast Cancer
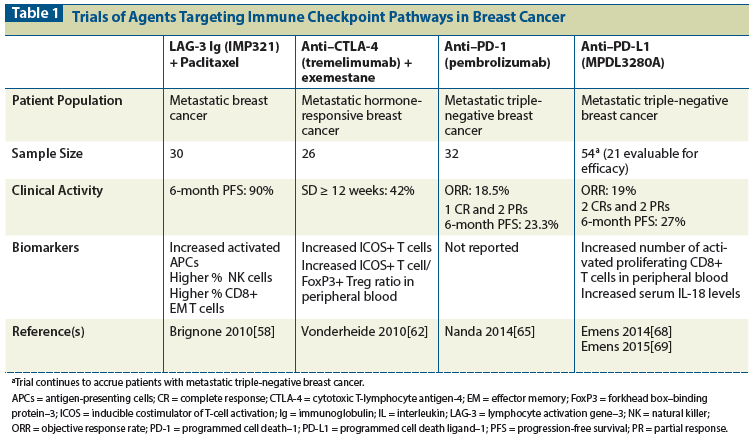
Table 2: Clinical Trials of Therapeutic Breast Cancer Vaccines
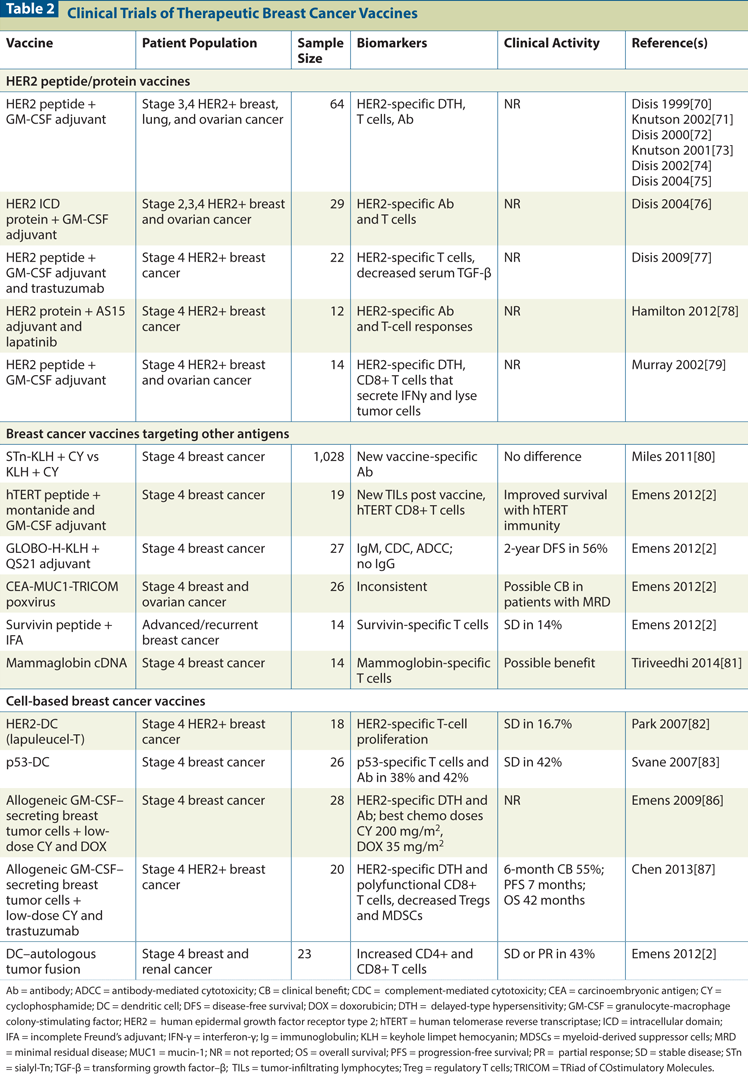
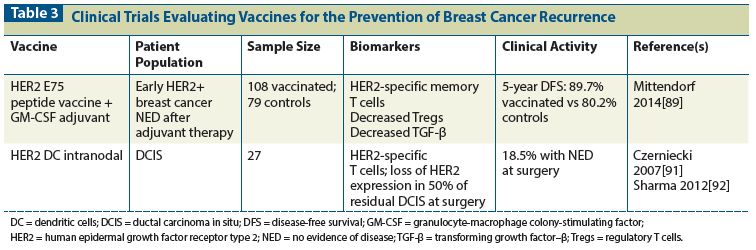
Table 3: Clinical Trials Evaluating Vaccines for the Prevention of Breast Cancer Recurrence
The immune system is active in breast cancer, playing a dual role in tumor progression and in immune surveillance. Infiltrating immune cells are both prognostic and predictive of response to standard breast cancer therapies. Breast cancer vaccines can activate and expand tumor-specific T cells, but have enjoyed minimal clinical success to date. Immune checkpoint blockade is a new approach to cancer immunotherapy, with documented clinical responses in diverse tumor types. Interest in breast cancer immunotherapy has been reignited by recent reports of objective responses in metastatic triple-negative breast cancer with both pembrolizumab (a programmed cell death protein 1 [PD-1] antagonist) and MPDL3280A (a programmed cell death ligand 1 [PD-L1] antagonist). Rational strategies for combination immunotherapy that expand and promote the trafficking of tumor-specific T cells, support their activity at the tumor site, and abrogate pathways of immune suppression within breast tumors are most likely to result in objective responses that translate into long-term disease control and cure.
Introduction
The immune system plays an integral and complex role in breast cancer biology, both promoting tumor growth and mediating the eradication of disease. Understanding this seemingly contradictory role requires insight into the dynamic interplay between various immune effector cells, tumor cells, stromal cells, and soluble factors; the theory of cancer immunoediting provides context for these considerations.[1] According to this hypothesis, tumor variants capable of surviving cancer immune surveillance are selected through genetic evolution, while those that cannot survive tumor surveillance are eradicated. The interaction between the immune system and tumors occurs in three phases: elimination, equilibrium, and escape. In the elimination phase, an acute inflammatory response triggered by stromal remodeling and angiogenesis initiates recruitment of innate immune cells (macrophages, dendritic cells, natural killer cells, and other cells) into the tumor microenvironment. Recognition of transformed tumor cells by these cells results in the production of proinflammatory cytokines, most notably interleukin-12 (IL-12) and interferon-γ (IFN-γ). These cytokines promote further activation of innate immune cells and tumor cell death. Also during this phase, dendritic cells mature, process tumor-associated antigens, and migrate into tumor-draining lymph nodes, where they present antigen to activate naive, tumor antigen–specific CD4+ and CD8+ T cells. These activated T cells expand and home to the tumor microenvironment, where they facilitate tumor cell death. The ultimate fate of the tumor can proceed in two directions: the complete eradication of tumor, or the evolution of tumor cell variants that escape the immune response and establish measurable tumors. Selective immune pressure on tumor cells can result in the accumulation of tumor cells with defects that predispose them to escape immune surveillance. These include loss of major histocompatibility complex (MHC) class I protein expression, other defects in antigen processing and presentation pathways, defects in T-cell receptor (TCR) signaling and costimulation, mutation or loss of tumor antigens, and deficiencies in IFN signaling pathways.[2-3] During the equilibrium phase, inflammation shifts from acute to chronic, ultimately leading to complete tumor escape from immune surveillance and to tumor outgrowth. Newly recruited tumor-associated cells (macrophages, regulatory T cells [Tregs], myeloid-derived suppressor cells, activated B lymphocytes, and tumor-associated fibroblasts) propagate chronic inflammation and tumor progression. Major mechanisms that actively promote tumor growth include the inhibition of tumor antigen–specific T cells by intratumoral regulatory T cells, a shift from an antitumorigenic T helper type 1 (TH1) immune response to a protumorigenic T helper type 2 (TH2) immune response, and the production of soluble factors by tumor cells that directly inhibit dendritic and T-cell function while promoting angiogenesis and stromal remodeling.[2,4,5] Furthermore, the upregulation of inhibitory immune checkpoint pathways-like the programmed cell death protein 1 (PD-1) pathway-by tumor cells and immune cells within the tumor microenvironment further inhibits the activation of tumor antigen–specific T cells.[5,6] Ultimately, tumors acquire complete autonomy from immune surveillance and grow and metastasize unchecked. This is the escape phase. Understanding the interplay of these cells and regulatory pathways in breast cancer will provide the blueprint for effective breast cancer immunotherapy, reversing the balance to promote tumor rejection by the immune system.
Immune Biomarkers in Breast Cancer
The impact of the immune milieu on breast cancer progression and outcomes depends upon both the carcinoma phenotype and inflammatory cell subsets within the breast tumor microenvironment (Figure 1).[2,7] For instance, it has long been recognized that medullary breast carcinomas carry a favorable prognosis, and are characterized by syncytial high-grade carcinoma cells with a prominent lymphoplasmacytic infiltrate.[8] Breast carcinomas can be further subdivided by gene expression profiles into intrinsic molecular subtypes[9-12] that have immunohistochemical surrogates based on tumor expression of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor 2 (HER2).[13,14] These subtypes include luminal A (ER+PR+HER2−Ki67low), luminal B (ER+PR+HER2−Ki67high or ER+PR+HER2+), HER2+ (ER−PR−HER2+), and basal-like (typically triple-negative [ER−PR−HER2−] disease with expression of cytokeratin 5/6 and/or epidermal growth factor receptor).
Triple-negative and HER2+ breast carcinomas are thought to be more immunogenic than luminal A carcinomas, as evidenced by the tumor-infiltrating lymphocyte (TIL) composition within the tumor microenvironment, as well as carcinoma gene signature patterns. Higher numbers of TILs are seen in ER– carcinomas compared with ER+ carcinomas.[14] Immune response gene expression modules are associated with better survival in ER−HER2− and HER2+ carcinomas, but not ER+HER2− carcinomas.[15] A T-cell metagene profile (lymphocyte-specific kinase metagene) correlated with improved response to chemotherapy in all ER− carcinomas and ER+HER2+ carcinomas.[16] B-cell gene profiles conferred a favorable prognosis in triple-negative breast carcinomas, ER− and ER+Ki67high carcinomas, but not ER+Ki67low carcinomas.[17-19] In contrast to luminal carcinomas, basal-like carcinomas had high expression of nonfavorable TH2/protumor humoral immunity genes.[20]
Tumor Infiltrating Lymphocytes and Lymphoid Aggregates in Breast Cancer
Association with survival
Both TILs and lymphoid aggregates have been associated with survival in breast cancer. The presence of TILs within the breast tumor microenvironment can be assessed by hematoxylin and eosin–stained sections, and immunohistochemistry (IHC) can be used to assess lymphocyte subsets and specifically characterize the TIL phenotype.[21] The presence of TILs in treatment-naive triple-negative breast carcinoma is an independent prognostic factor for improved overall survival,[22,23] decreased distant recurrence,[23,24] and increased metastasis-free survival.[25] In addition, the presence of TILs in residual triple-negative breast carcinoma after neoadjuvant chemotherapy is also prognostic for metastasis-free and overall survival.[26] The presence of brisk TILs in treatment-naive HER2+ carcinomas correlates with prolonged survival[22] and response to trastuzumab.[24] Among specific TIL subsets, high numbers of CD8+ cytotoxic T cells,[27] CD4+ follicular helper T cells,[28] and CD20+ B cells[29] are predictors for patient survival across breast carcinoma subtypes. Conversely, high numbers of forkhead box–binding protein–3 (FoxP3)+ Tregs are associated with higher tumor grade,[29,30] ER negativity,[30] shorter relapse-free survival,[29,31] and shorter overall survival time.[31] Consistent with these findings, metastatic triple-negative breast carcinomas at first relapse have fewer TILs than their matched primary breast carcinomas.[32] The clinical significance of tumor-infiltrating macrophages remains less clear.[33]
Lymphoid aggregates are another emerging biomarker for the inflamed tumor microenvironment. Also termed ectopic lymphoid-like structures[34] or tertiary lymphoid structures,[7,21,35] these aggregates can vary from loose clusters of T and B lymphocytes to well-organized nodules of lymphocytes with germinal centers.[34] These structures represent foci of immunoregulation that reflect an ongoing adaptive immune response.[36] Similar structures have been observed in treatment-naive breast carcinomas, where the density of high endothelial venules (thought to be a gateway for TIL entry into tumors) is associated with a low risk of relapse and longer overall survival time.[37]
Association with response to therapy
The presence of TILs and/or lymphoid aggregates in the breast tumor microenvironment can also predict response to neoadjuvant and adjuvant therapy. High numbers of TILs correlate with pathologic complete response (pCR) to neoadjuvant chemotherapy across breast carcinoma subtypes.[38-40] The presence of > 60% TILs or an immune subtype (based upon high mRNA expression of immune genes) correlates with pCR to neoadjuvant anthra-cyline-plus-taxane chemotherapy in triple-negative breast carcinomas and HER2+ carcinomas, particularly in patients treated with chemotherapy plus carboplatin.[41] High levels of TIL infiltrates in ER− carcinomas predict pCR after neoadjuvant anthracycline-based chemotherapy, but not after treatment with cyclophosphamide, methotrexate, and fluorouracil (CMF).[42] Greater numbers of TILs are also associated with decreased recurrence rates after treatment with adjuvant trastuzumab in HER2+ carcinomas.[24] In addition, a greater reduction in FoxP3+ Tregs is seen in patients responding to the aromatase inhibitor letrozole,[43] and the development of new TILs is associated with response to neoadjuvant paclitaxel.[44]
Furthermore, the presence of TILs in the residual breast tumor microenvironment after neoadjuvant therapy is a favorable prognostic factor. Decreased levels of FoxP3+ Tregs are seen in patients with pCR.[26,45] The presence of high CD8+ and low FoxP3+ T-lymphocyte levels in residual tumors after neoadjuvant chemotherapy is associated with improved recurrence-free and overall survival; notably, a score combining the CD8/FoxP3 ratio and pathologic stage identifies a subgroup with an overall survival of 100%.[46] The presence of T-bet+ lymphocytes within tertiary lymphoid nodules in residual HER2+ tumors after neoadjuvant therapy with trastuzumab and a taxane (therapies that promote a TH1 antitumor response) is also associated with improved recurrence-free survival.[47]
Biomarkers of the PD-1 Pathway in Breast Carcinomas
The PD-1 pathway is a major immune checkpoint pathway for immune responses within the tumor microenvironment.[48] PD-1 is a coregulatory molecule expressed by activated lymphocytes.[49] Its ligand, PD-L1 (also known as B7-H1), is expressed on infiltrating immune cells[50] but can also be induced on tumor cells by inflammatory cytokines.[6] PD-L1 may also be constitutively upregulated on tumor cells by autonomous cancer cell mutations. In breast cancer, PTEN loss leads to increased tumor PD-L1 expression and decreased T-cell proliferation,[51] and tumor PD-L1 expression is seen more often in carcinomas with TP53 mutations than other mutations, including mutations of PIK3CA.[52]
In breast cancer, the reported rates of PD-1 and/or PD-L1 expression by TILs or carcinoma cells vary between studies; this is likely due to differences in tumor sample size, sampling format (eg, tissue microarray vs whole section), and the method used to detect PD-1/PD-L1 expression. Overall, the presence of PD-1+ TILs is associated with an aggressive phenotype, including high tumor grade and lack of ER expression.[30] PD-1+ TILs are associated with worse survival in luminal B and basal-like carcinomas.[53] PD-L1 expression was first reported in 34% of primary breast carcinomas and 41% of TILs[54]; tumor PD-L1 expression correlated with high tumor grade and lack of ER expression. The reported rate of PD-L1 expression by tumor cells in triple-negative breast carcinoma ranges from 19%[51] to 59%,[52] and both PD-1+ TILs and PD-L1+ carcinoma cells are seen more often in triple-negative breast carcinoma than in other breast cancer subtypes.[52] PD-L1 expression in triple-negative breast carcinoma correlates with CD8+ TIL infiltrates.[51] PD-L1 expression was demonstrated by quantitative immunofluorescence in 30% of primary breast carcinomas, where PD-L1 expression also correlated with lack of ER expression, higher TIL counts, and the triple-negative breast carcinoma phenotype.[55] In addition, both PD-L1 expression by tumor cells and higher levels of TIL infiltrates predicted pCR to neoadjuvant chemotherapy on univariate and multivariate analysis. In situ mRNA hybridization detected PD-L1 mRNA in 55% to 60% of primary breast carcinomas in tissue microarrays,[56] and PD-L1 expression correlated with higher TIL infiltration and improved clinical outcomes. Another study reported poor clinical outcome in PD-L1+ breast carcinomas.[57]
Targeting the Immune System for Breast Cancer Therapy
The ability of TILs and lymphoid aggregates to predict survival and response to standard breast cancer therapies, combined with the recent clinical success of inhibiting the cytotoxic T lymphocyte antigen-4 (CTLA-4) and PD-1 immune checkpoint pathways in other cancers, has stimulated intense interest in directly targeting the immune system for breast cancer therapy. The major immunotherapeutic modalities for which clinical data are available are vaccines and immune checkpoint antagonists. A critical concept underlying immunotherapy is that, while vaccines target tumor antigens and immune checkpoint antagonists target molecules expressed by tumor cells or other cells within the tumor microenvironment, the ultimate end-effector and therapeutic target of cancer immunotherapy is the tumor-specific T cell.
Immune checkpoint agonists and antagonists
Regulation of T-cell activation. T cells are activated by the recognition of tumor antigens bound to MHC molecules, with the strength and quality of the T-cell activation signal fine-tuned by multiple receptor-ligand interactions (Figure 2).[48] These regulatory pathways can transmit positive signals that augment T-cell activation, or negative signals that blunt T-cell activation. Immune checkpoint receptors and ligands may be expressed by a variety of cells within the tumor microenvironment, including effector T cells, Tregs, macrophages, fibroblasts, and tumor cells themselves. Immune checkpoint agonists include molecules that target OX-40 and CD137 and promote tumor-specific T-cell activity by enhancing activation or maturation. Immune checkpoint antagonists include agents like ipilimumab, pembrolizumab, and nivolumab. These target CTLA-4 or PD-1 and block signaling through negative regulatory pathways that dampen T-cell activation, thereby enhancing T-cell activity by relieving suppression. Clinical work in breast cancer to date has focused on abrogating suppression by targeting the lymphocyte activation gene–3 (LAG-3), CTLA-4, or PD-1 pathways (Table 1).
Targeting the LAG-3 pathway. The recombinant soluble LAG-3 immunoglobulin (Ig) fusion protein, IMP321, was tested as part of first-line therapy in 30 patients with metastatic breast cancer.[58] IMP321 binds with high avidity to MHC class II, resulting in activation of antigen-presenting cells (APCs) and subsequent activation of memory T cells. IMP321 was given subcutaneously every 2 weeks the day after days 1 and 15 of weekly paclitaxel at 80 mg/m2 for 6 cycles. No clinically significant IMP321-related adverse events were noted, and the 6-month progression-free survival (PFS) rate was 90%. Biomarker analyses revealed a sustained increase in activated APCs and a greater percentage of natural killer and CD8+ effector memory T cells.
Blockade of the CTLA-4 pathway. Signaling through the CTLA-4 pathway occurs when the cell surface receptor CTLA-4 binds its ligands CD80 and CD86.[48] CTLA-4 is upregulated after T-cell activation, providing a mechanism for down-modulating the evolving T-cell response. Two monoclonal antibodies (MAbs) that inhibit CTLA-4 are either approved or under investigation for clinical use: The United States Food and Drug Administration (FDA) approved the MAb ipilimumab for both untreated and treatment-refractory metastatic melanoma, based on an overall survival benefit[59,60]; the second Mab, tremelimumab, is not FDA-approved but has been tested in a variety of cancers.[61] These agents have unique toxicity profiles compared with standard cancer therapies, with clinically significant autoimmune breakthrough events, including colitis, hypophysitis, hepatitis, and thyroiditis. The emergence of these breakthrough events occurs more frequently in patients who have an objective response to therapy.[48]
Tremelimumab was evaluated in 26 patients with metastatic hormone-responsive breast cancer.[62] The patients received tremelimumab at 3–10 mg/kg every 28 or 90 days, with concurrent exemestane at 25-mg daily. The majority of treatment-related adverse events were diarrhea (46%), pruritus (42%), constipation (23%), and fatigue (23%). Five patients had dose-limiting toxicities of diarrhea (4 patients) or transient elevation of transaminases (1 patient), and the maximum tolerated dose (MTD) was 6 mg/kg every 90 days. Of 13 patients treated at the MTD, no patient had grade 3/4 treatment-related diarrhea. The best overall response rate (ORR) was stable disease for 12 weeks or more in 11 of 26 patients (42%). Treatment was associated with increased levels of peripheral CD4+ and CD8+ T cells that expressed the protein inducible costimulator of T-cell activation (ICOS), a potential biomarker of immune activation resulting from blockade of CTLA-4. A marked increase in the ratio of ICOS+ T cells/FoxP3+ Tregs in the peripheral blood was observed.
Blockade of the PD-1 pathway. Signaling through the PD-1 pathway results when the cell surface receptor PD-1 binds to its ligands PD-L1/B7-H1 and PD-L2/B7-DC.[48] The PD-1 pathway inhibits immune responses within the tumor microenvironment. Blocking the PD-1/PD-L1 interaction alleviates immune suppression and unleashes the activity of tumor-specific T cells. Agents that antagonize the PD-1 pathway have demonstrated durable clinical activity in multiple types of advanced cancers,[63] and PD-1 blockade with nivolumab is associated with overall survival benefit in both advanced melanoma[64] and metastatic non–small-cell lung carcinoma (NSCLC). The FDA has approved two PD-1 antagonists, pembrolizumab and nivolumab, for the treatment of patients with advanced melanoma; nivolumab is also approved for metastatic NSCLC. PD-L1 expression by tumor cells or infiltrating immune cells within the tumor microenvironment is under intense investigation as a predictive biomarker of response to blockade of the PD-1 pathway. Early reports demonstrate that PD-1 pathway blockade has clinical activity in patients with metastatic triple-negative breast cancer.
Pembrolizumab was evaluated in 32 patients with advanced PD-L1+ triple-negative breast carcinoma.[65] Of all patients screened, 58% had PD-L1 staining in the tumor stroma or in
≥ 1% of tumor cells. Most patients treated with pembrolizumab had received one to three prior chemotherapy regimens for metastatic disease, and 21.9% had received five or more. Patients received pembrolizimab at a dose of 10 mg/kg intravenously (IV) every 2 weeks. Adverse events were generally manageable, with five grade 3/4 toxicities. There was also one treatment-related death due to disseminated intravascular coagulation. The ORR for 27 evaluable patients was 18.5%, including 1 CR and 2 partial responses (PRs). The median time to response was 18 weeks (range, 7–32 weeks), with the median duration of response not reached. The 6-month PFS rate was 23.3%.
The PD-L1 antagonist MPDL3280A is being evaluated in an ongoing phase Ia study exploring its safety and efficacy, as well as biomarkers of response in a variety of cancers, with demonstrated activity in NSCLC and urothelial bladder cancer.[66,67] One expansion cohort has enrolled patients with both PD-L1+ and PD-L1− triple-negative breast carcinoma.[68,69] Tumors were considered to be PD-L1+ if ≥ 5% of infiltrating immune cells stained for PD-L1 expression by immunohistochemistry. Among prescreened patients, 23% were PD-L1+ at first report. Enrolled patients were heavily treated, with 89% having received more than four lines of systemic therapy.[69] MPDL3280A was given at 15 or 20 mg/kg of a 1,200 mg flat dose IV every 3 weeks. MPDL3280A was well tolerated in 54 patients with PD-L1+ and PD-L1− disease who were evaluable for safety.[69] Low-grade adverse events, including fatigue, nausea, fever, anorexia, and asthenia, were observed in 63% of patients, while 11% of patients experienced grade 3 treatment-related adverse events. There was one case of grade 4 pneumonitis, and two deaths currently assessed as related by the investigator are under active investigation. The ORR for 21 PD-L1+ patients with metastatic triple-negative breast cancer evaluable for efficacy was 19%, including 2 CRs and 2 PRs; 3 of 4 of these responses were ongoing at the time of data cutoff. Three additional patients had clinical benefit in the setting of a nonclassical response, with durable regression of target lesions, even though new lesions developed. Pharmacodynamic changes associated with PD-L1 inhibition included transient increases in the number of activated, proliferating CD8+ T cells and increased levels of interleukin-18. Further evaluation of the safety and clinical activity of MPDL3280A in both PD-L1+ and PD-L1– metastatic triple-negative breast cancer is ongoing.
Breast Cancer Vaccines
The development of effective vaccines for both breast cancer therapy and prevention depends on targeting the most potent tumor-rejection antigens (HER2 is a prototype), overcoming systemic mechanisms of immune tolerance (Tregs, among others), and abrogating immune-suppressive pathways (eg, PD-1) within the tumor microenvironment.[2] Given this complexity of immunoregulation, combination immunotherapies will almost certainly have the greatest likelihood of success.
Vaccines are designed to stimulate immunity specific for breast tumor antigens, which may be delivered as a single immune target or combined into a multiantigen vaccine using a variety of vaccine platforms. Polyantigen vaccines may be comprised of antigen mixtures (peptide, protein, or carbohydrate), recombinant constructs that encode multiple antigens (plasmid DNA, viruses, bacteria), tumor cell extracts loaded onto dendritic cells, and tumor cell–based vaccines that are inherently polyantigenic. Clinical vaccine development has focused primarily on the tumor antigens HER2 and mucin-1 (MUC1), with additional trials evaluating human telomerase reverse transcriptase (hTERT), survivin, and mammaglobin. In addition, cell-based vaccines that deliver the entire antigenic profile of the breast tumor cell have been reported. Trials have tested vaccination alone, or in combination with standard breast cancer therapies to harness potential clinical synergies. Vaccine trials for therapy and secondary prevention are summarized in Table 2 and Table 3, respectively.
Therapeutic breast cancer vaccines
Antigen-specific vaccines. The Tumor Vaccine Group at the University of Washington has tested HER2 peptide and protein vaccines given with the adjuvant granulocyte-macrophage colony-stimulating factor (GM-CSF) in patients with metastatic HER2+ breast cancer.[70-76] HER2 peptide epitopes that only activate CD8+ T cells induce short-lived CD8+ T-cell responses.[71] In contrast, HER2 peptides that can activate both CD4+ and CD8+ T cells induce new delayed-type hypersensitivity (DTH-a marker of CD4+ T cell–dependent immunity) and durable CD8+ T-cell responses characterized by epitope spreading both within HER2 and to other breast tumor antigens not included in the vaccine.[72-75] Vaccination with HER2 intracellular domain protein and GM-CSF adjuvant was similarly immunologically active.[76] Clinical responses have not been reported on these trials. The Tumor Vaccine Group also tested HER2 peptide-based vaccination with standard trastuzumab therapy in 22 patients with metastatic HER2+ breast cancer.[77] HER2-specific immunity was boosted by vaccination, and epitope spreading occurred. Survival was inversely correlated with serum levels of transforming growth factor–β (TGF-β). Overall survival had not yet been reached at a median follow-up of 3 years. Others tested a HER2 protein vaccine with lapatinib in 12 patients with metastatic HER2+ breast cancer refractory to trastuzumab; antibody and T cells specific to HER2 were induced in 100% and 8% of patients, respectively.[78] The US Military Group also tested a HER2 peptide vaccine in metastatic breast cancer,[79] but has since focused efforts on evaluating vaccination for secondary prevention. Other HER2-specific vaccines have been less extensively tested.[2]
Breast cancer vaccines that target carbohydrate antigens and MUC1 have been tested extensively in patients with metastatic breast cancer.[2] MUC1 is an aberrantly glycosylated protein derived from secretory tissues, with antigens represented by peptide epitopes unmasked by altered glycosylation, and modified carbohydrate epitopes themselves. A vaccine consisting of MUC1 epitopes conjugated to the protein carrier keyhole limpet hemocyanin (KLH) induces the production of MUC1-specific antibodies, but no T cells. Vaccine activity was enhanced by a low dose of cyclophosphamide (CY) given 3 days prior to vaccination, as evidenced by higher antibody levels and longer median survival time in early trials. However, a phase III trial of sialyl-Tn conjugated to KLH+CY vs KLH+CY failed to confirm this activity.[80] Vaccines targeting other carbohydrate antigens, telomerase, survivin, p53, and mammaglobin have been less extensively tested.[2,81]
Cell-based vaccines. These vaccines directly or indirectly engage the power of dendritic cells to present tumor antigens and activate tumor immunity. Lapuleucel-T is comprised of autologous peripheral blood mononuclear cells (including APCs) loaded with a fusion protein containing HER2 linked to GM-CSF. In 18 patients with metastatic HER2+ breast cancer, vaccination activated T cells that proliferated and secreted IFN-γ; clinical responses included 1 PR lasting > 6 months and 3 patients with stable disease lasting > 12 months.[82] Dendritic cells loaded with p53 antigen have also been tested in 26 patients with metastatic breast cancer, with new p53-specific T-cell responses and stable disease noted in 38% and 42% of patients, respectively.[83]
We have evaluated an allogeneic breast tumor cell vaccine genetically modified to secrete GM-CSF.[84] The paracrine secretion of GM-CSF promotes the massive influx of dendritic cells at the vaccination site, resulting in the presentation of breast tumor antigens delivered by the vaccine to activate both CD4+ and CD8+ T cells.[85] Because this vaccine delivers HER2, responses to HER2 are followed as a sentinel marker of vaccine-induced immunity. We first tested this vaccine in a specifically timed sequence with a range of low doses of CY and doxorubicin (DOX) in 28 patients with stable metastatic breast cancer.[86] Vaccination induced CD4+ T-cell dependent immunity as measured by DTH and antibody levels[86]; HER2-specific T cells were also observed (Emens et al, unpublished data). The most immunologically active low doses of CY selectively induced the apoptosis of Tregs relative to effector T cells, thereby augmenting vaccine-activated immune responses.[87] We also tested this vaccine sequenced with low-dose CY and weekly trastuzumab in 20 patients with metastatic HER2+ breast cancer. Increased DTH developed in 35% of patients, and levels of polyfunctional HER2-specific CD8+ T cells expanded across the four vaccination cycles.[88]
Breast Cancer Vaccines for Immunoprevention
A unique and powerful feature of the immune system lies in its ability to prevent disease via the immunologic memory response. Applying vaccines to primary or secondary breast cancer prevention circumvents some of the barriers to successful cancer immunotherapy represented by established disease burdens and the immunosuppressive tumor microenvironment.
Secondary prevention
The US Military Institute Clinical Trials Group conducted two complementary clinical trials testing the HER2 peptide epitope E75 with adjuvant GM-CSF in disease-free, lymph node–positive (a dose-escalation study) or lymph node–negative (a dose-optimization study) breast cancer patients after standard adjuvant therapy.[2,89] Of 195 enrolled patients, 187 were assessable-108 in the vaccinated group and 79 in the control group. The investigators observed a dose-dependent immune response to vaccination. Five-year disease-free survival (DFS) was 89.7% in the vaccinated group and 80.2% in the control group (P = .08). Because of the trial design, 65% of patients received less than the optimal vaccine dose. Five-year DFS rates were 94.6% and 87.1% in optimally and suboptimally dosed patients, respectively. Boost vaccinations augmented immunity in patients who had lost response, and among 21 patients who were optimally boosted there was only one recurrence. This vaccine induced intra- and inter-antigen epitope spreading, decreased levels of Tregs and TGF-β in the peripheral blood, and increased levels of memory T cells.[2] Notably, breast cancer patients with HER2− tumors developed higher levels of immunity than patients with HER2+ tumors, possibly due to pre-existing antigen-specific immune tolerance.[90] The E75 peptide vaccine is currently being tested in a phase III trial (the PRESENT study) evaluating its ability to prevent disease relapse after standard therapy for patients with early-stage HER2− breast cancer. Additional small studies by this group have evaluated alternative HER2 peptide vaccines for secondary prevention.[2]
Dendritic cell–based vaccines targeting HER2 have also been evaluated in patients with ductal carcinoma in situ (DCIS).[91,92] Intranodal vaccination induced high numbers of
IFN-γ-secreting T cells specific for HER2. At surgery, 5 of 27 (18.5%) vaccinated patients had no evidence of disease. Vaccination was associated with eradication of HER2 expression in 11 of 22 (50%) patients with residual DCIS at surgery. These findings are consistent with immunoediting at the tumor site.
Primary prevention
Primary immunoprevention of breast cancer is highly attractive, and several features of breast cancer suggest it may be feasible. First, individuals at high risk for breast cancer can be identified. Second, breast cancer can already be prevented with endocrine agents like tamoxifen, raloxifene, and aromatase inhibitors. Third, the development of breast cancer occurs over a period of years, providing a window of time in which to intervene with an immunopreventive strategy. The success of vaccines against hepatitis B and the human papilloma virus provide proof of principle for the ability of antigen-specific immunity to prevent the development of cancer. The success of immunoprevention for breast cancer will require well-designed trials that target the best breast tumor antigens, include the most appropriate patient populations, integrate the best immunotherapies, and evaluate the most informative biomarkers. This is the future of breast cancer immunotherapy.
Conclusions
TILs are present in some, but not all, breast tumors. TILs are prognostic and predictive of response to standard therapies, so the immune system is clearly an active player in breast cancer biology. Understanding the pathways that control T cells within the breast tumor microenvironment will be critical to maximizing the clinical activity of breast cancer immunotherapy. Strategies to increase the number of patients whose tumors contain TILs will likely expand the pool of patients who can benefit from immunotherapy. Several breast cancer vaccines have been tested, with evidence of immune activation but only hints of clinical activity so far. There is now great excitement about the first reports of objective breast cancer responses to PD-1 pathway antagonists, which abrogate immune suppression to unleash the activity of T cells at the tumor site. Given the complexity of both breast cancer biology and the immune response to breast cancer, it is certain that rational combination immunotherapies designed to maximally support tumor-specific T cells will have the greatest success. The future is bright, as the most effective immunotherapies may not only effect objective tumor responses acutely, but also establish durable responses that promote the long-term control, and ultimately the cure, of breast cancer.
Financial Disclosure:Dr. Emens receives research funding from Aduro, Amplimmune, EMD Serono, Genentech, Maxcyte, Merck, and Roche; is a consultant to Aveo; and serves on the advisory board of Bristol-Myers Squibb. Dr. Cimino-Mathews receives funding/grant support from Roche-Genentech, and honoraria for serving on their advisory committee. Dr. Foote has no disclosures.
Acknowledgments and conflict of interest:This work was supported in part by Roche, Inc. (ACM, LAE), the Breast Cancer Research Foundation (LAE), and the Commonwealth Foundation (LAE). Under a licensing agreement between Aduro, Inc., and Johns Hopkins University, the University and Dr. Emens are entitled to milestone payments and royalty on sales of the GM-CSF–secreting breast cancer vaccine. The terms of these arrangements are being managed by Johns Hopkins University in accordance with its conflict of interest policies.
References:
1. Dunn GP, Bruce AT, Ikeda H, et al. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol. 2002;3:991-8.
2. Emens LA. Breast cancer immunobiology driving immunotherapy: vaccines and immune checkpoint blockade. Expert Rev Anticancer Ther. 2012;12:1597-1611.
3. Singh R, Paterson Y. Immunoediting sculpts tumor epitopes during immunotherapy. Cancer Res. 2007;67:1887-92.
4. Denardo DG, Coussens LM. Inflammation and breast cancer. Balancing immune response: cross-talk between adaptive and innate immune cells during breast cancer progression. Breast Cancer Res. 2007;9:212.
5. Coussens LM, Pollard JW. Leukocytes in mammary development and cancer. Cold Spring Harb Perspect Biol. 2011;3(pii):a003285.
6. Taube JM, Anders RA, Young GD, et al. Colocalization of inflammatory response with B7-H1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci Transl Med. 2012;127ra37.
7. Fridman WH, Pages F, Sautes-Fridman, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nature Rev Cancer. 2012;12:298-306.
8. Ridolfi RL, Rosen PP, Port A, et al. Medullary carcinoma of the breast: a clinicopathologic study with 10 year follow up. Cancer. 1977;40:1365-85.
9. Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumors. Nature. 2000;406:747-52.
10. Sorlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98:10869-74.
11. Sorlie T, Tibshirani R, Parker J, et al. Repeated observation of breast tumor subtypes in gene expression data sets. Proc Natl Acad Sci USA. 2003;100:8418-23.
12. Nielsen TO, Hsu FD, Jensen K, et al. Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res. 2004;10:5367-74.
13. O’Brien KM, Cole SR, Tse CK, et al. Intrinsic breast cancer subtypes, race, and long-term survival in the Carolina Breast Cancer Study. Clin Cancer Res. 2010;16:6100-10.
14. Schalper KA, Velcheti V, Carvajal D, et al. In situ PD-L1 mRNA expression is associated with increased TILs and better outcome in breast carcinomas. Clin Cancer Res. 2014;20:2773-82.
15. Desmedt C, Haibe-Kains B, Wirapati P, et al. Biological processes associated with breast cancer clinical outcome depend on the molecular subtypes. Clin Cancer Res. 2008;15:5158-65.
16. Rody A, Holtrich U, Pusztai L, et al. T cell metagene predicts a favorable prognosis in estrogen receptor-negative and HER2-positive breast cancers. Breast Cancer Res. 2009;11:R15.
17. Rody A, Karn T, Liedtke C, et al. A clinically relevant gene signature in triple negative and basal-like breast cancer. Breast Cancer Res. 2011;13:R97.
18. Bianchini G, Qi Y, Alvarez RH, et al. Molecular anatomy of breast cancer stroma and its prognostic value in estrogen receptor-positive and -negative cancers. J Clin Oncol. 2010;28:316-23.
19. Iglesia MD, Vincent BG, Parker JS, et al. Prognostic B-cell signatures using mRNA-seq in patients with subtypes-specific breast and ovarian cancers. Clin Cancer Res. 2014;20:3818-29.
20. Kristensen VN, Vaske CJ, Ursini-Siegel J, et al. Integrated molecular profiles of invasive breast tumors and ductal carcinoma in situ (DCIS) reveal differential vascular and interleukin signaling. Proc Natl Acad Sci USA. 2012;109:2801-7.
21. Salgado R, Denkert C, Demaria S, et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an international TILs Working Group 2014. Ann Oncol. 2015;26:259-71.
22. Loi S, Sirtaine N, Piette F, et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol. 2013;31:860-7.
23. Adams S, Gray RJ, Demaria S, et al. Prognostic value of tumor-infiltrating lymphocytes in triple negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol. 2014;32:2959-67.
24. Loi S, Michiels S, Salgado R, et al. Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: the FinHER trial. Ann Oncol. 2014;25:1544-50.
25. Krieke B, van Kouwenhove M, Horlings H, et al. Gene expression profiling and histopathological characterization of triple negative/basal-like breast carcinomas. Breast Cancer Res. 2007;9:R65.
26. Dieci MV, Cristicello C, Goubar A, et al. Prognostic value of tumor-infiltrating lymphocytes on residual disease after primary chemotherapy for triple negative breast cancer: a retrospective multicenter study. Ann Oncol. 2014;25:611-8.
27. Mahmoud SM, Paish EC, Powe DG, et al. Tumor infiltrating CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin Oncol. 2011;29:1949-55.
28. Gu-Trantien C, Loi S, Garaud S, et al. CD4+ follicular helper T cell infiltration predicts breast cancer survival. J Clin Invest. 2013;123:273-92.
29. Mahmoud SM, Lee AH, Paish EC, et al. The prognostic significance of B lymphocytes in invasive carcinoma of the breast. Breast Cancer Res Treat. 2012;132:545-53.
30. Ghebeh H, Barhoush E, Tulbah A, et al. FoxP3+ Tregs and B7-H1/PD-1+ T lymphocytes co-infiltrate the tumor tissues of high risk breast cancer patients: implication for immunotherapy. BMC Cancer. 2008;8:57.
31. Bates GJ, Fox SB, Han C, et al. Quantification of regulatory T cells enables the identification of high-risk breast cancer patients and those at risk of late relapse. J Clin Oncol. 2006;24:5373-80.
32. Cimino-Mathews A, Hicks JL, Sharma R, et al. Metastatic breast cancers at first relapse have fewer tumor-infiltrating lymphocytes than their matched primary breast tumors: a pilot study. Human Immunol. 2013;44:2494-500.
33. Mahmoud SM, Lee AH, Paish EC, et al. Tumour-infiltrating macrophages and clinical outcome in breast cancer. J Clin Pathol. 2012;65:159-63.
34. Pitzalis C, Jones GW, Bombardieri M, Jones SA. Ectopic lymphoid-like structures in infection, cancer, and autoimmune disease. Nature Rev Immunol, 2014;14:447-62.
35. Gajewski TJ, Schreiber H, Fu YX. Innate and adaptive cells in the tumor microenvironment. Nature Immunol. 2013;14:1014-22.
36. Aloisi F, Pujol-Borrell R. Lymphoid neogenesis in chronic inflammatory diseases. Nat Rev Immunol. 2006;6:205-17.
37. Martinet L, Garrido I, Filleron T, et al. Human solid tumors contain high endothelial venules: association with T- and B-lymphocyte infiltration and favorable prognosis in breast cancer. Cancer Res. 2011;71:5678-87.
â©38. Denkert C, Loibl S, Noske A, et al. Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol. 2010;28:105-13.
39. Ono M, Tsuda H, Shimizu C, et al. Tumor-infiltrating lymphocytes are correlated with response to neoadjuvant chemotherapy in triple-negative breast cancer. Breast Cancer Res Treat. 2012;132:793-805.
40. Mao Y, Qu Q, Zhang Y, et al. The value of tumor-infiltrating lymphocytes (TILs) for predicting response to neoadjuvant chemotherapy in breast cancer: a systematic review and meta-analysis. PLoS One. 2014;9:e115103.
41. Denkert C, von Minckwitz G, Brase JC, et al. Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin Oncol. 2015;33:983-91.
42. West NR, Milne K, Truong PT, et al. Tumor-infiltrating lymphocytes predict response to anthracycline-based chemotherapy in estrogen receptor-negative breast cancer. Breast Cancer Res. 2011;13:R126.
43. Generali D, Bates G, Berruti A, et al. Immunomodulation of FoxP3+ regulatory T cells by the aromatase inhibitor letrozole in breast cancer patients. Clin Cancer Res. 2009;15:1046-51.
44. Demaria S, Volm MD, Shapiro RL, et al. Development of tumor infiltrating lymphocytes in breast cancer after neoadjuvant therapy. Clin Cancer Res. 2001;7:3025-30.
45. Ladoire S, Arnould L, Apetoh L, et al. Pathologic complete response to neoadjuvant chemotherapy of breast carcinoma is associated with the disappearance of tumor-infiltrating FoxP3+ regulatory T cells. Clin Cancer Res. 2008;14:2413-20.
46. Ladoire S, Mignot G, Dabakuyo S, et al. In situ immune response after neoadjuvant chemotherapy predicts survival. J Pathol. 2011;224:389-400.
47. Ladoire S, Arnould L, Mignot G, et al. T-bet expression in intratumoral lymphoid structures after neoadjuvant trastuzumab plus docetaxel for HER2-overexpressing breast carcinoma predicts survival. Br J Cancer. 2011;105:366-71.
48. Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nature Rev Cancer. 2012;12:252-64.
49. Agata Y, Kwasaki A, Nishimura H, et al. Expression of the PD-1 antigen on the surface of stimulated mouse T and B lymphocytes. Int Immunol. 1996;8:765-72.
50. Dong H, Zhu G, Tamada K, Chen L. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nature Med. 1999;5:365-9.
51. Mittendorf EA, Philips AV, Meric-Bernstam F, et al. PD-L1 expression in triple-negative breast cancer. Cancer Immunol Res. 2014;2:361-70.
52. Gatalica Z, Snyder C, Maney T, et al. Programmed cell death 1 (PD-1) and its ligand (PD-L1) in common cancers and their correlation with molecular cancer type. Cancer Epidemiol Biomarkers Prev. 2014;23:2965-70.
53. Muenst S, Soysal SD, Gao F, et al. The presence of programmed death-1 (PD-1)-positive tumor-infiltrating lymphocytes is associated with poor prognosis in human breast cancer. Breast Cancer Res Treat. 2013;139:667-76.
54. Ghebeh H, Mohammed S, Al-Omair A, et al. The B7-H1 (PD-L1) T lymphocyte inhibitory molecule is expressed in breast cancer patients with infiltrating ductal carcinoma: correlation with important high-risk prognostic factors. Neoplasia. 2006;8:190-8.
55. Wimberly H, Brown JR, Schalper K, et al. PD-L1 expression correlates with tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy in breast cancer. Cancer Immunol Res. 2015;3:326-32.
56. Schalper KA, Velcheti V, Carvajal D, et al. In situ PD-L1 mRNA expression is associated with increased TILs and better outcome in breast carcinomas. Clin Cancer Res. 2014;20:2773-82.
57. Muenst S, Schaerli AR, Gao F, et al. Expression of programmed death ligand 1 (PD-L1) is associated with poor prognosis in breast cancer. Breast Cancer Res Treat. 2014;146:15-24.
58. Brignone C, Gutierrez M, Mefti F, et al. First line chemoimmunotherapy in metastatic breast carcinoma: combinations of paclitaxel and IMG-321 (LAG-3Ig) enhances immune responses and antitumor activity. J Transl Med. 2010;8:71.
59. Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in metastatic melanoma. N Engl J Med. 2010;363:711-23.
60. Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517-26.
61. Tarhini AA. Tremelimumab: a review of development to date in solid tumors. Immunother. 2013;5:215-29.
62. Vonderheide RH, LoRusso PM, Khalil M, et al. Tremelimumab in combination with exemestane in patients with advanced breast cancer and treatment-associated modulation of inducible costimulator expression on patient T cells. Clin Cancer Res. 2010;16:3485-94.
63. Lipson EJ, Forde PM, Hammers H-J, et al. Antagonists of PD-1 and PD-L1 in cancer treatment. Semin Oncol. 2015; in press.
64. Robert C, Long GV, Brady B, et al. Nivolumab in previously treated melanoma without BRAF mutation. N Engl J Med. 2015;372:320-30.
65. Nanda R, Chow L, Dees E, et al. A phase Ib study of pembrolizumab (MK-3475) in patients with advanced triple-negative breast cancer. Presented at 2014 San Antonio Breast Cancer Symposium; Dec 9-13, 2014; San Antonio, TX. Abstr S1-09.
66. Herbst RS, Soria JC, Kowanetz M, et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515:563-7.
67. Powles T, Eder JP, Fine GD, et al. MPDL3280A (anti-PD-L1) treatment leads to clinical activity in metastatic bladder cancer. Nature. 2014;55:558-62.
68. Emens L, Braiteh F, Cassier P, et al. Inhibition of PD-L1 by MPDL3280A leads to clinical activity in patients with metastatic triple negative breast cancer. Presented at 2014 San Antonio Breast Cancer Symposium; 2014 Dec 9-13; San Antonio, TX. Poster PD1-6.
69. Emens L, Braiteh F, Cassier P, et al. Inhibition of PD-L1 by MPDL3280A leads to clinical activity in patients with metastatic triple negative breast cancer. Presented at 2015 Annual Meeting of the American Association of Cancer Research; 2015 Apr 18-22; Philadelphia, PA. Abstr 6317.
70. Disis ML, Grabstein KH, Sleath PR, Cheever MA. Generation of immunity to the HER-2/neu oncogenic protein in patients with breast and ovarian cancer using a peptide-based vaccine. Clin Cancer Res. 1999;5:1289-97
71. Knutson KL, Schiffman K, Cheever MA, Disis ML. Immunization of cancer patients with a HER2/neu, HLA-A2 peptide, p369-377, results in short-lived peptide-specific immunity. Clin Cancer Res. 2002;8:1014-18.
72. Disis ML, Schiffman K, Gooley TA, et al. Delayed type hypersensitivity is a predictor of peripheral blood T-cell immunity after HER-2/neu peptide immunization. Clin Cancer Res. 2000;6:1347-50.
73. Knutson KL, Schiffman K, Disis ML. Immunization with a HER-2/neu helper peptide vaccine generates HER-2/neu CD8 T cell immunity in cancer patients. J Clin Invest. 2001;107:477-84.
74. Disis ML, Gooley TA, Rinn K, et al. Generation of T-cell immunity to the HER-2/neu protein after active immunization with HER-2/neu peptide-based vaccines. J Clin Oncol. 2002;20:2624-32.
75. Disis ML, Goodell V, Schiffman K, Knutson KL. Humoral epitope-spreading following immunization with a HER-2/neu peptide-based vaccine in cancer patients. J Clin Immunol. 2004;24:571-8.
76. Disis ML, Schiffman K, Guthrie K, et al. Effect of dose on immune response in patients vaccinated with an HER-2/neu intracellular domain protein-based vaccine. J Clin Oncol. 2004;22:1916-25.
77. Disis ML, Wallace DR, Gooley TA, et al. Concurrent trastuzumab and HER-2/neu-specific vaccination in patients with metastatic breast cancer. J Clin Oncol. 2009;27:4685-92.
78. Hamilton E, Blackwell K, Hobeika AC, et al. Phase I clinical trial of HER-2-specific immunotherapy with concomitant HER-2 kinase inhibition. J Transl Med. 2012;10:28.
79. Murray JL, Gillogly ME, Przepiorka D, et al. Toxicity, immunogenicity, and induction of E75-specific tumor-lytic CTLs by HER-2 peptide E75 (369-377) combined with granulocyte-macrophage colony-stimulating factor in HLA-A2+ patients with metastatic breast and ovarian cancer. Clin Cancer Res. 2002;8:3407-18.
80. Miles D, Roché H, Martin M, et al. Theratope Study Group. Phase III multicenter clinical trial of the sialyl-TN (STn)-keyhole limpet hemocyanin (KLH) vaccine for metastatic breast cancer. Oncologist. 2011:16:1092-1100.
81. Tiriveedhi V, Tucker N, Herndon J, et al. Safety and preliminary evidence of biologic efficacy of a mammaglobin-a DNA vaccine in patients with stable metastatic breast cancer. Clin Cancer Res. 2014;20:5964-75.
82. Park JW, Melisko ME, Esserman LJ, et al. Treatment with autologous antigen-presenting cells activated with the HER-2-based antigen lapuleucel-T: results of a phase I study in immunology and clinical activity in HER-2-overexpressing breast cancer. J Clin Oncol. 2007;25:3680-7.
83. Svane IM, Pedersen AE, Johansen JS, et al. Vaccination with p53 peptide-pulsed dendritic cells is associated with disease stabilization in patients with p53 expressing advanced breast cancer: monitoring of serum YKL-40 and IL-6 as response biomarkers. Cancer Immunol Immunother. 2007;56:1485-99.
84. Davis-Sproul JM, Harris MP, Davidson NE, et al. Cost-effective manufacture of an allogeneic GM-CSF-secreting breast tumor vaccine in an academic cGMP facility. Cytotherapy. 2005;7:46-56.
85. Gupta R, Emens LA. GM-CSF-secreting vaccines for solid tumors: moving forward. Discov Med. 2010;10:52-60.
86. Emens LA, Asquith JM, Leatherman JM, et al. Timed sequential treatment with cyclophosphamide, doxorubicin, and an allogeneic granulocyte-macrophage colony-stimulating factor-secreting breast tumor vaccine: a chemotherapy dose-ranging factorial study of safety and immune activation. J Clin Oncol. 2009;27:5911-8.
87. Chen G, Leatherman JM, Sunay ME, Emens LA. Cyclophosphamide selectively induces dose-dependent apoptosis of CD4+FoxP3+ regulatory T cells relative to CD4+FoxP3- effector T cells in breast cancer patients. Cancer Res. 2013;73(8 suppl):abstr 4749. Available from: http://cancerres.aacrjournals.org/content/73/8_Supplement/4749.short. Accessed April 14, 2015.
88. Chen G, Gupta R, Petrik S, et al. A feasibility study of cyclophosphamide, trastuzumab, and an allogeneic GM-CSF-secreting tumor vaccine for HER-2+ metastatic breast cancer. Cancer Immunol Res. 2014;2:949-61.
89. Mittendorf EA, Clifton GT, Holmes JP, et al. Final report of the phase I/II clinical trial of the E75 (nelipepimut-S) vaccine with booster inoculations to prevent disease recurrence in high-risk breast cancer patients. Ann Oncol. 2014;25:1735-42.
90. Benavides LC, Gates JD, Carmichael MG, et al. The impact of HER-2/neu expression level on response to the E75 vaccine: from the US Military Institute Clinical Trials Study Group Study I-01 and I-02. Clin Cancer Res. 2009;15:2895-2904.
91. Czerniecki BJ, Koski GK, Koldovsky U, et al. Targeting HER-2/neu in early breast cancer development using dendritic cells with staged interleukin-12 burst secretion. Cancer Res. 2007;67:1842-52.
92. Sharma A, Koldovsky U, Xu S, et al. HER-2-pulsed dendritic cells can eliminate HER-2 expression and impact ductal carcinoma in situ. Cancer. 2012;118:4354-62.