Ixabepilone Combo Improves PFS/OS in Platinum-Resistant Ovarian Cancer
Even when adjusting for prior taxane responses in patients with ovarian cancer, ixabepilone/bevacizumab appears to yield survival benefits in a phase 2 trial.
“The addition of ixabepilone to bevacizumab conferred benefit in PFS and OS, even when adjusting for prior taxane response,” according to the study authors.
Significant improvements in progression-free survival (PFS) and overall survival (OS) with ixabepilone (Ixempra) plus bevacizumab (Avastin) compared with ixabepilone monotherapy among those with platinum-resistant or platinum-refractory ovarian cancer, according to updated findings from a phase 2 trial (NCT03093155) presented at the Society of Gynecologic Oncology (SGO) 2024 Annual Meeting on Women’s Cancer.1
Data showed that patients treated with the combination (n = 39) achieved an overall response rate (ORR) of 38.4% vs 8.1% for patients treated with ixabepilone alone (n = 37; P = .003). No complete responses were achieved, but durable responses, defined as stable disease or a partial response sustained for at least 6 months, were observed in 14 patients in the combination arm.
Furthermore, the combination elicited a median PFS of 5.5 months vs 2.2 months for ixabepilone alone (HR, 0.31; 90% CI, 0.20-0.49; P < .001). The median OS was 10.3 months for the combination and 6.0 months for ixabepilone monotherapy (HR, 0.56; 90% CI, 0.38-0.84; P = .02).
“The addition of ixabepilone to bevacizumab conferred benefit in PFS and OS, even when adjusting for prior taxane response,” Dana M. Roque, MD, and colleagues, wrote in a poster presentation of the data. When adjusting for prior taxane response, PFS (HR, 0.31; 90% CI, 0.20-0.48; P < .001) and OS (HR, 0.59; 90% CI, 0.39-0.88; P < .03) benefits were also observed with the combination.
Roque is an associate professor of obstetrics, Gynecology and Reproductive Sciences, at the University of Maryland Medical System in Baltimore.
The trial was designed to evaluate whether the microtubule-stabilizing agent ixabepilone could retain activity in paclitaxel-resistant disease. Analyses were initially conducted in November 2020. Initial results were previously published in the British Journal of Cancer and demonstrated the efficacy and safety of weekly ixabepilone with or without biweekly bevacizumab in chemotherapy-resistant ovarian cancer.2
The trial’s end points of PFS (HR, 0.33; 95% CI, 0.19-0.55; P < .001) and OS (HR, 0.52; 95% CI, 0.31-0.87; P = .006) were met with the doublet vs single-agent ixabepilone. No new safety signals were observed.
Updated best ORR, PFS, and OS in a mature dataset were reported in the current analysis.1
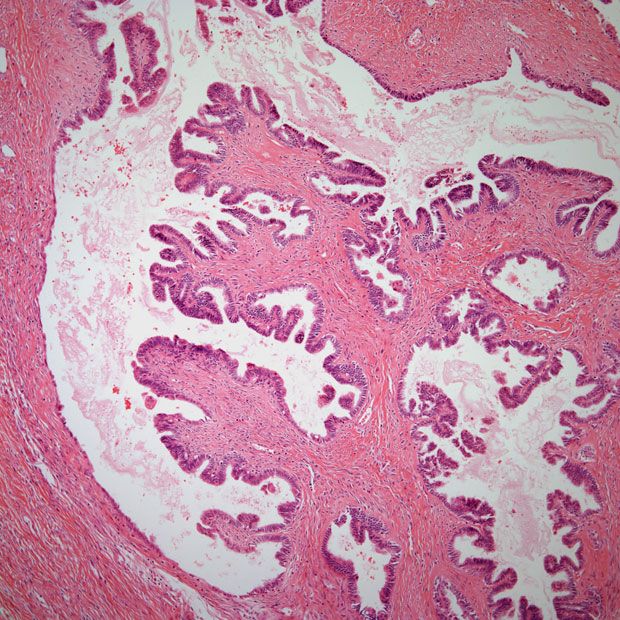
The investigator-initiated, open-label trial enrolled patients 18 years of age or older with histologically confirmed, platinum-resistant or -refractory epithelial ovarian, fallopian tube, or primary peritoneal carcinoma. Patients were required to have measurable disease per RECIST v1.1 criteria, an ECOG performance status of 0 to 2, and prior exposure to paclitaxel every 3 weeks or weekly. Prior debulking was permitted, and there was no limit on prior lines of therapy received.1,3
All patients on the trial received 20 mg/m2 of intravenous (IV) ixabepilone on days 1, 8, and 15 of a 28-day treatment cycle. Those in the combination arm also received 10 mg/kg of IV bevacizumab on days 1 and 15. Treatment continued until disease progression, unacceptable toxicity, or death. Participants were stratified based on prior bevacizumab treatment.
Regarding statistical analyses, the Kaplan-Meier method was utilized to analyze survival data, and two-sided Fisher’s exact tests were used to compare response rates. In subgroup analyses, data were illustrated with Forest plots, and 2-tailed Wald tests were utilized for analysis.1
Patients who experienced disease progression within 6 months of treatment with paclitaxel/docetaxel administration were considered taxane-resistant; those who progressed during treatment with a taxane or demonstrated disease persistence in an end-of-treatment assessment, prompting subsequent treatment, were classified as taxane-refractory. All other patients were considered taxane-sensitive.
The primary end point of the trial was PFS. Key secondary end points included OS, ORR, and safety.3
A total of 76 patients were enrolled onto the study and randomly assigned to treatment. The median number of prior lines across both arms was 4, and groups did not differ according to taxane-free interval. The majority of patients were refractory/resistant to paclitaxel in both the monotherapy arm (51%) and the combination arm (67%).1
As of the data cutoff of March 29, 2023, 75 PFS events and 70 deaths occurred. Although 59% of patients in the monotherapy arm and 64% of patients in the combination arm required dose reduction, PFS or OS benefit was not greatly decreased after undergoing 2 or more dose reductions.
Additional data showed the PFS and OS benefits were still observed following dose reductions. HRs for PFS were 0.49 (90% CI, 0.22-1.07; P = .074), 0.25 (90% CI, 0.10-0.62; P = 0.003) and 0.17 (90% CI, 0.05-0.54; P = 0.002) at de-escalating doses of 20 mg/m2, 16 mg/m2 and 12 mg/m2, respectively. Accompanying OS HRs were 0.70 (90% CI, 0.33-1.49; P = .354), 0.60 (90% CI, 0.26-1.36; P = .216) and 0.67 (90% CI, 0.25-1.63; P = .438) for those dose reductions, respectively.
References
- Roque D, Siegel E, Buza N, et al.Randomized phase II trial of weekly ixabepilone with or without biweekly bevacizumab for platinum-resistant or refractory ovarian/fallopian tube/primary peritoneal cancer: Updated survival and subgroup analyses. Presented at the Society of Gynecologic Oncology 2024 Annual Meeting on Women’s Cancer; San Diego, CA; March 16-18, 2024.
- Roque DM, Siegel ER, Buza N, et al. Randomised phase II trial of weekly ixabepilone ± biweekly bevacizumab for platinum-resistant or refractory ovarian/fallopian tube/primary peritoneal cancer. Br J Cancer. Published online February 11, 2022. doi:10.1038/s41416-022-01717-6
- Evaluation of Weekly Ixabepilone With or Without Biweekly Bevacizumab. ClinicalTrials.gov. Updated November 21, 2023. Accessed March 19, 2024. https://clinicaltrials.gov/study/NCT03093155