Metastatic Basal Cell Carcinoma Arising From a Primary Cutaneous Carcinosarcoma
This study presents a case of a man, aged 56 years, found to have a 26-mm exophytic lesion on the vertex scalp identified to contain a distinct population of basal cell carcinoma as well as another population of spindled cells representing a poorly differentiated sarcomatous component.
Introduction
Primary cutaneous carcinosarcoma is a rare biphenotypic tumor with both malignant mesenchymal and epithelial components. Few cases of carcinosarcoma in which the epithelial component consists of basal cell carcinoma (BCC) have been reported to date.1
Fifty-one tumors consisting of cutaneous carcinosarcoma arising from BCC have been described in the literature.1 The authors of one study identified BCC as the most commonly reported epithelial component of cutaneous carcinosarcoma.2 Prognostic factors, including recurrence or metastasis, have been outlined using 94 cases of primary cutaneous carcinosarcomas that were reported between 1972 and 2016. Carcinosarcomas containing a basal cell epithelial component demonstrate a recurrence and metastasis rate of 4.3%. In comparison, the recurrence and metastasis rate of carcinosarcomas derived from other skin tumors, such as squamous cell carcinoma and other adnexal neoplasms, was found to be 38%.2 These data further support the observation that carcinosarcomas that include a BCC component tend to behave less aggressively than those with a squamous or adnexal epithelial component.3 In this report, we present a rare case of metastatic BCC arising from a carcinosarcoma. Our case also highlights the importance of clinicopathologic correlation in the evaluation and management of metastatic cutaneous tumors.
Oncology (Williston Park). 2021;35(12):812-815.
DOI: 10.46883/2021.25920933
Case Description
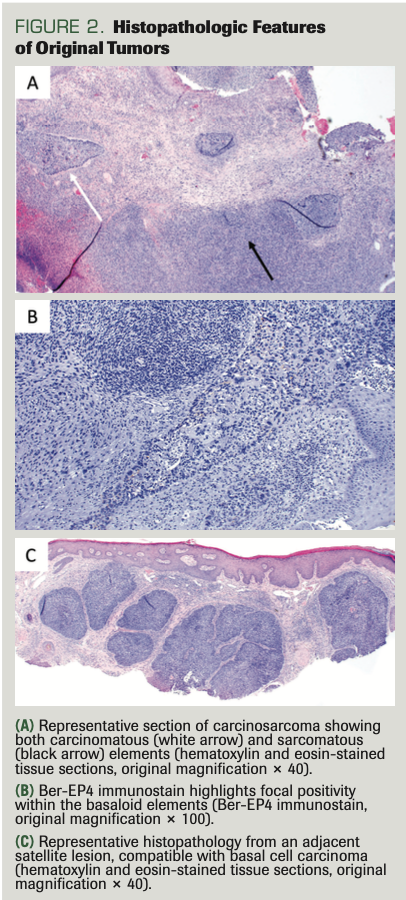
A man, aged 56 years, originally presented to dermatology with a 26-mm erythematous, markedly exophytic tumor on the vertex scalp with 2 adjacent satellite lesions (Figure 1). Biopsies were obtained from both the main and adjacent lesions. Microscopic examination of the main mass revealed a nodular aggregate of peripherally palisaded basaloid cells as well as infiltrating cords set in fibromyxoid stroma with a second population of atypical spindle cells (Figure 2A). These 2 cell populations were intimately intertwined. Immunostains including CD10, CD34, and S100 were negative throughout, speaking against a primary cutaneous sarcoma (including dermatofibrosarcoma protuberans and pleomorphic undifferentiated sarcoma). Ber-EP4, pancytokeratin, and p63 were negative in the spindle cell population, but positive within the basaloid component (Figure 2B). This primary tumor was classified as a carcinosarcoma with features of a spindle cell sarcoma and BCC. The adjacent satellite lesions displayed nests of basaloid keratinocytes with peripheral palisading and retraction artifact, which was compatible with a diagnosis of BCC. At the time, the vertex scalp lesion and adjacent nodules were deemed to represent separate primary tumors (Figure 2C). All lesions were treated by Mohs micrographic surgery. Radiation was offered as adjuvant therapy for the main mass, but the patient declined and was subsequently lost to follow-up.
FIGURE 1. Vertex Scalp at the Time of Original Diagnosis

FIGURE 2. Histopathologic Features of Original Tumors
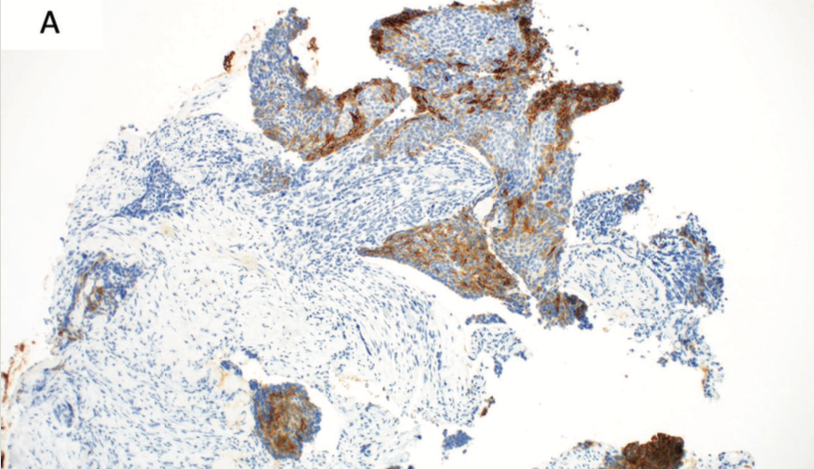
Five years later,the patient developed shortness of breath and cough, and CT imaging revealed a left seventh rib destructive lesion, a right lower lobe cavitating mass, and a few scattered 3-mm pulmonary nodules, concerning for metastases. A bronchoscopy with endobronchial ultrasound and right lower lobe mass fine needle aspiration was performed, and histopathologic examination revealed a basaloid neoplasm displaying expression of pancytokeratin and Ber-EP4 compatible with metastatic BCC (Figure 3A). Next-generation sequencing (NGS) revealed targetable mutations in the PTCH1, PTEN, ARID1A, PDGFRA, and PIK3A genes. The patient’s staging PET scan displayed fluorodeoxyglucose-avid metastatic lesions to the right lower lung, cervical lymph nodes, and skeleton.
FIGURE 3. Histopathologic Features of Subsequent Metastases
(A) Ber-EP4 positivity within the lung mass confirms a diagnosis of metastatic basal cell carcinoma (Ber-EP4 immunostain, original magnification × 100).
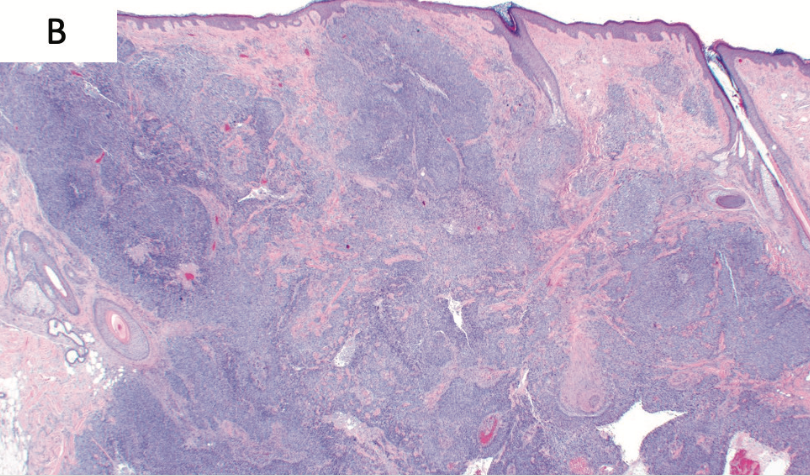
Thorough skin examination revealed a large irregular firm mass in the right supra-auricular areas as well as cervical lymphadenopathy. An incisional biopsy of the scalp lesion was performed and revealed features of nodular BCC (Figure 3B). When compared with the patient’s previously biopsied scalp lesions, this lesion revealed striking similarity in morphology. Notably, this new supra-auricular lesion did not contain a sarcomatous component, and additionally, it displayed a lack of connection to the overlying dermis, which is suggestive of a locoregional metastasis as opposed to de novo BCC.
FIGURE 3. Histopathologic Features of Subsequent Metastases
(B) Representative sections of the supra-auricular scalp mass with diagnostic features of basal cell carcinoma (hematoxylin and eosin-stained tissue sections, original magnification × 40).
After careful review and diligent clinicopathologic correlation, the patient was diagnosed with metastatic BCC arising from a carcinosarcoma in which the carcinomatous component was basal cell. The patient was started on vismodegib 150 mg daily. Six weeks after initiation of therapy, the patient displayed near-complete resolution of the right supra-auricular mass. Six months into treatment, the patient is free of evidence of metastatic disease.
Discussion
Carcinosarcoma is a rare biphenotypic malignant tumor consisting of an epithelial as well as a mesenchymal component. Carcinosarcomas have been reported in numerous organs but primary cutaneous disease is rare. Furthermore, very few cases of cutaneous basal cell carcinosarcoma have been reported to date.4 There are 2 predominant theories for the origin of mixed malignant tumors such as carcinosarcoma: The convergence hypothesis (multiclonal hypothesis) suggests that the neoplasms arise from 2 or more stem cells, while the divergence hypothesis (monoclonal hypothesis) suggests that the neoplasm arises from a single totipotent stem cell that subsequently differentiates into both a mesenchymal component and an epithelial component.4 Some authors have more recently begun to favor the divergence hypothesis. One author reported on a basal cell carcinosarcoma in which both the epithelial and sarcomatous portions underwent DNA sequencing with NGS, and they were found to share multiple mutations, including a mutation in the PTCH1 gene in the hedgehog pathway, which suggests a common origin for the neoplasm.5
Risk factors for the development of epithelial-derived (basal or squamous cell) carcinosarcomas have been identified as advanced age, male gender, and sun-damaged skin of the head and neck. Ultraviolet (UV) light has been suggested as an important causative factor.3 The results of one study suggest that the 5-year disease-free survival rate for patients with these tumors of 70%. Additionally, it has been shown that the prognosis is not affected by the type or the ratio of sarcomatous component.2 Results of another study showed that age less than 65 years, recent growth, longstanding skin tumor, and tumor size greater than 2 cm is correlated with more aggressive disease.4 These findings are pertinent to our patient, as he fits many of these categories and has had metastatic recurrence of disease 5 years after original resection.
There is little evidence for effective treatment modalities for these rare malignancies. Vismodegib, a hedgehog pathway inhibitor (HHI), has been approved for treatment of metastatic BCC as well as locally advanced BCC.5 Cemiplimab (Libtayo), an anti–PD-1 antibody, has recently been approved for treatment of locally advanced and metastatic BCC in patients either previously treated with an HHI or in patients in whom an HHI is not appropriate.6 Very careful clinicopathologic correlation was necessary in accurately classifying this patient’s metastatic neoplasm, because choice of treatment modality is dependent on histogenesis. This patient’s pulmonary metastasis was basaloid and displayed strong positivity for Ber-EP4, which is compatible with metastatic BCC. Furthermore, NGS of the metastasis revealed a high tumor mutational burden, which is often seen in UV–mediated carcinogenesis. Sequencing also highlighted a PTCH1 mutation, confirming that targeted therapy with an HHI would likely be effective. The patient was started on vismodegib and scheduled for a follow-up 6 weeks later, at which time the right supra-auricular mass was nearly resolved. Subsequent PET-CT imaging showed resolution of the lung mass but persistence of the rib lesions; for these, he was provided radiation therapy.
This case highlights an exceptional occurrence in which basal cell carcinosarcoma developed locoregional then distant metastasis and had an excellent response to hedgehog pathway inhibition.
CONFLICT OF INTEREST: None reported
FUNDING: None.
References
1. Davis K, Whale K, Tran S, Hamilton S, Kandamany N. A rare case of cutaneous basal cell carcinosarcoma in an immunosuppressed patient. Pathology. 2020;52(2):267-268. doi:10.1016/j.pathol.2019.10.011
2. Suzuki H, Hashimoto A, Saito R, Izumi M, Aiba S. A case of primary cutaneous basal cell carcinosarcoma. Case Rep Dermatol. 2018;10(2):208-215. doi:10.1159/000492525
3. Rose RF, Merchant W, Stables GI, Lyon CL, Platt A. Basal cell carcinoma with a sarcomatous component (carcinosarcoma): a series of 5 cases and a review of the literature. J Am Acad Dermatol. 2008;59(4):627-632. doi:10.1016/j.jaad.2008.05.035
4. Tran TA, Muller S, Chaudahri PJ, Carlson JA. Cutaneous carcinosarcoma: adnexal vs. epidermal types define high- and low-risk tumors. results of a meta-analysis. J Cutan Pathol. 2005;32(1):2-11. doi:10.1111/j.0303-6987.2005.00260.x
5. Meiss F, Andrlová H, Zeiser R. Vismodegib. Recent Results Cancer Res. 2018;211:125-139. doi:10.1007/978-3-319-91442-8_9
6. Stratigos AJ, Sekulic A, Peris K, et al. Cemiplimab in locally advanced basal cell carcinoma after hedgehog inhibitor therapy: an open-label, multi-centre, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6):848-857. doi:10.1016/S1470-2045(21)00126-1