Caring for Patients With Serious Mental Illness: Guide for the Oncology Clinician
Veronica B. Decker, DNP, MBA, APRN, PMHCNS-BC, and colleagues discuss how to care for patients with cancer and serious mental illness.
Oncology (Williston Park). 2022;36(7):450-459.
DOI: 10.46883/2022.25920966
Challenges for Patients With Cancer and Serious Mental Illness
Advances in cancer care have resulted in improved cancer survival in the general population,1 but decades of evidence reveal that individuals with serious mental illness (SMI) experience poorer quality of cancer care and disproportionate cancer mortality.2-5 SMI, encompassing mental disorders such as schizophrenia, bipolar disorder, or major depressive disorder that significantly impede functioning,6,7 affects more than 13 million adults in the United States.8 Barriers to care for patients with SMI include late-stage cancer diagnoses at initial contact due to lower rates of cancer screening9,10; fragmented or inadequate psychosocial care, which may result in uncontrolled psychiatric symptoms11; and increased risk of medication interactions with cancer therapies.12 This population has higher incidence of comorbidities,13 smoking,14 obesity,15 and substance abuse14; fewer support systems for navigating cancer care16; and higher incidence of cognitive deficits that interfere with illness understanding and decision-making.17 Patients’ reluctance to share mental health history, deriving from traumatic experiences with discrimination, is also a common barrier and can lead to delays in psychiatric referral.18
Historically, people with SMI have experienced mental health discrimination. Common misperceptions include that they are dangerous, unpredictable, uncooperative, incapable of working, and/or unable to participate in research studies.19,20 Self-stigma, the process of internalizing negative stereotypes and applying them to oneself, can also contribute to lower rates of disclosing psychiatric history and may deter help-seeking completely.21 In a meta-analysis, a majority of nonpsychiatric medical physicians believed that people with SMI were more dangerous than cohorts with less serious psychiatric diagnoses. Although these physicians were amenable to seeing patients with SMI, they worried about the amount of time required as well as potential nonadherence to treatment.7 Clinician inexperience can also contribute to delays and misdiagnoses. For example, implicit bias may occur if the clinician ascribes a patient’s physical symptoms to mental illness, which can lead to delays in specialty referrals and initiation of treatment.22 Structural discrimination, referring to discriminatory institutional policies or laws that inhibit opportunities for marginalized populations, can also curb oncology specialists’ investment in mental health training or accessing mental health services for their patients.23 Moreover, since patients with SMI have higher incidence of substance use or abuse, oncology clinicians may miss opportunities to improve cancer treatment outcomes and survivorship if they do not assess for this and refer patients to addiction experts.24
Overcoming Barriers With Patients With SMI
Collaborative care approaches that integrate psychological and physical care have demonstrated clinical effectiveness25,26 and cost-effective access to care for a variety of health conditions among different populations and across practice settings.27 Why, then, haven’t these approaches been more widely adopted in oncology settings? The integration process may be perceived as too complex, requiring more time than oncology clinicians can devote to it without sacrificing care quality. Practical strategies exist, however, for overcoming some of the barriers with patients with SMI, beginning with patient-provider communication.28
Establishing Rapport for Effective Communication
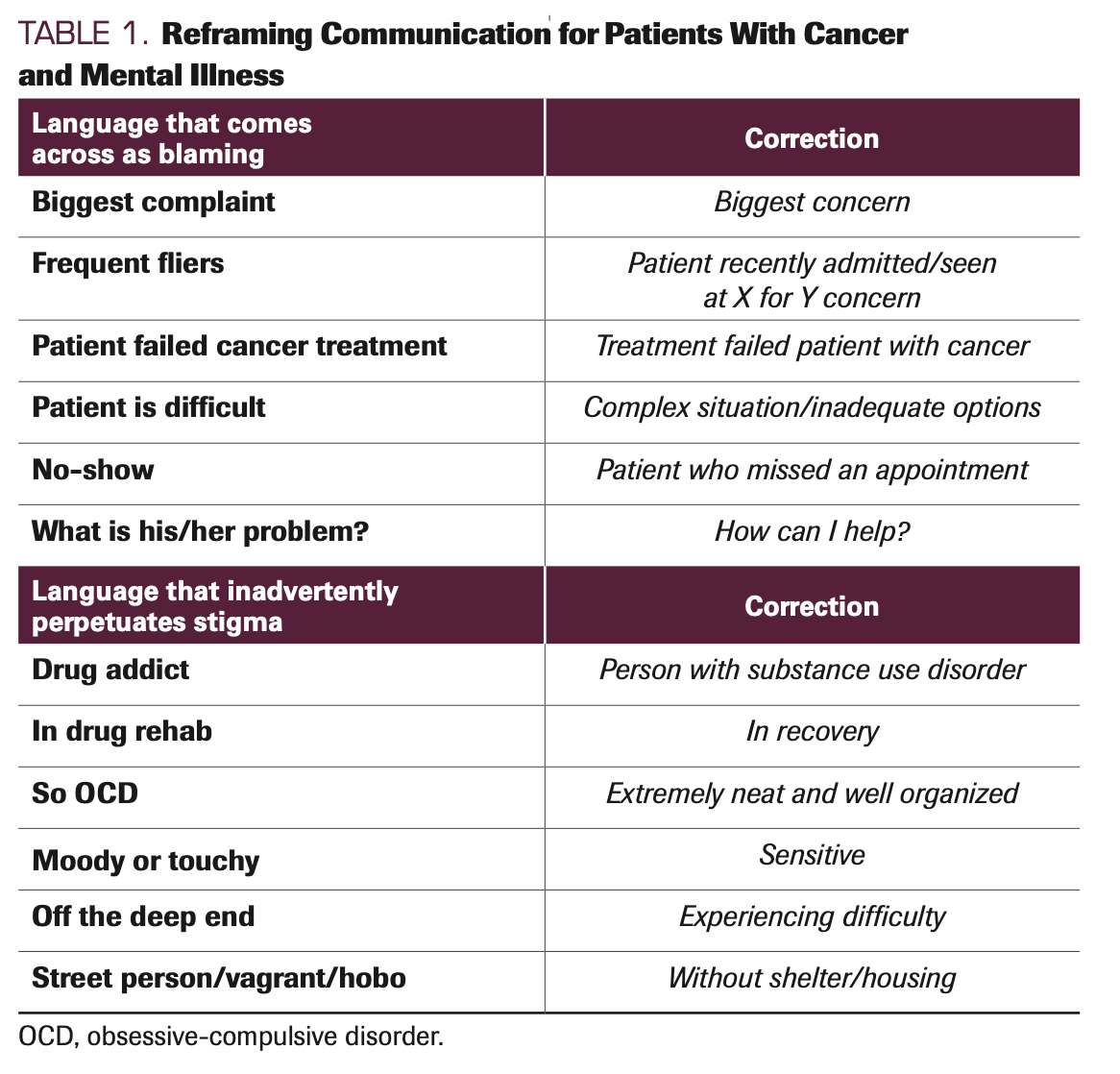
Patients and clinicians have recommended establishing fast rapport by using person-first language, a type of linguistic approach that focuses on the person as a unique individual and not on the person’s condition or diagnosis.29 In this approach, an individual’s medical diagnosis follows them as a human being, not the other way around: a patient with cancer rather than a cancer patient. Person-first language has been taught in most health professions programs for decades and is mandated by most scholarly journals as an important aspect of cultural competence in health care. It demonstrates the power of language to raise consciousness about and respect for all patients, and it affirms patients’ autonomy and the right to identify themselves however they choose. Despite its obvious significance, it is nonetheless infrequently used in clinical practice.30 To initiate person-first language with patients with SMI, clinicians and their staffs can show sensitivity and respect by first asking how they would like to be addressed (eg, Ms Smith, Pamela, Pam, Ms Pam). This can be followed with open-ended questions to find out about their current circumstances, hopes, fears, and possible adherence barriers, and how they feel the oncology team can be helpful. Clinicians can tailor their language, slowing their speech and using concrete terms and visual aids to explain procedures. As staff members become aware of how their perceptions of patients may impact their language and professionalism, practicing person-first thinking and language may boost their confidence in knowing how to communicate with all patients and each other as well.31 Table 1 contrasts examples of blaming and stigma-perpetuating language with corrections in person-first language.
TABLE 1. Reframing Communication for Patients With Cancer and Mental Illness
Trauma-Informed Care
It is important for staff to realize that many patients with SMI have had a lifetime of exposure to trauma. These experiences have left them deeply distressed or disturbed, beginning with abuse and/or neglect in their early years and continuing into adulthood.32,33 In a study of individuals with SMI spanning 30 years, participants reported a mean lifetime prevalence rate of 47% for physical abuse, 37% for sexual abuse, and 30% for posttraumatic stress disorder, compared with prevalence rates in the general population of 21%, 23%, and 7%, respectively.34 According to the US Substance Abuse and Mental Health Services Administration, traumatic experiences often adversely impact people in every functional sphere: physically, mentally, emotionally, socially, and spiritually.35 Common forms of trauma include familial physical and sexual violence; childhood abuse and/or neglect; neighborhood/community violence, including bullying, gang wars/shootings, robberies, and rape; and natural disasters. Types of trauma that are less understood include racism as well as other stigma-related or prejudice-related incidences; these include being ridiculed or treated differently because of one’s mental illness or disability, historical trauma (eg, genocide), and other types of long-term hardship, such as extreme poverty.36
Trauma-informed care is an approach that emphasizes sensitivity to the impact of trauma in patients’ lives. Health care professionals’ heightened sensitivity is essential for helping patients feel safe and for not inadvertently triggering patients’ previous trauma responses while they cope with all the challenges of a cancer diagnosis and treatment.36 To help patients feel safe and more in control, 2 of the aims of trauma-informed care, clinicians can check for illness understanding, offer options, and empower patients as ultimate authorities who will decide what happens to their own bodies regarding treatment preferences and goals. Patients with SMI, however, may require more explanation about their cancer and treatment options, including such explanations in visual formats, as well as more time to process what has been presented to them. It may be helpful to ask patients their preferences about staff member gender and to promote continuity of care when possible. In this regard, for example, a staff member whom patients have already met, trained in person-first language and trauma-informed care, can accompany them to consults for additional support, to answer questions or concerns afterward, and to provide materials to study at home when they are not under pressure. This type of additional support may be particularly helpful when cancer care requires invasive procedures, such as colonoscopies; imaging and procedures related to gastrointestinal, genitourinary, gynecologic, and breast cancers; and mask fitting prior to radiation. Oncology clinicians can invest in person-first and trauma-informed literature and workshops for themselves and staff (much of it free)37,38 that will help overcome patients’ previous experiences with discrimination and improve communication.39 Tailored approaches can be discussed with staff members.
Screening and Identification of Mental Illness
The American Society of Clinical Oncology and the Commission on Cancer mandated psychosocial distress screening as a quality care standard in 2015,40 but only 50% to 65% of patients with cancer are currently screened for distress.41 Reasons given for the slow implementation rate are lack of staff training42 and fragmentation between mental health and oncology care.43 Mental health clinics are often geographically isolated from main health care structures,44 with separate electronic health records (EHRs).12 If communication between oncology and mental health care teams exists at all, it is likely infrequent.16 Moreover, even if measures are used to assess patients’ distress in oncology clinics, they are not typically meant to assess SMI, so serious psychiatric disorders may be missed.12,16,43,44
The most practical method for identifying SMI may be assessment of patients’ medications. A staff member can compile a list of commonly prescribed psychotropic medications for SMI that can be checked against patients’ reported medications or EHR medication history. In a recent international study of 13,200 primary care clinicians, only 40% in the United States reported frequently coordinating with social services,45 but disruptions in patients’ psychiatric care and/or failure to manage symptoms result in decreased adherence to cancer treatment and decreased quality of life and survivorship,46 accenting inequities in care.47 If patients are taking a medication commonly prescribed to treat mental illness, clinicians can ask about patients’ prescribers, so they can be contacted right away. If patients do not list any psychotropic medications in the medical record, clinicians need to remember they may be reluctant to share their mental health history because of stigma-related experiences. Gentle questioning to find out the cause of reticence can open the door to building trust. Psychological safety enables effective communication,48 and person-first and trauma-informed communication strategies have been demonstrated as facilitators of psychological safety with patients, caregivers, and staffs.49 Additionally, not all patients have a formal diagnosis of mental illness or insight into that diagnosis. It is helpful to ask patients if they have a history of seeing a social worker or psychiatrist or if they have ever received a mental health diagnosis. If they are accompanied by a caregiver, it is also important to partner with them to obtain additional history.
Referring Patients With SMI to Clinical Trials
Historically, inequities in care for patients with SMI who have cancer have been exacerbated by lack of research. Almost 25 years ago, a National Cancer Institute Clinical Trials Program Review Group asserted there were “too many exclusion criteria in the current clinical trials system” and “entry criteria for all studies need to be simplified and broadened.”50,51 Currently, however, half of the most circulated and cited US clinical trials, including oncology trials, exclude patients with psychiatric conditions.52 Oncology clinicians reported that their main reasons for nonreferral of patients with SMI to trials were the patients’ possible lack of motivation to participate, inability to provide informed consent, inability to complete protocols and return for follow-up appointments; the potential for increased patient burden and compromised safety; and perceived risk and additional burden for investigators.19 However, when patients with SMI, including schizophrenia, are provided with more details about the study and given more time to process this information, their motivation and capacity to consent is improved.53,54 In a trial bridging cancer care and psychiatric care, patients had high rates of consent, symptoms remained stable or improved during the trial, and they were able to complete the trial.54 People with SMI have also demonstrated the ability to successfully participate in remote interventions. Recently, 315 people with confirmed diagnoses of bipolar disorder, major depressive disorder, and/or schizophrenia or schizoaffective disorder were recruited from advertisements placed in large search engines, and they participated in a fully remote smartphone intervention for reducing severity of psychiatric symptoms and increasing self-esteem. Although retention was a challenge, some of the main reasons oncologists gave for not referring (eg, lack of motivation, inability to provide consent, and burden for investigators) were not encountered, and results indicated that people with SMI can be successfully recruited and treated remotely for reduced symptom severity.55
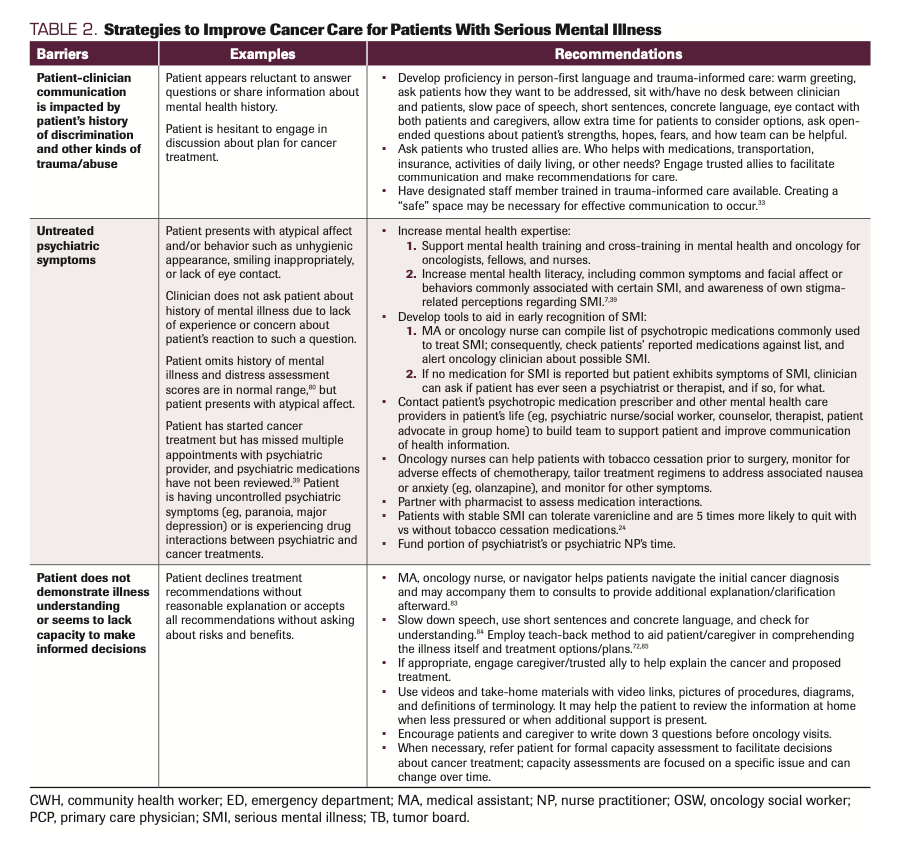
Oncology clinicians may believe that they are protecting their patients by not referring them for trials. Ironically, lack of research drives misperceptions about the ability of people with SMI to participate in research,16 and participation in trials may be needed to dispel these limiting misperceptions that lead to care inequities.39,56 Table 2 describes types and examples of barriers that might occur with patients with SMI and practical recommendations for overcoming them.
TABLE 2. Strategies to Improve Cancer Care for Patients With Serious Mental Illness
Pulling the Team Together to Enhance Care for Patients With Mental Illness
As patients with SMI begin the challenging process of managing the demands of cancer treatment, ongoing mental health care is needed to address their complex psychological needs and help them be successful. The clinical team can brainstorm the most efficient way to tailor the existing practice for an integrated approach57 to increase access to the psychiatric expertise patients need. Most patients will have someone from mental health or primary care managing their medications. Who on the team can take responsibility for initial and ongoing engagement with the patient’s mental health team?
Psychiatrists or psychologists with additional training in pharmacology can provide initial and ongoing assessment of psychiatric symptoms, illness understanding, and decisional capacity of patients with SMI. Updates regarding medication efficacy, adherence, and adverse effects should be shared not only between oncology and psychiatric clinicians but with people dispensing medication to patients, whether they are caregivers, home health nurses, or staff members at a group home.58 Psychiatric clinicians are also more likely to provide treatment that can address exacerbated symptoms expected in cancer care, thus potentially reducing emergency department visits and hospitalizations.59
Although many patients with SMI have a psychiatric clinician prescribing their medications, many others work with their primary care physicians (PCPs) for medication management. Currently, PCPs provide about a third of care for patients with SMI60; thus, they may value rapid access to psychiatric expertise or to a consultant when needed. They may also bring their own multidisciplinary alliances to the table.61 With greater projected gaps in the psychiatric clinician workforce and greater demand for services,62 PCPs will likely play an even larger role for many patients during the survivorship period. Regardless of situation or prescribing practices, PCPs are allies who may have considerable influence with patients and caregivers, and they may offer excellent advice for building trust with and engaging patients in cancer care.
Oncology nurses and advanced practice clinicians fill key roles in a team prepared for all types of patients with comorbidities, taking the lead in identifying SMI and making referrals to psychiatric clinicians for care and assessment of patients’ decisional capacity. As experts in symptom management and tracking, oncology nurses are often the first to note changes in patients’ symptoms and/or treatment adherence barriers. They may help conduct chemotherapy teaching and tailor medication guidance for patients with SMI in collaboration with pharmacists, who should be able to help with assessment of medication interactions. Common challenges include tailoring antiemetics and decreasing the risk of mood instability when steroids are used. Nurses may also fulfill 2 important aspects of caring for patients that can build trust and adherence to cancer care: establishing tailored communication (eg, phone calls, texts) to remind patients/caregivers about appointments, and supporting the emotional needs of caregivers, who typically keep patients on track.63,64 Caregivers routinely drive and accompany patients to appointments, and they typically pick up, administer, and monitor medications and schedules. Support is particularly important for caregivers of patients with schizophrenia or severe bipolar disorder, as these patients may have difficulty communicating about symptoms, organizing thoughts and scheduling, or lack insight regarding the urgency for treatment. When faced with the additional complexities of cancer care, caregivers are at particular risk for distress and burnout. They frequently feel helpless, inadequate, overwhelmed, and uncertain, especially when they cannot identify or access health care resources for help.65 Their emotional and physical health must thus be considered throughout the cancer care continuum.63-65 Oncology nurses and/or social workers may be able to help them cope with emotional stressors and exhaustion by offering educational resources and individual and/or family support groups. Of note, caregivers for patients with SMI are less likely to be spouses and include other family members and community mental health staff from group living environments.54
Many cancer centers have oncology social workers (OSWs) and navigators. OSWs can also conduct psychosocial assessments to identify sources of distress, psychiatric comorbidity, and patients’ unique needs. They can make early referrals to psychiatric services and may serve as liaisons between the oncology team and mental health team to prevent disruptions in cancer care.11 As licensed professionals, they can, like oncology nurses, provide evidence-based treatments/brief therapies, follow-up, and education. Almost half (48.4%) of caregivers, however, reported unmet service needs as their biggest stressor,66 and connecting them to support services is one of the expert skills of a navigator.
Navigators can build trust with patients and facilitate their day-to-day care, helping them deal with the complexities of the system by connecting them to services as they progress through the care continuum.67,68 Often, they serve as point persons for communication, so when patients have questions or concerns, they call the navigator. Lay navigators, who do not have formal health care training, can offer emotional support, help with coordination of appointments, and assist in addressing barriers related to social determinants of health, such as impaired health literacy or lack of transportation or childcare.69 Community health workers (CHWs) are nonclinical public health workers who possess deep knowledge of the community a patient is from. Like navigators, CHWs may serve as liaisons between patients and health care teams, providing outreach, education, and informal counseling, and they may accompany patients to oncology consults and other appointments.70
Tumor Boards
Information about patients with SMI from all the people involved in their care presents a multidimensional view of these patients’ unique circumstances, barriers, facilitators, preferences, and goals, which are key considerations for developing workable treatment plans. Because tumor boards are composed largely of oncology specialists,71 it may happen that patients’ psychosocial histories, medical and psychiatric comorbidities, complex circumstances and barriers, and preferences/goals for treatment are minimally considered or omitted entirely.71 These gaps in knowledge can limit consideration of barriers to cancer care, contribute to delays in care, and in some cases, prevent patients with SMI from receiving the care they need.72 If community mental health clinicians and PCPs are invited to and attend tumor boards when their patients are being discussed, their input may help to inform proactive plans for both cancer and mental health treatment and address care barriers.
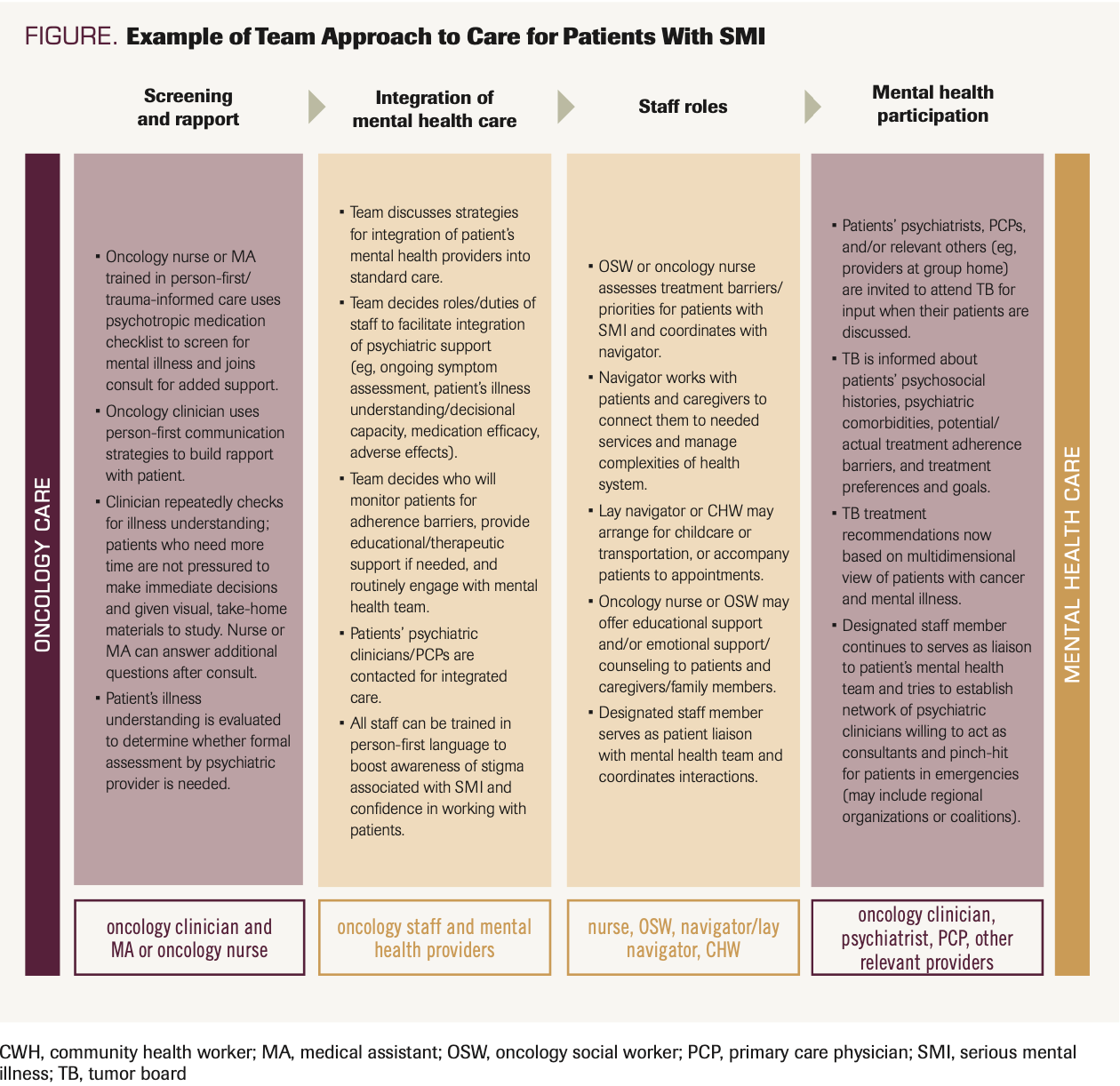
Collaborative care models use a team-based approach to integrate mental health services in primary or specialty care to increase access to integrated mental health services for patients with cancer.73,74 We recognize that, given limited time and resources, it will not be feasible for all oncology practices to implement all aspects of a collaborative care model. Therefore, we aimed to provide pragmatic recommendations that can be adapted to different practice settings, regardless of size or affiliation with larger health care systems. The Figure illustrates the steps an independent oncology practice can take to connect with and integrate a patient’s mental health team as part of routine cancer care. Next, we present recent developments in collaborative care approaches for patients with SMI.
FIGURE. Example of Team Approach to Care for Patients With SMI
Recent Developments
Adapting the Collaborative Care Model for SMI and Cancer
To date, few teams that care for people with serious medical illnesses, like cancer, are staffed with cross-trained experts in mental health care.75 The collaborative care model is a promising approach that increases access to mental health expertise and has been found to improve patients’ psychiatric symptoms in more than 70 randomized trials.54,58,76-78 However, patients with SMI and cancer have traditionally been excluded from collaborative care trials. In 2019, Irwin and colleagues piloted a person-centered collaborative care model for patients with SMI.54,79 Key components of the intervention, called Bridge, included (1) early screening, identification, and tracking of patients with SMI, (2) person-centered, team-based care, including psychiatry and social work, and (3) collaboration between the mental health intervention team and oncology to guide treatment recommendations and integrate input from community-based mental health clinicians. The pilot trial demonstrated that the intervention was feasible and acceptable for patients with SMI, caregivers, and oncology clinicians. Results from the subsequent randomized clinical trial assessing the intervention’s efficacy in improving cancer outcomes for this population are forthcoming.54
Cancer care has the potential to be a healing opportunity for patients who have been marginalized in many areas of their lives. One of the core elements of person-centered collaborative care is the creation of patient-clinician partnerships. For example, oncology clinicians can support patients’ decision-making processes and empower them to decide what happens to their bodies regarding treatment preferences and goals. Person-first language and trauma-informed care can be used to initiate and safeguard the partnership to increase patient engagement in care, and there is evidence that engagement has the potential to improve both cancer and mental health outcomes.80 More research is under way that explores how person-centered collaborative care can impact health outcomes, quality of life, and patient satisfaction.74
Another opportunity to gather information about marginalized populations is through cultivation of a population-based registry, a tool that can capture important data (eg, cancer type, stage of diagnosis at consult, physical and psychiatric comorbidities, history of screenings) and facilitate both early identification and systematic tracking. Population-based management using data available in commercial EHRs can be done by any trained team member and can be an efficient strategy to fill information gaps about a specific population and identify unmet needs. This information may be aggregated with mandated efforts for distress screening to identify a population at high risk for gaps in cancer care delivery using International Classification of Diseases, Tenth Edition codes, problem lists, or commonly prescribed medications. Our research team, for example, developed a population-based registry for screening EHRs to identify patients with both SMI and a new cancer diagnosis; such a registry can facilitate referrals for consultation and clinical trials as well as prioritize patients experiencing challenges accessing cancer care.81
Adapting the Tumor Board Model for SMI and Cancer
Virtual multidisciplinary tumor boards or conferences are gaining ground as a strategy to increase access to multispecialty cancer care for patients in underserved settings. Virtual approaches enable providers located in distant settings to share information and may help ensure appropriate dispersal of resources and access to specialty expertise, as has been demonstrated during the COVID-19 pandemic.82 These models also hold promise for integrating mental health and cancer care and may be considered for building collaborations between comprehensive cancer centers and community-based settings that serve individuals with SMI. More research is needed, however, to confirm whether virtual multidisciplinary conferences have the capacity to increase access to quality cancer care for patients with SMI.
Conclusions
In this review, we focused on supporting oncologists in their efforts to address the complex needs of patients with serious mental illness. We provided practical recommendations for overcoming barriers to cancer care and provided a simple method for identifying the population at the time of cancer diagnosis. We offered evidence-based strategies for improved patient-clinician communication and partnership, methods to build illness understanding, and strategies to prepare and support patients undergoing treatment procedures. We emphasized the importance of ongoing collaborations with patients’ psychiatric providers as part of routine care, and in this vein, the relevance of inviting patients’ mental health clinicians to tumor boards for their input. We also recommended referral of patients with SMI to clinical trials to dispel misperceptions about SMI and this population’s ability to participate, and to provide critical evidence to guide cancer care delivery with potential to mitigate disparities in cancer outcomes. Finally, we discussed innovative approaches to care delivery, including adaptation of the collaborative care model and the tumor board model, for increasing access to evidence-based mental health and cancer care for a marginalized population.
Disclosure: The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
Corresponding Author:
Veronica B. Decker, DNP, MBA, APRN, PMHCNS-BC
University of Central Florida
12201 Research Parkway
Orlando, FL 32826
Tel: 407-823-5025 | Fax: 407-823-5675 | veronica.decker@ucf.edu
Authors Affiliations:
Veronica B. Decker, DNP, MBA, APRN, PMHCNS-BC1; Zoe E. Nelson, BA2; Amy Corveleyn, MSW3; Priya K. Gopalan, MD, MPH4; and Kelly Irwin, MD, MPH3
1University of Central Florida, Orlando, FL
2Massachusetts General Hospital, Boston, MA
3Massachusetts General Hospital – Cancer Center, Boston, MA
4Orlando VA Medical Center, Orlando, FL
References
- Facts & Figures 2021 reports another record-breaking 1-year drop in cancer deaths. News release. American Cancer Society; January 12, 2021. Accessed November 15, 2021. https://bit.ly/3wveRJo
- Irwin KE, Freudenreich O, Peppercorn J, Taghian AG, Freer PE, Gudewicz TM. Case records of the Massachusetts General Hospital. case 30-2016. a 63-year-old woman with bipolar disorder, cancer, and worsening depression. N Engl J Med. 2016;375(13):1270-1281. doi:10.1056/NEJMcpc1609309
- Solmi M, Firth J, Miola A, et al. Disparities in cancer screening in people with mental illness across the world versus the general population: prevalence and comparative meta-analysis including 4 717 839 people. Lancet Psychiatry. 2020;7(1):52-63. doi:10.1016/S2215-0366(19)30414-6
- Manderbacka K, Arffman M, Lumme S, et al. The effect of history of severe mental illness on mortality in colorectal cancer cases: a register-based cohort study. Acta Oncol. 2018;57(6):759-764. doi:10.1080/0284186X.2018.1429649
- Davis LE, Bogner E, Coburn NG, et al. Stage at diagnosis and survival in patients with cancer and a pre-existing mental illness: a meta-analysis. J Epidemiol Community Health. 2020;74(1):84-94. doi:10.1136/jech-2019-212311
- Grove LR, Gertner AK, Swietek KE, et al. Effect of enhanced primary care for people with serious mental illness on service use and screening. J Gen Intern Med. 2021;36(4):970-977. doi:10.1007/s11606-020-06429-2
- Stone EM, Chen LN, Daumit GL, Linden S, McGinty EE. General medical clinicians’ attitudes toward people with serious mental illness: a scoping review. J Behav Health Serv Res. 2019;46(4):656-679. doi:10.1007/s11414-019-09652-w
- Mental illness. National Institute of Mental Health. Updated January 2022. Accessed February 8th, 2022. https://bit.ly/3NqvJGD
- Carney CP, Jones LE. The influence of type and severity of mental illness on receipt of screening mammography. J Gen Intern Med. 2006;21(10):1097-1104. doi:10.1111/j.1525-1497.2006.00565.x
- Xiong GL, Bermudes RA, Torres SN, Hales RE. Use of cancer-screening services among persons with serious mental illness in Sacramento County. Psychiatr Serv. 2008;59(8):929-932. doi:10.1176/ps.2008.59.8.929
- Leahy D, Donnelly A, Irwin K, D’Alton P. Barriers and facilitators to accessing cancer care for people with significant mental health difficulties: a qualitative review and narrative synthesis. Psychooncology. 2021;30(12):2012-2022. doi:10.1002/pon.5848
- Deshields TL, Wells-Di Gregorio S, Flowers SR, et al. Addressing distress management challenges: recommendations from the consensus panel of the American Psychosocial Oncology Society and the Association of Oncology Social Work. CA Cancer J Clin. 2021;71(5):407-436. doi:10.3322/caac.21672
- Mitchell AJ, Malone D, Carney Doebbeling C. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry. 2009;194(6):491-499. doi:10.1192/bjp.bp.107.045732
- Firth J, Siddiqi N, Koyanagi A, et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6(8):675-712. doi:10.1016/S2215-0366(19)30132-4
- Hjorth P, Davidsen AS, Kilian R, Skrubbeltrang C. A systematic review of controlled interventions to reduce overweight and obesity in people with schizophrenia. Acta Psychiatr Scand. 2014;130(4):279-289. doi:10.1111/acps.12245
- Irwin KE, Henderson DC, Knight HP, Pirl WF. Cancer care for individuals with schizophrenia. Cancer. 2014;120(3):323-334. doi:10.1002/cncr.28431
- McFarland DC, Blackler L, Hlubocky FJ, et al. Decisional capacity determination in patients with cancer. Oncology (Williston Park). 2020;34(6):203-210.
- Rüsch N, Müller M, Ajdacic-Gross V, Rodgers S, Corrigan PW, Rössler W. Shame, perceived knowledge and satisfaction associated with mental health as predictors of attitude patterns towards help-seeking. Epidemiol Psychiatr Sci. 2014;23(2):177-187. doi:10.1017/S204579601300036X
- Irwin KE, Moy B, Fields LE, Callaway CA, Park ER, Wirth L. Expanding access to cancer clinical trials for patients with mental illness. J Clin Oncol. 2019;37(18):1524-1528. doi:10.1200/JCO.18.01881
- Vaccari P, Ramírez-Vielma R, Saldivia S, et al. Stigma towards people with a diagnosis of severe mental disorder in primary healthcare centers: perspectives of service users and health teams in Chile. Int J Ment Health Syst. 2020;14:6. doi:10.1186/s13033-020-0340-5
- Pattyn E, Verhaeghe M, Sercu C, Bracke P. Public stigma and self-stigma: differential association with attitudes toward formal and informal help seeking. Psychiatr Serv. 2014;65(2):232-238. doi:10.1176/appi.ps.201200561
- Ungar T, Knaak S, Mantler E. Making the implicit explicit: a visual model for lowering the risk of implicit bias of mental/behavioural disorders on safety and quality of care. Healthc Manage Forum. 2021;34(2):72-76. doi:10.1177/0840470420953181
- Horrill TC, Browne AJ, Stajduhar KI. Equity-oriented healthcare: what it is and why we need it in oncology. Curr Oncol. 2022;29(1):186-192. doi:10.3390/curroncol29010018
- Kaiser EG, Prochaska JJ, Kendra MS. Tobacco cessation in oncology care. Oncology. 2018;95(3):129-137. doi:10.1159/000489266
- Camacho EM, Davies LM, Hann M, et al. Long-term clinical and cost-effectiveness of collaborative care (versus usual care) for people with mental-physical multimorbidity: cluster-randomised trial. Br J Psychiatry. 2018;213(2):456-463. doi:10.1192/bjp.2018.70
- Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve depression treatment guidelines. J Clin Psychiatry. 1997;58(suppl 1):20-23.
- Walker J, Sharpe M. Integrated management of major depression for people with cancer. Int Rev Psychiatry. 2014;26(6):657-668. doi:10.3109/09540261.2014.981512
- Institute of Medicine (US) Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting; Adler NE, Page AEK, eds. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. National Academies Press; 2008. Accessed February 14, 2022. https://www.ncbi.nlm.nih.gov/books/NBK4023/#:~:text=https%3A//www.ncbi.nlm.nih.gov/books/NBK4023/
- Guidelines: How To Write About People with Disabilities. 9th ed. The University of Kansas Research & Training Center on Independent Living. Accessed February 15th, 2022. https://rtcil.org/guidelines
- Crocker AF, Smith SN. Person-first language: are we practicing what we preach? J Multidiscip Healthc. 2019;12:125-129. doi:10.2147/JMDH.S140067
- Nelson Z, Shaqour S, Flores EJ, et al. Lessons learned to advanced person-centered outcomes research and virtual engagement with underrepresented populations: engaging adults with serious mental illness. Presented at: American Psychosocial Oncology Society 19th Annual Conference; March 9-11, 2022; virtual. https://bit.ly/3PtBmWF
- Isobel S. Is trauma informed care possible in the current public mental health system? Australas Psychiatry. 2021;29(6):607-610. doi:10.1177/10398562211028625
- Isobel S, Gladstone B, Goodyear M, Furness T, Foster K. A qualitative inquiry into psychiatrists’ perspectives on the relationship of psychological trauma to mental illness and treatment: implications for trauma-informed care. J Ment Health. 2021;30(6):667-673. doi:10.1080/09638237.2020.1714012
- Song H, Fall K, Fang F, et al. Stress related disorders and subsequent risk of life threatening infections: population based sibling controlled cohort study. BMJ. 2019;367:I5784. doi:10.1136/bmj.l5784
- Substance Abuse and Mental Health Services Administration. A Treatment Improvement Protocol: Trauma-Informed Care in Behavioral Health Services. HHS; 2014. Accessed April 10, 2022. ttps://store.samhsa.gov/product/TIP-57-Trauma-Informed-Care-in-Behavioral-Health-Services/SMA14-4816
- Sweeney A, Filson B, Kennedy A, Collinson L, Gillard S. A paradigm shift: relationships in trauma-informed mental health services. BJPsych Adv. 2018;24(5):319-333. doi:10.1192/bja.2018.29
- Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc Manage Forum. 2017;30(2):111-116. doi:10.1177/0840470416679413
- Menschner C, Maul A. Key ingredients for successful trauma-informed care implementation. Center for Health Care Strategies. April2016. Accessed May 20, 2022. https://bit.ly/3G7muIU
- Thornicroft G, Mehta N, Clement S, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016;387(10023):1123-1132. doi:10.1016/S0140-6736(15)00298-6
- Wagner LI, Spiegel D, Pearman T. Using the science of psychosocial care to implement the new American College of Surgeons Commission on Cancer distress screening standard. J Natl Compr Canc Netw. 2013;11(2):214-221. doi:10.6004/jnccn.2013.0028
- Zebrack B, Kayser K, Bybee D, et al. A practice-based evaluation of distress screening protocol adherence and medical service utilization. J Natl Compr Canc Netw. 2017;15(7):903-912. doi:10.6004/jnccn.2017.0120
- Dekker J, Graves KD, Badger TA, Diefenbach MA. Management of distress in patients with cancer – are we doing the right thing? Ann Behav Med. 2020;54(12):978-984. doi:10.1093/abm/kaaa091
- White S. Barriers to the delivery and uptake of psychosocial care in adult cancer services: a literature review. Cancer Nursing Practice. 2021;20(4):29-34. doi:10.7748/cnp.2021.e1760
- Fann JR, Ell K, Sharpe M. Integrating psychosocial care into cancer services. J Clin Oncol. 2012;30(11):1178-1186. doi:10.1200/JCO.2011.39.7398
- Doty MM, Tikkanen R, Shah A, Schneider EC. Primary care physicians’ role in coordinating medical and health-related social needs in eleven countries. Health Aff (Millwood). 2020;39(1):115-123. doi:10.1377/hlthaff.2019.01088
- Pozo-Kaderman C, Pirl WF. Depression and anxiety disorders in patients with cancer. Psychiatric Times. 2017;34(3).
- Irwin KE, Park ER, Shin JA, et al. Predictors of disruptions in breast cancer care for individuals with schizophrenia. Oncologist. 2017;22(11):1374-1382. doi:10.1634/theoncologist.2016-0489
- Jain AK, Fennell ML, Chagpar AB, Connolly HK, Nembhard IM. Moving toward improved teamwork in cancer care: the role of psychological safety in team communication. J Oncol Pract. 2016;12(11):1000-1011. doi:10.1200/JOP.2016.013300
- Callaway CA, Corveleyn AE, Barry MJ, Gorton EI, Nierenberg AA, Irwin KE. Lessons learned: building a coalition to advance equity in cancer and mental health care. Psychooncology. 2021;30(12):2087-2091. doi:10.1002/pon.5852
- Report of the National Cancer Institute Clinical Trials Program Review Group. National Cancer Institute Division of Extramural Activities. August 26, 1997. Accessed May 20, 2022. https://bit.ly/3wG0rF1
- Jin S, Pazdur R, Sridhara R. Re-evaluating eligibility criteria for oncology clinical trials: analysis of investigational new drug applications in 2015. J Clin Oncol. 2017;35(33):3745-3752. doi:10.1200/JCO.2017.73.4186
- Humphreys K, Blodgett JC, Roberts LW. The exclusion of people with psychiatric disorders from medical research. J Psychiatr Res. 2015;70:28-32. doi:10.1016/j.jpsychires.2015.08.005
- Carpenter WT Jr, Gold JM, Lahti AC, et al. Decisional capacity for informed consent in schizophrenia research. Arch Gen Psychiatry. 2000;57(6):533-538. doi:10.1001/archpsyc.57.6.533
- Irwin KE, Park ER, Fields LE, et al. Bridge: person-centered collaborative care for patients with serious mental illness and cancer. Oncologist. 2019;24(7):901-910. doi:10.1634/theoncologist.2018-0488
- Ben-Zeev D, Chander A, Tauscher J, et al. A smartphone intervention for people with serious mental illness: fully remote randomized controlled trial of CORE. J Med Internet Res. 2021;23(11):e29201. doi:10.2196/29201
- Gaynes B, Brown C, Lux LJ, et al. Relationship Between Use of Quality Measures and Improved Outcomes in Serious Mental Illness. Agency for Healthcare Research and Quality; 2015. Accessed February 28, 2022.
- Seely DM, Weeks LC, Young S. A systematic review of integrative oncology programs. Curr Oncol. 2012;19(6):e436-e461. doi:10.3747/co.19.1182
- Reilly S, Planner C, Gask L, et al. Collaborative care approaches for people with severe mental illness. Cochrane Database Syst Rev. 2013;(11):CD009531. doi:10.1002/14651858.CD009531.pub2
- Medical Director Institute. The Psychiatric Shortage: Causes and Solutions. March 29, 2017. Updated March 1, 2018. Accessed February 23, 2022. https://ewscripps.brightspotcdn.com/8d/40/f24438bd4a8d850f390e6fcf3211/psychiatric-shortage-national-council.pdf
- Jetty A, Petterson S, Westfall JM, Jabbarpour Y. Assessing primary care contributions to behavioral health: a cross-sectional study using Medical Expenditure Panel Survey. J Prim Care Community Health. 2021;12:21501327211023871. doi:10.1177/21501327211023871
- Planner C, Gask L, Reilly S. Serious mental illness and the role of primary care. Curr Psychiatry Rep. 2014;16(8):458. doi:10.1007/s11920-014-0458-8
- Jorgensen S, Dixon LB. The psychiatric workforce shortage. Psychiatr Serv. 2021;72(7):859-860. doi:10.1176/appi.ps.72701
- Caruso R, Nanni MG, Riba MB, Sabato S, Grassi L. The burden of psychosocial morbidity related to cancer: patient and family issues. Int Rev Psychiatry. 2017;29(5):389-402. doi:10.1080/09540261.2017.1288090
- Harrison R, Raman M, Walpola RL, Chauhan A, Sansom-Daly UM. Preparing for partnerships in cancer care: an explorative analysis of the role of family-based caregivers. BMC Health Serv Res. 2021;21(1):620. doi:10.1186/s12913-021-06611-0
- LeSeure P, Chongkham-Ang S. The experience of caregivers living with cancer patients: a systematic review and meta-synthesis. J Pers Med. 2015;5(4):406-439. doi:10.3390/jpm5040406
- Kent EE, Dionne-Odom JN. Population-based profile of mental health and support service need among family caregivers of adults with cancer. J Oncol Pract. 2019;15(2):e122-e131. doi:10.1200/JOP.18.00522
- Riley S, Riley C. The role of patient navigation in improving the value of oncology care. J Clin Pathwy. December 2016. Accessed May 20, 2022. https://bit.ly/3LD2u26
- Krok-Schoen JL, Oliveri JM, Paskett ED. Cancer care delivery and women’s health: the role of patient navigation. Front Oncol. 2016;6:2. doi:10.3389/fonc.2016.00002
- Meade CD, Wells KJ, Arevalo M, et al. Lay navigator model for impacting cancer health disparities. J Cancer Educ. 2014;29(3):449-457. doi:10.1007/s13187-014-0640-z
- Community health workers. American Public Health Association. Accessed February 14, 2022. https://bit.ly/3LwK0QY
- Specchia ML, Frisicale EM, Carini E, et al. The impact of tumor board on cancer care: evidence from an umbrella review. BMC Health Serv Res. 2020;20(1):73. doi:10.1186/s12913-020-4930-3
- Choi S, Choi J. Effects of the teach-back method among cancer patients: a systematic review of the literature. Support Care Cancer. 2021;29(12):7259-7268. doi:10.1007/s00520-021-06445-w
- Huang H, Forstein M, Joseph R. Developing a collaborative care training program in a psychiatry residency. Psychosomatics. 2017;58(3):245-249. doi:10.1016/j.psym.2016.12.006
- Using the Collaborative Care Model for special populations. American Psychiatric Association. Accessed February 14, 2022. https://bit.ly/3Lxz4CG
- Shalev D, Docherty M, Spaeth-Rublee B, et al. Bridging the behavioral health gap in serious illness care: challenges and strategies for workforce development. Am J Geriatr Psychiatry. 2020;28(4):448-462. doi:10.1016/j.jagp.2019.09.003
- O’Neill EA, Ratliff Black D. Collaborative care for individuals with bipolar disorder or schizophrenia and co-occurring physical health conditions: a systematic review. Soc Work Ment Health. 2017;15(6):705-729. doi:10.1080/15332985.2017.1306823
- Katon W, Unützer J, Wells K, Jones L. Collaborative depression care: history, evolution and ways to enhance dissemination and sustainability. Gen Hosp Psychiatry. 2010;32(5):456-464. doi:10.1016/j.genhosppsych.2010.04.001
- Ee C, Lake J, Firth J, et al. An integrative collaborative care model for people with mental illness and physical comorbidities. Int J Ment Health Syst. 2020;14(1):83. doi:10.1186/s13033-020-00410-6
- Irwin KE, Loscalzo ML. Witnessing unnecessary suffering: a call for action and policy change to increase access to psycho-oncology care. Psychooncology. 2020;29(12):1977-1981. doi:10.1002/pon.5599
- Loonen JJ, Ma Blijlevens N, Prins J, et al. Cancer survivorship care: person centered care in a multidisciplinary shared care model. Int J Integr Care. 2018;18(1):4. doi:10.5334/ijic.3046
- Pappano CR, Fung V, Barry M, Zucconi T, Chen J, Irwin K. Developing a population health tool to identify patients with serious mental illness at cancer diagnosis. J Clin Oncol. 2019;37(suppl 31):abstr 82. doi:10.1200/JCO.2019.37.31_suppl.82
- Dharmarajan H, Anderson JL, Kim S, et al. Transition to a virtual multidisciplinary tumor board during the COVID-19 pandemic: University of Pittsburgh experience. Head Neck. 2020;42(6):1310-1316. doi:10.1002/hed.26195
- Happell B, Ewart SB, Bocking J, Platania-Phung C, Stanton R. 'That red flag on your file': misinterpreting physical symptoms as mental illness. J Clin Nurs. 2016;25(19-20):2933-2942. doi:10.1111/jocn.13355
- Gregg J. The Care I Needed. N Engl J Med. 2022;386(5):411-413. doi:10.1056/NEJMp2112526
- Talevski J, Wong Shee A, Rasmussen B, Kemp G, Beauchamp A. Teach-back: A systematic review of implementation and impacts. PLoS One. 2020;15(4):e0231350. Published 2020 Apr 14. doi:10.1371/journal.pone.0231350
- Molloy R, Brand G, Munro I, Pope N. Seeing the complete picture: A systematic review of mental health consumer and health professional experiences of diagnostic overshadowing. J Clin Nurs. Published online December 6, 2021. doi:10.1111/jocn.16151