Perspectives on Follicular Lymphoma Treatment From New and Experienced Clinicians: New, Old, & Old Is New
Jonathan R. Day, MD, PharmD, and Brian K. Link, MD, give their perspective on emerging treatments for follicular lymphoma.
The accompanying article is an excellent overview of a field perceived to be evolving quickly, but how quick is that evolution in reality?
Perspective of Experienced Clinician (BKL)
Providing peer review and perspective on the accompanying article, which nicely summarizes the biology and management of follicular lymphoma (FL), was a pleasure. The joy was derived from the high quality of the writing and from sharing this assignment with a senior internal medicine resident recently dedicated to the study of a field I have pondered for more than 30 years. The fresh perspective on many of the topics sparked an interesting dialogue on new vs old and rapid vs indolent.
Perspective of a New Clinician (JRD)
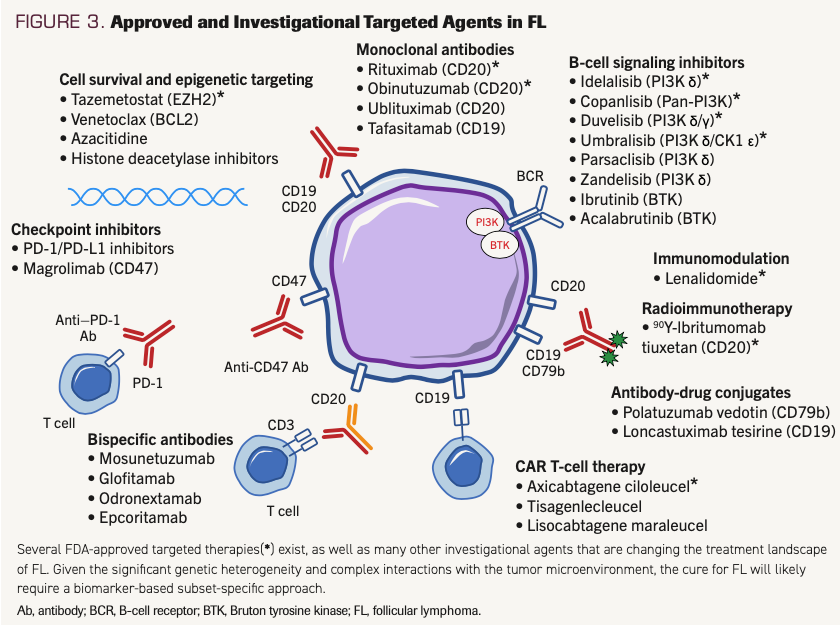
The accompanying article highlights many reasons for new clinicians to be excited about entering the field of hematology and oncology. New clinicians see a landscape with abundant options for patients and can be optimistic for improvements in FL treatment. These new options move beyond standard anti-CD20 antibodies plus cytotoxic chemotherapeutics to new and varied mechanisms of action and novel therapeutics. A fascinating, multifaceted array of options and mechanisms is depicted in the article’s Figure 3, highlighting targeted inhibition of biologic pathways and complex approaches to harnessing the immune system.
FIGURE 3. Approved and Investigational Targeted Agents in FL (originally appears in Cahill et al. ONCOLOGY (Williston Park). 2021.)
Although new options are arriving in the clinic at a rapid pace, the story of improving therapy for FL is, summarily, persistence.
Targeting Pathways
Efforts to find selective molecular pathway targets to subdue aberrant cellular activity in cancer has long been a goal in cancer pharmacology. One pathway that regulates multiple hallmarks of malignancy is the mTOR–AKT–PI3K pathway. Efforts focused on mTOR inhibition in lymphoma date back to the early 2000s, but clinical trial results were less robust than hoped for.1-6 Therefore, efforts shifted elsewhere in the pathway. For example, Bruton tyrosine kinase (BTK) is activated by PI3K, and BTK inhibition has achieved great results in chronic lymphocytic leukemia (CLL). Its role in FL, however, remains to be established—although it also remains under investigation.7-11
The persistent efforts to interrupt this pathway seem to be finally paying off. As noted in the accompanying article, 4 of 7 new agents recently approved for FL are PI3K inhibitors. Other mechanistic approaches like BCL-2 inhibitors failed to have the initially expected impact, and perhaps more persistence is needed to understand how BCL-2 inhibition should be utilized.12
Harnessing the Immune System
Novel methods to fight cancer, including harnessing the immune system, are exciting, but this concept is hardly new. Some of the newest treatments can trace their beginnings to more than 30 years ago. Initial efforts to manipulate the immune system were less elegant than they are today, utilizing systemic interferon and interleukin.13-16 The 1984 Nobel Prize was awarded for technology used to create monoclonal antibodies; this opened a Pandora’s box that was widely expected to quickly revolutionize the treatment of lymphoma. Early breakthroughs with anti-CD20 monoclonal antibodies provided to have meaningful benefit for patients before the century turned, but efforts at targeting other antigens (those that come to mind were against CD19, CD22, and CD80) were not immediately fruitful.17,18 Immunoconjugates with biotoxins and radioisotopes were variably active but did not meaningfully change the treatment landscape. Even the vision of bispecific antibodies to retarget autologous T cells was clear from preclinical models in the early 1990s, but challenges with protein chemistry stunted clinical development.19
Other immune-mediated strategies, such as tumor vaccines, were first trialed in the 1990s.20 Large phase 3 trials in the 2000s had conflicting results, which led to an ongoing pause in momentum for vaccination strategies.21-23 Immunomodulation with lenalidomide (Revlimid) was undergoing testing in hematologic malignancies by 2002, and it gained approval for multiple myeloma and myelodysplastic syndrome by 2006, but its utility in FL wasn’t fully realized until recent combinations with antibodies targeting CD20 and perhaps CD19.24,25
Early efforts to capitalize on recent exciting techniques for immunologic checkpoint inhibition have been underwhelming in FL, but as highlighted in the featured article, ongoing studies with antibody combinations may unlock the hoped-for potential.26,27 These examples illustrate the blurred lines between new and old. Other new therapies for FL, such as chimeric antigen receptor T cells, are inspiring examples of the efficiency seen from combining the newest technologies with the newest biology. Nonetheless, persistence and an open mind to reevaluation of previously “failed” ideas will no doubt result in more immunotherapy options in the future. In contrast with a relatively spartan treatment landscape a generation ago, we are now looking at a plethora of emerging therapies to treat patients. The next generational challenge will be establishing sequences and combinations optimal for long-term management of this disease, which so far remains incurable. A significant challenge for clinical researchers is how to measure improvement. The use of overall survival (OS) as a primary end point is challenging in FL due to the infrequency of early deaths. Patients with early progression of disease after immunochemotherapy has been identified as a population with unmet need; however, this group is heterogenous and relatively small. How to best individualize these therapies for patients will be a challenge. Perhaps a reevaluation of end points is in order. OS and even progression-free survival do not measure the complete impact of FL on patients. How do we incorporate acute and chronic toxicities, quality of life, and cost factors? Should we target cure as goal and if so, how do we define cure in FL?
The persistence of previous generations of researchers with biological discoveries has resulted in more therapeutic options to work with. The next generation will undoubtedly persist in redefining loftier measures of success for patients and incorporating new options to achieve those measures.
AUTHOR AFFILIATIONS:
Jonathan R. Day, MD, PharmD;1 and Brian K. Link, MD1
1Department of Internal Medicine, University of Iowa, Iowa City, Iowa
References
1. Jundt F, Raetzel N, Müller C, et al. A rapamycin derivative (everolimus) controls proliferation through down-regulation of truncated CCAAT enhancer binding protein {beta} and NF-{kappa}B activity in Hodgkin and anaplastic large cell lymphomas. Blood. 2005;106(5):1801-1807. doi:10.1182/blood-2004-11-4513
2. Witzig TE, Geyer SM, Ghobrial I, et al. Phase II trial of single-agent temsirolimus (CCI-779) for relapsed mantle cell lymphoma. J Clin Oncol. 2005;23(23):5347-5356. doi:10.1200/JCO.2005.13.466
3. Wanner K, Hipp S, Oelsner M, et al. Mammalian target of rapamycin inhibition induces cell cycle arrest in diffuse large B cell lymphoma (DLBCL) cells and sensitises DLBCL cells to rituximab. Br J Haematol. 2006;134(5):475-484. doi:10.1111/j.1365-2141.2006.06210.x
4. Yee KW, Zeng Z, Konopleva M, et al. Phase I/II study of the mammalian target of rapamycin inhibitor everolimus (RAD001) in patients with relapsed or refractory hematologic malignancies. Clin Cancer Res. 2006;12(17):5165-5173. doi:10.1158/1078-0432.CCR-06-0764
5. Witzig TE, Reeder CB, LaPlant BR, et al. A phase II trial of the oral mTOR inhibitor everolimus in relapsed aggressive lymphoma. Leukemia. 2011;25(2):341-347. doi:10.1038/leu.2010.226
6. Smith SM, van Besien K, Karrison T, et al. Temsirolimus has activity in non-mantle cell non-Hodgkin’s lymphoma subtypes: The University of Chicago phase II consortium. J Clin Oncol. 2010;28(31):4740-4746. doi:10.1200/JCO.2010.29.2813
7. Woyach JA, Ruppert AS, Heerema NA, et al. Ibrutinib regimens versus chemoimmunotherapy in older patients with untreated CLL. N Engl J Med. 2018;379(26):2517-2528. doi:10.1056/NEJMoa1812836
8. Maddocks K, Christian B, Jaglowski S, et al. A phase 1/1b study of rituximab, bendamustine, and ibrutinib in patients with untreated and relapsed/refractory non-Hodgkin lymphoma. Blood. 2015;125(2):242-248. doi:10.1182/blood-2014-08-597914
9. Fowler NH, Advani RH, Sharman J, et al. The Bruton's tyrosine kinase inhibitor ibrutinib (PCI-32765) is active and tolerated in relapsed follicular lymphoma. 2012;120(21):156. doi:10.1182/blood.V120.21.156.156
10. Fowler N, Boyd TE, Sharman JP, et al. Long-term follow-up and analysis of dose groups with ibrutinib in relapsed follicular lymphoma. Blood. 2015;126(23):2706. doi:10.1182/blood.V126.23.2706.2706
11. Gopal AK, Schuster SJ, Fowler NH, et al. Ibrutinib as treatment for patients with relapsed/refractory follicular lymphoma: results from the open-label, multicenter, phase II DAWN study. J Clin Oncol. 2018;36(23):2405-2412. doi:10.1200/JCO.2017.76.8853
12. Zinzani PL, Flinn IW, Yuen SLS, et al. Venetoclax-rituximab with or without bendamustine vs bendamustine-rituximab in relapsed/refractory follicular lymphoma. Blood. 2020;136(23):2628-2637. doi:10.1182/blood.2020005588
13. Chisesi T, Capnist G, Vespignani M, Cetto G. Interferon alfa-2b and chlorambucil in the treatment of non-Hodgkin’s lymphoma. Invest New Drugs. 1987;5 Suppl:S35-S40. doi:10.1007/BF00207261
14. Chisesi T, Congiu M, Contu A, et al. Randomized study of chlorambucil (CB) compared to interferon (alfa-2b) combined with CB in low-grade non-Hodgkin’s lymphoma: an interim report of a randomized study. Non-Hodgkin’s Lymphoma Cooperative Study Group. Eur J Cancer. 1991;27(Suppl 4):S31-S33. doi:10.1016/0277-5379(91)90566-v
15. Ozer H, Anderson JR, Peterson BA, et al. Combination trial of subcutaneous interferon alfa-2b and oral cyclophosphamide in favorable histology, non-Hodgkin’s lymphoma. Invest New Drugs. 1987;5 suppl:S27-S33. doi:10.1007/BF00207260
16. Weber JS, Yang JC, Topalian SL, Schwartzentruber DJ, White DE, Rosenberg SA. The use of interleukin-2 and lymphokine-activated killer cells for the treatment of patients with non-Hodgkin’s lymphoma. J Clin Oncol. 1992;10(1):33-40. doi:10.1200/JCO.1992.10.1.33
17. May RD, Vitetta ES, Moldenhauer G, Dorken B. Selective killing of normal and neoplastic human B cells with anti-CD19- and anti-CD22-ricin A chain immunotoxins. Cancer Drug Deliv. 1986;3(4):261-272. doi:10.1089/cdd.1986.3.261
18. Vitetta ES, Stone M, Amlot P, et al. Phase I immunotoxin trial in patients with B-cell lymphoma. Cancer Res. 1991;51(15):4052-4058.
19. Link BK, Weiner GJ. Production and characterization of a bispecific IgG capable of inducing T-cell-mediated lysis of malignant B cells. Blood. 1993;81(12):3343-3349.
20. Hsu FJ, Caspar CB, Czerwinski D, et al. Tumor-specific idiotype vaccines in the treatment of patients with B-cell lymphoma--long-term results of a clinical trial. Blood. 1997;89(9):3129-3135.
21. Freedman A, Neelapu SS, Nichols C, et al. Placebo-controlled phase III trial of patient-specific immunotherapy with mitumprotimut-T and granulocyte-macrophage colony-stimulating factor after rituximab in patients with follicular lymphoma. J Clin Oncol. 2009;27(18):3036-3043. doi:10.1200/JCO.2008.19.8903
22. Levy R, Robertson M, Ganjoo K, Leonard J, Vose J, Denney D. Results of a phase 3 trial evaluating safety and efficacy of specific immunotherapy, recombinant idiotype (Id) conjugated to KLH (Id-KLH) with GM-CSF, compared to non-specific immunotherapy, KLH with GM-CSF, in patients with follicular non-Hodgkin’s lymphoma (fNHL). Cancer Res. 2008;68(suppl 9):abstr LB-204.
23. Schuster SJ, Neelapu SS, Gause BL, et al. Vaccination with patient-specific tumor-derived antigen in first remission improves disease-free survival in follicular lymphoma. J Clin Oncol. 2011;29(20):2787-2794. doi:10.1200/JCO.2010.33.3005
24. Leonard JP, Trneny M, Izutsu K, et al; AUGMENT Trial Investigators. AUGMENT: a phase III study of lenalidomide plus rituximab versus placebo plus rituximab in relapsed or refractory indolent lymphoma. J Clin Oncol. 2019;37(14):1188-1199. doi:10.1200/JCO.19.00010
25. Wiernik PH, Lossos IS, Tuscano JM, et al. Lenalidomide monotherapy in relapsed or refractory aggressive non-Hodgkin’s lymphoma. J Clin Oncol. 2008;26(30):4952-4957. doi:10.1200/JCO.2007.15.3429
26. Armand P, Janssens A, Gritti G, et al. Efficacy and safety results from CheckMate 140, a phase 2 study of nivolumab for relapsed/refractory follicular lymphoma. Blood. 2021;137(5):637-645. doi:10.1182/blood.2019004753
27. Nastoupil LJ, Westin JR, Fowler NH, et al. Response rates with pembrolizumab in combination with rituximab in patients with relapsed follicular lymphoma: interim results of an on open-label, phase II study. J Clin Oncol. 2017;35(suppl 15):abstr 7519. doi:10.1200/JCO.2017.35.15_suppl.7519
Highlighting Insights From the Marginal Zone Lymphoma Workshop
Clinicians outline the significance of the MZL Workshop, where a gathering of international experts in the field discussed updates in the disease state.