Improved OS in Leukemia Elicited by cBTK and BCL2 inhibitors and anti-CD20 Antibodies
Data shown at ASH 2024 demonstrated higher OS rates with anti-CD20 antibodies in patients with chronic lymphocytic leukemia and small lymphocytic lymphoma.
Data shown at ASH 2024 demonstrated higher OS rates with anti-CD20 antibodies in patients with chronic lymphocytic leukemia and small lymphocytic lymphoma.
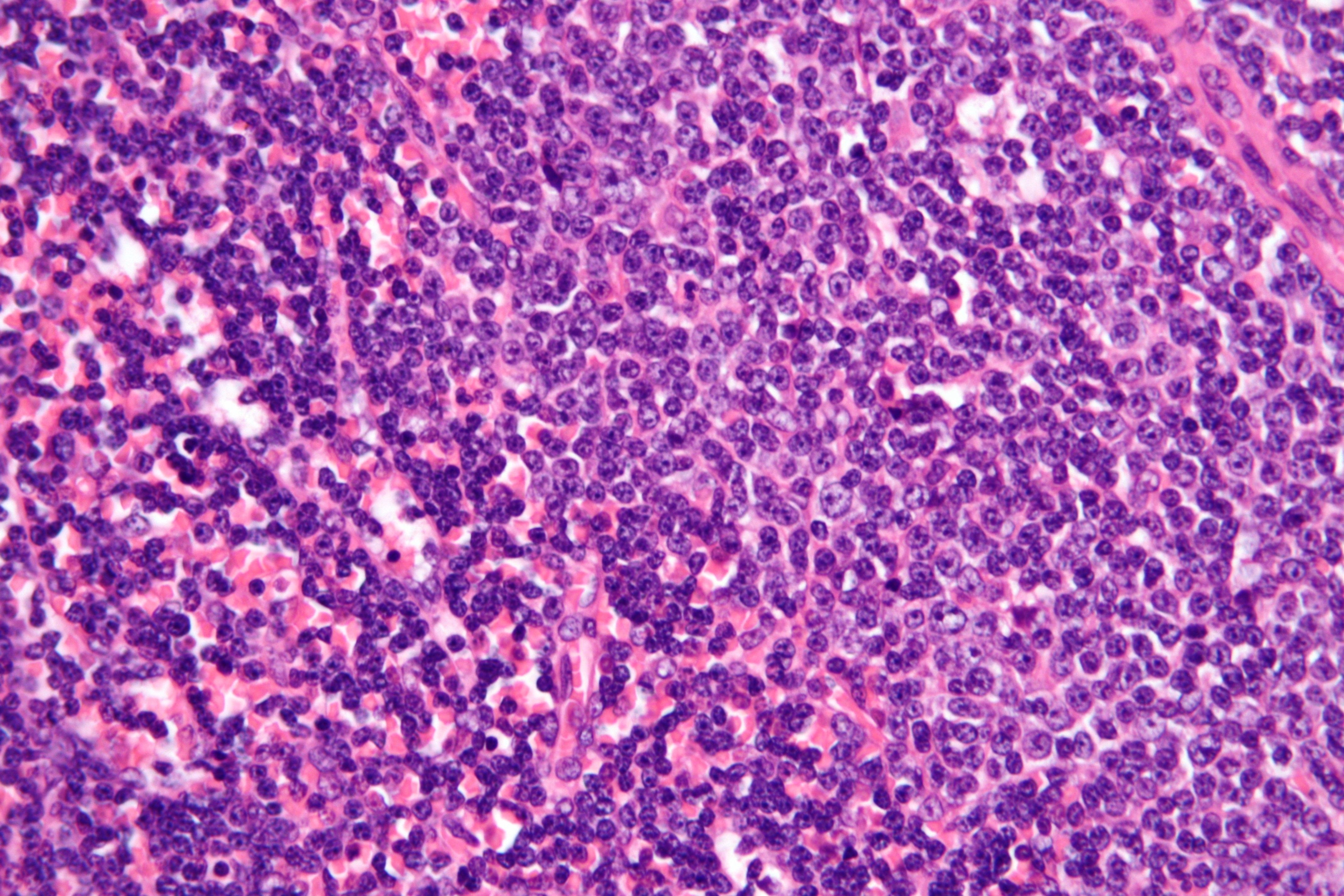
For patients with chronic lymphocytic leukemia (CLL) and small lymphocytic leukemia (SLL), covalent Bruton tyrosine kinase inhibitors (cBTKIs) followed by B-cell lymphoma-2 (BCL2) inhibitors and anti-CD20 monoclonal antibodies corresponded with improved overall survival (OS) whereas patients who received chemoimmunotherapy then cBTKI monotherapy or anti-CD20 antibodies corresponded with worse OS outcomes.
These findings were presented during a presentation at the 2024 American Society of Hematology Annual Meeting & Exposition (ASH), through analyzing the impact of real-world treatment sequences on OS in patients with CLL/SLL in the US.1
Background and Objectives of the Trial
Over the past decade, treatment strategies for CLL/SLL have evolved, with a shift from traditional chemoimmunotherapy to targeted therapies, including BTKis, BCL2 inhibitors, and anti-CD20 monoclonal antibodies. However, the sequencing of these therapies to optimize patient outcomes remains an area of debate, according to the poster presented at ASH. This is particularly true in the real-world setting, where multiple factors influence treatment decisions.
In this study, investigators utilized the Flatiron Health electronic health recordz–derived de-identified database to analyze treatment sequences in adult patients with CLL/SLL who started systemic therapy after 2016. The study compared OS associated with the most frequent treatment sequences across the first and second lines of therapy.
A total of 2354 patients met the eligibility criteria, which included having CLL/SLL, being 18 years or older at the index date, having received first-line treatment on or after January 1, 2016, and having received at least 2 lines of therapy. The study then focused on 1711 patients who received 1 of 16 of the most frequent treatment sequences, which included combinations of chemoimmunotherapy, anti-CD20 monoclonal antibodies, cBTKi, and BCL2i.
The median age of patients in this cohort was 71 years (interquartile range, 63-78), and most were male (63%) and non-Hispanic White (73.6%). For those with available data, 10.8% of patients had a del(17p)/TP53 mutation, 62.2% had unmutated IGHV, 91.4% had an ECOG performance status of 0 or 1, and 62.6% were initially diagnosed with RAI stage 0/I.
The study identified several treatment sequences that were commonly used in the real world, including chemoimmunotherapy followed by cBTKi monotherapy (20.5%), anti-CD20 monoclonal antibodies monotherapy followed by cBTKi monotherapy (11.7%), anti-CD20 monoclonal antibody monotherapy followed by BCL2i + anti-CD20 monoclonal antibodies (10.2%), and cBTKi monotherapy followed by anti-CD20 monoclonal antibody monotherapy (6.3%).
Findings and Clinical Implications
OS was analyzed by comparing various treatment sequences to the reference sequence of cBTKi monotherapy followed by BCL2i and anti-CD20 monoclonal antibodies, which was associated with the best OS outcomes.
Patients who received the following sequences had significantly worse OS: cBTKi monotherapy followed by anti-CD20 monoclonal antibody monotherapy (adjusted hazard ratio [aHR], 2.47), anti-CD20 monoclonal antibody monotherapy followed by chemoimmunotherapy (aHR, 2.68), and chemoimmunotherapy followed by chemoimmunotherapy (aHR, 2.87). Sequences that included cBTKi monotherapy followed by BCL2i and anti-CD20 monoclonal antibodies were not significantly different in OS when adjusted for baseline factors and treatment history.
OS outcomes were similar to the reference group with sequences that did not involve BCL2i in the second line of therapy. The median OS for those given cBTKi monotherapy followed by anti-CD20 monoclonal antibody monotherapy sequence was 63 months, while OS for most other sequences could not be estimated due to limited follow-up or patient drop-out.
“Optimizing treatment sequencing remains an important area of future research in this population,” study authors wrote in the poster.
Reference
Rhodes JM, Bhandari NR, Khanal M, et al. Overall survival associated with real-world treatment sequences in patients with CLL/SLL in the United States. Blood. 2024;144(suppl 1):5144. doi:10.1182/blood-2024-198104