Ivonescimab/Chemo Combo Yields Positive Efficacy and Safety Results in TNBC
Ivonescimab with chemotherapy elicited a median progression-free survival of 9.36 months in patients with locally advanced unresectable or metastatic triple-negative breast cancer.
Ivonescimab with chemotherapy elicited a median progression-free survival of 9.36 months in patients with locally advanced unresectable or metastatic triple-negative breast cancer.
Ivonescimab (SMT112) in tandem with chemotherapy demonstrated strong antitumor activity and a manageable safety profile in patients with locally advanced unresectable or metastatic triple-negative breast cancer (TNBC), according to results from an open-label, multicenter phase 2 Chinese study (NCT05227664) shared at the 2024 San Antonio Breast Cancer Symposium (SABCS).
At a median follow-up of 11.8 months (95% CI, 10.9-12.8), the overall response rate (ORR) in all evaluable patients (n = 35) was 80.0% (95% CI, 63.1%-91.1%). Complete responses (CR) were observed in 2 (5.7%) patients, partial responses in 26 (74.3%) patients, and stable disease in 7 (20.0%) patients. The disease control rate (DCR) was 100.0% (95% CI, 90.0%-100.0%). The median duration of response (DOR) was 7.49 months (95% CI, 5.32-not evaluable [NE]); the 6-month DOR rate was 72.2% (95% CI, 45.4%-87.4%).
The median progression-free survival (PFS) was 9.36 months (95% CI, 6.24-NE), the 6-month PFS rate was 73.8% (95% CI, 52.7%-86.6%), and the 9-month PFS rate was 61.3% (95% CI, 39.7%-77.1%).
“Ivonescimab in combination with chemotherapy had a manageable safety profile and promising antitumor activity in patients with locally advanced unresectable or metastatic TNBC,” lead study author Quchang Ouyang, MD, of Hunan Provincial Tumor Hospital in Changsha, China, and coinvestigators wrote in the presentation. “Results of this analysis support further evaluation of ivonescimab in combination with chemotherapy as a first-line treatment for TNBC.”
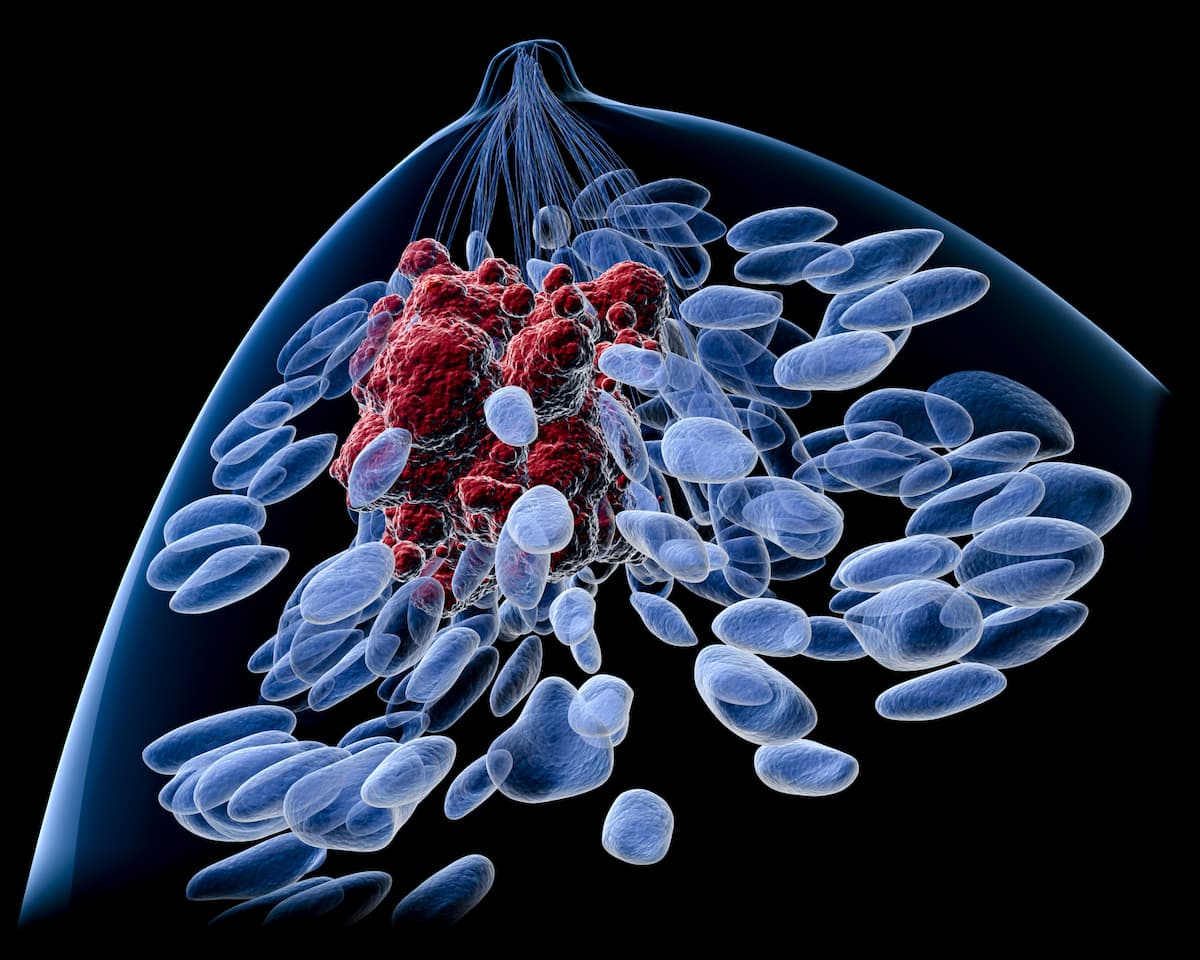
Ivonescimab is an investigational, tetrameric, bispecific antibody targeting PD-1 and VEGF.
To be eligible for enrollment on the phase 2 Chinese study, patients must have been between 18 and 75 years, had an ECOG performance status of 0 or 1, measurable disease per RECIST v1.1 criteria, not having received prior chemotherapy or targeted systemic therapy for TNBC, and at least 1 year from the time of last dose of previous neoadjuvant/adjuvant taxane treatment to disease recurrence.
Patients were administered 20 mg/kg of ivonescimab every 2 weeks with either 90 mg/m2 of paclitaxel or 100 mg/m2 of nab-paclitaxel (Abraxane), all on day 1, 8, and 15 of each 4-week treatment cycle.
The primary end points of the study were ORR and incidence and severity of AEs. Secondary end points were DCR, DOR, and PFS.
Of the 36 patients, the median age was 54.6 years (range, 35.4-73.3). A total 83.3% of patients had a PD-L1 CPS of less than 10 at baseline; 14 (38.9%) patients had an initial metastatic diagnosis, and 22 patients (61.1%) had recurrent or metastatic disease. Exactly half of all patients had an ECOG performance status of 0.
Also, 20 patients (55.6%) received prior taxane-based neoadjuvant or adjuvant therapy. Six patients (16.7%) had received prior endocrine therapy; 2 (5.6%) received a CDK4/6 inhibitor, and 1 (2.8%) received targeted therapy.
Additional efficacy data showed that, in patients with a PD-L1 combined positive score (CPS) greater than 10 (n = 6), the ORR was 83.3% (95% CI, 35.9%-99.6%), with 1 CR (16.7%). The DCR was 100.0% (54.1%-100.0%), and the median DOR was not reached (NR; 95% CI, 3.58-NE); the 6-month DOR rate was 80.0% (95% CI, 20.4%-96.9%). The median PFS was NR (95% CI, 5.36-NE), the 6-month PFS was 83.3% (95% CI, 27.3%-97.5%), and the 9-month PFS rate was 66.7% (95% CI, 19.5%-90.4%).
In patients with a PD-L1 CPS less than 10 (n = 29), the ORR was 79.3% (95% CI, 60.3%-92.0%), which comprised 1 CR (3.4%). The DCR was 100.0% (88.1%-100.0%) and the median DOR was 7.49 months (95% CI, 3.91-NE); the 6-month DOR rate was 70.0% (95% CI, 38.2%-87.6%). The median PFS was 9.30 months (95% CI, 5.55-NE), the 6-month PFS was 71.2% (95% CI, 46.6%-86.0%), and the 9-month PFS rate was 59.8% (95% CI, 35.0%-77.7%).
In patients with a PD-L1 CPS less than 1 (n = 17), the ORR was 88.2% (95% CI, 63.6%-98.5%), which consisted fully of partial responses. The DCR was 100.0% (80.5%-100.0%) and the median DOR was 7.49 months (95% CI, 3.45-NE); 6-month DOR rate was 64.2% (95% CI, 30.2%-84.8%). The median PFS was 9.30 months (95% CI, 5.26-NE), the 6-month PFS was 70.0% (95% CI, 38.2%-87.6%), and the 9-month PFS rate was 61.3% (95% CI, 30.0%-81.9%).
Regarding safety, all patients (n = 36) experienced a treatment-emergent adverse event (TRAE) of any grade; 18 (50.0%) patients experienced a TRAE of grade 3 or higher and 9 (25.0%) experienced serious TRAEs. No TRAEs led to discontinuation or death.
The most common TRAEs of any grade and grade 3 or higher were decreased white blood cell count (69.4% and 22.2%, respectively), decreased neutrophil count (55.6% and 19.4%), increased alanine aminotransferase (50.0% and 5.6%), and increased aspartate aminotransferase (50.0% and 5.6%).
Reference
Wang X, Ouyang Q, Tian C, et al. Evaluation of the safety and efficacy of ivonescimab in combination with chemotherapy as first-line treatment for triple-negative breast cancer. Presented at: 2024 San Antonio Breast Cancer Symposium; December 10-13, 2024; San Antonio, TX. Abstract PS3-05.