Use of Neoadjuvant Chemotherapy in Elderly Patients With Muscle-Invasive Bladder Cancer: A Population-Based Study, 2006-2017
Patients 70 years or older that received neoadjuvant chemotherapy and radical cystectomy had better overall survival than those undergoing radical cystectomy alone.
Objectives/Introduction
Bladder cancer is a disease of the elderly (median age at diagnosis, 73 years).1 Current guidelines recommend that patients with muscle-invasive bladder cancer (MIBC) be given neoadjuvant chemotherapy (NAC) prior to radical cystectomy (RC).2 NAC has been shown to increase median overall survival from 46 months to 77 months3 and to confer a 5% improvement in overall survival (OS).4 Improvement in OS is seen in both younger and older patients. In the landmark randomized controlled trial by Grossman et al, median OS in patients 65 years or older receiving NAC was 61 months compared with 30 months in those undergoing cystectomy alone.3 Subsequently, several single-institution studies have shown that elderly patients receiving NAC have similar OS and pathologic response as younger patients.5,6
Despite strong evidence for the benefit of NAC in patients with MIBC, it remains underutilized. A recent Surveillance, Epidemiology and End Results (SEER) – Medicare study found that only 12.6% of patients treated with RC between 2001 and 2011 received NAC. Use of NAC was even lower with increasing age, with only 11.4% of patients aged 75 to 79 years and 7.0% of those 80 years or older receiving NAC.7 Reasons for lower NAC use in the elderly population include comorbidities and age-related renal dysfunction.8 Nevertheless, some older patients are not offered NAC due to perceived lack of physiologic reserve and concerns regarding postoperative complications after receipt of chemotherapy. RC may be associated with worse complication rates and perioperative mortality in older patients,9,10 but the effect of NAC on surgical outcomes in appropriately selected elderly patients has not been studied. Our objective was to evaluate real-world age-based disparity in treatment and outcomes of patients with MIBC undergoing RC.
Oncology (Williston Park). 2022;36(1):21-33.
DOI: 10.46883/2022.25920939
Methods
Data were extracted from the National Cancer Database (NCDB), the largest cancer registry in the world, collecting data from more than 1500 Commission on Cancer (CoC)–accredited facilities. Approximately 30% of United States hospitals have CoC accreditation and as such, the NCDB provides an excellent resource to study real-world population-based trends and outcomes.11 Patients diagnosed with MIBC from 2006 to 2017 were identified. This time frame was chosen to allow time for infiltration into clinical practice of the key Grossman et al study, published in 2003.3 Furthermore, sequencing of systemic treatment and surgical procedures was added as a data point to the NCDB in 2006, allowing for identification of the neoadjuvant nature of administered chemotherapy.
Cohorts
Two study cohorts were formed for analysis of (1) the use of various treatment modalities among elderly compared with younger patients and (2) the effect of NAC on perioperative outcomes in elderly patients undergoing RC.
FIGURE 1. Study Inclusion Diagram
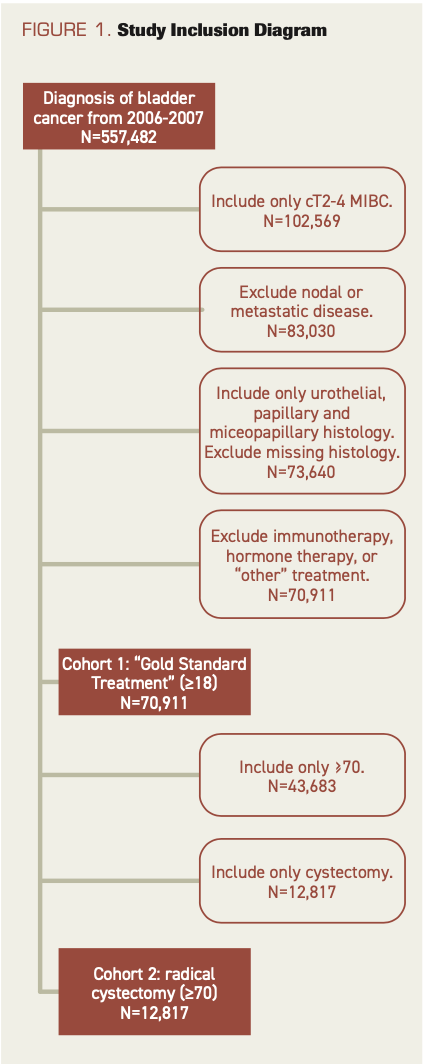
The first cohort consisted of all patients 18 years or older with microscopically confirmed clinical stage T2 to T4 MIBC. Only patients with urothelial, papillary, or micropapillary disease were included. Patients were excluded if they had nodal or metastatic disease or missing histology, or if they had undergone immunotherapy, hormone therapy, or “other” treatment (Figure 1). Patients were stratified into 2 groups based on age: under 70 or 70 years and older. Use of different treatments, including RC alone; RC and adjuvant chemotherapy (AC); chemotherapy and radiation therapy; “gold-standard treatment” (GST), defined as NAC and RC; and no or missing treatment was compared between age groups. The second cohort included only elderly patients, defined as 70 years or older, who underwent RC. Patients were stratified based on receipt of RC alone (no NAC) vs NAC and RC. Of note, the no-NAC cohort included patients receiving AC.
Analysis
Each cohort was weighted for analysis using propensity scores calculated using logistic regression for the following demographic and treatment specific variables: age (second cohort only), sex, race, area of residence, insurance, year of diagnosis, median income, high school graduation status, treatment facility type, distance to treatment facility, histology, clinical T stage, Charlson Comorbidity Index (CCI) score, pelvic lymph node dissection (PLND), and surgery type (minimally invasive vs open). Weights were estimated by transforming the calculated propensity scores via inverse probability. Chi-square comparisons were analyzed for all variables of interest pre- and post weight application. Estimated weights were included for all regression and survival analyses across both cohorts.12 Propensity score weighting (PSW) resulted in narrowing of both cohorts to diagnosis years 2010 to 2017 due to missing data for variables used in score calculation or lack of patient characteristic matching.
For the first cohort, differences in the proportion of preweighted age groups who received GST during the study timeframe were assessed by t test. Weighted univariate and multivariate logistic regression was performed to determine predictors of receiving GST. For the second cohort, primary outcomes included length of stay (LOS), readmission within 30 days, and 30- and 90- day mortality. Weighted univariate and multivariate regressions were constructed. Secondary outcomes included OS through weighted Cox proportional hazard analysis. OS was defined by time to “date of last contact or death” and overall mortality status (NCDB “vital status”). OS was first analyzed in the entire cohort from 2010 to 2016 (no mortality data were available for 2017). Utilization of NAC increased over the study period, which resulted in proportional hazards assumption violations. To account for this, OS analysis was separated based on year of diagnosis (2010-2013 and 2014-2016). Kaplan-Meier curves were constructed for the overall cohort and the separate time periods.
Covariates assessed in the weighted regressions included all variables used for PSW as well as receipt of NAC (second cohort only). Assumptions and violations of confounding were checked for all models. Statistical analysis was conducted using R (R Core Team) and Excel for Office 365 MSO (Microsoft).
Results
GST by Age Group (cohort 1)
Pre–propensity weighted analysis
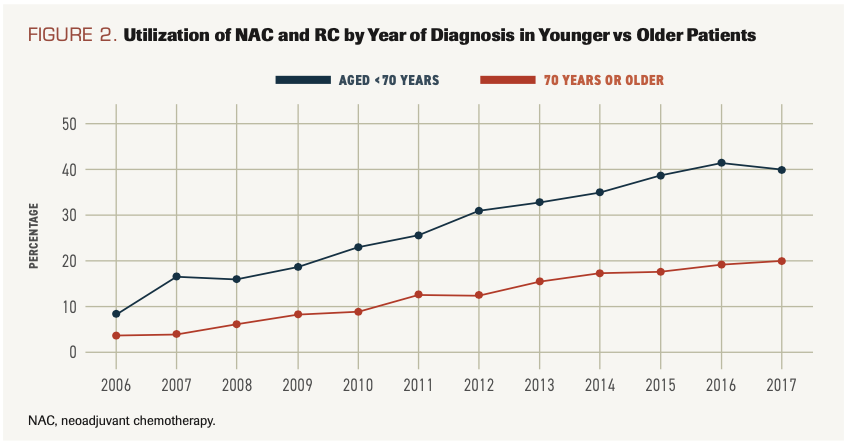
A total of 557,482 patients with bladder cancer diagnosed between 2006 and 2017 were identified. The cohort for the first analysis was composed of 70,911 patients with nonmetastatic MIBC; younger patients (under 70 years) accounted for 38.4% (n = 27,228) and older patients (70 years or older) for 61.6% (n = 43,683). Compared with older patients, younger patients were more likely to be male, to be Black, to live further from their treatment facility, and to be treated at an academic center. Older patients were more likely to have Medicare or Medicaid, high school completion, higher median income, and higher CCI score. PLND was less often performed in patients 70 years or older (30.4% vs 55.8%; P < .001), while robotic cystectomy was more common in these patients (45.4% vs 39.4%; P < .001) (Supplementary Table 1). Utilization of NAC and RC increased in recent years in younger and older patients but at a significantly slower rate in those 70 years or older. In 2017, 40.3% of all patients with MIBC who were aged under 70 years received NAC and RC compared with just 20.5% of those 70 years or older (P < .001) (Figure 2).
FIGURE 2. Utilization of NAC and RC by Year of Diagnosis in Younger vs Older Patients
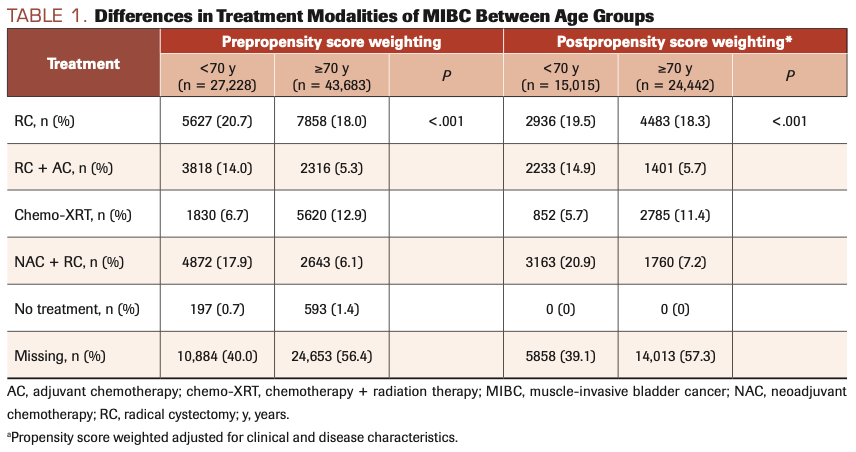
Postpropensity weighted analysis
Older patients were less likely to undergo GST. Only 7.2% of patients 70 years or older underwent NAC and RC compared with 20.9% of patients aged under 70 years. RC and AC were less common in the older cohort (5.7% vs 14.9%) while chemoradiation was more common in the older cohort (11.4% vs 5.7%; P <.001) (Table 1). On multivariate analysis, age remained a predictor of receiving GST (odds ratio [OR], 0.52; 95% CI, 0.49-0.56; P <.001). PLND at time of RC was also associated with receipt of NAC (OR, 6.67; 95% CI, 5.90-7.56; P < .001). Additional predictors of GST were private insurance, treatment at an academic center or integrated network cancer program, high school completion, lower CCI score, higher clinical T stage, and surgery in recent years (Supplementary Table 2).
TABLE 1. Differences in Treatment Modalities of MIBC Between Age Groups
Patients 70 Years or Older Undergoing RC With or Without NAC (cohort 2)
Preweighted analysis
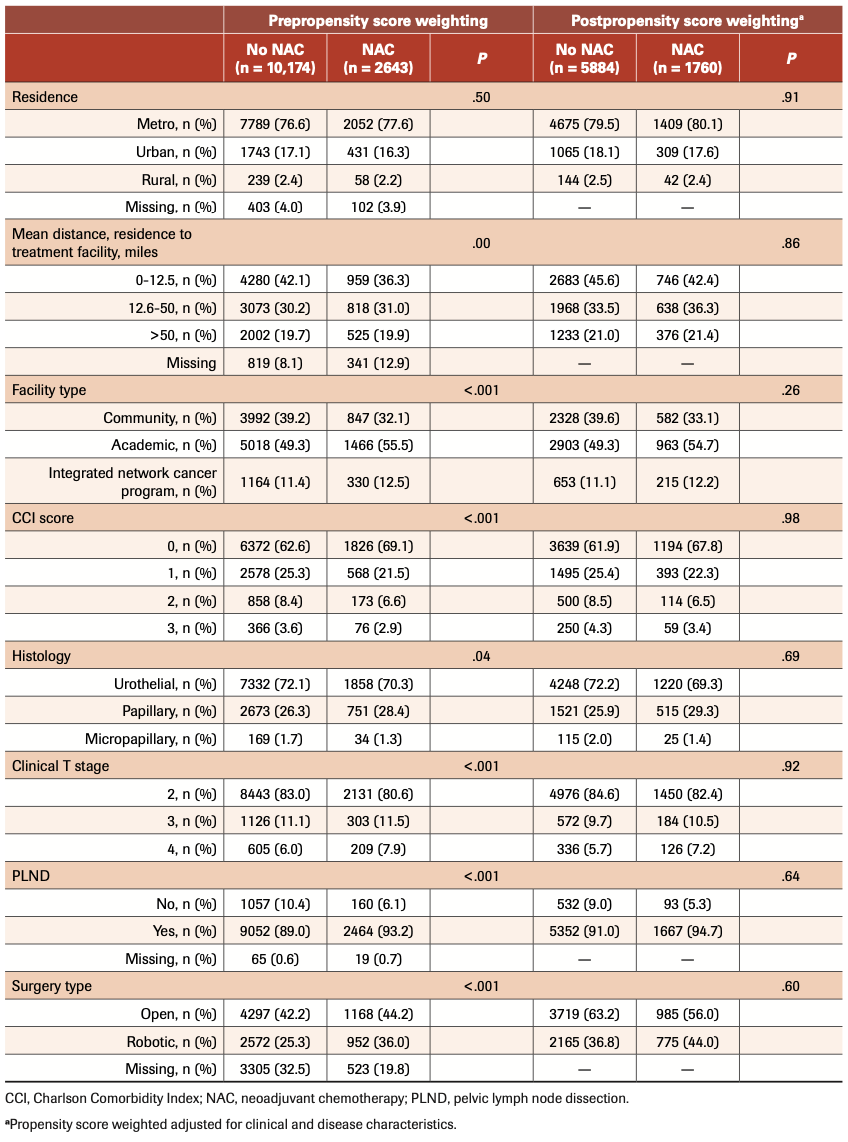
Subsequent analysis was focused on patients 70 years or older who underwent RC (n = 12,817). Of these patients, only 2643 (20.6%) received NAC. Patients receiving NAC were more likely to be aged 70 to 80 years (86.5% vs 68.7%; P <.001). NAC was associated with higher median income and high school completion rate, CCI score of 0, higher clinical T stage, and treatment at an academic center or integrated network cancer program. Furthermore, PLND and robotic surgery were more common in the NAC cohort (93.2% vs 89.0%; P <.001; and 36.0% vs 25.3%; P <.001, respectively). (Table 2)
TABLE 2. Demographics and Pathology Data of Cohort ≥70 Years Undergoing Radical Cystectomy
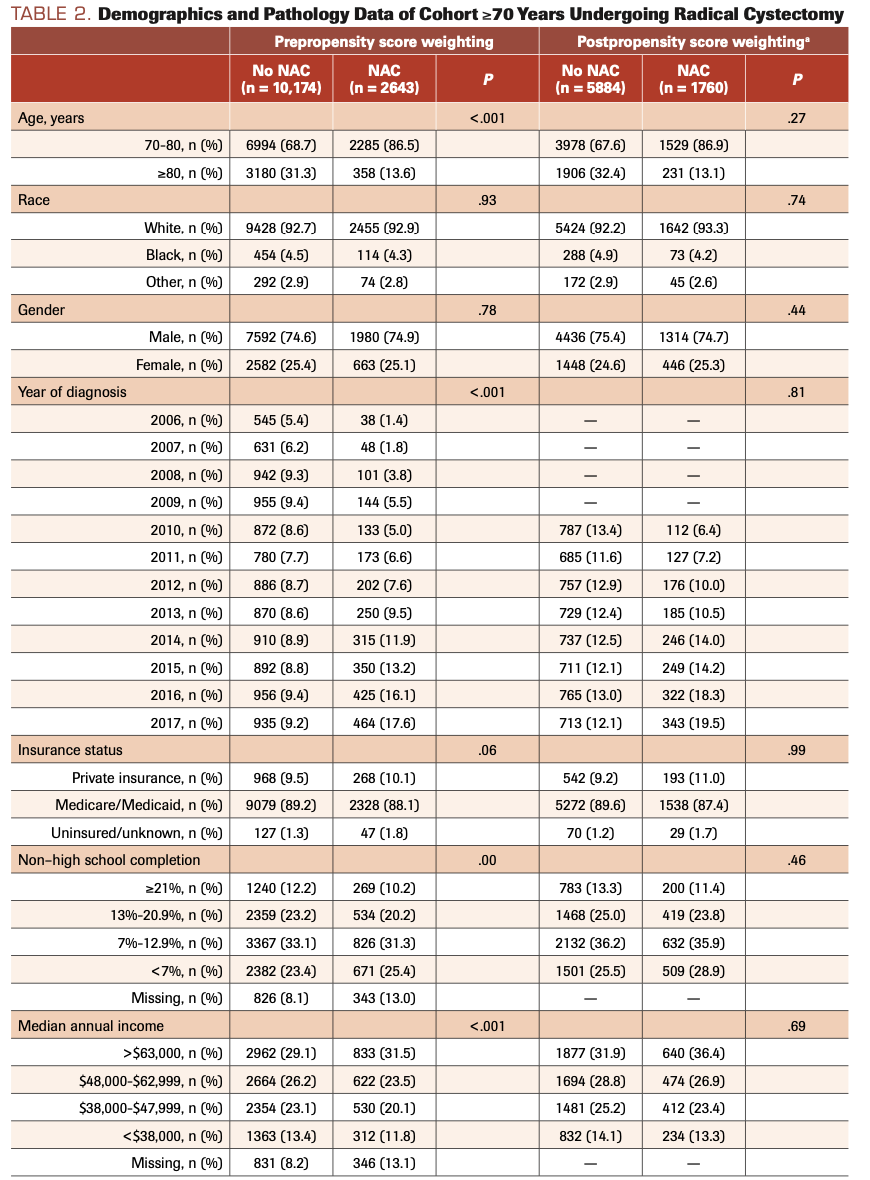
TABLE 2. Demographics and Pathology Data of Cohort ≥70 Years Undergoing Radical Cystectomy
Postweighted analysis
Patients receiving NAC had shorter LOS (8.5 days vs 9.6 days; P < .001) and were less likely to be readmitted within 30 days (8.6% vs 10.6%; P < .001). They also had lower 30- and 90-day mortality (1.5% vs 3.1%; P = .01; and 4.9% vs 7.7%; P = .003, respectively). OS was improved with NAC (43.7% vs 37.5%; P < .001) (Table 3).
TABLE 3. Perioperative and Mortality Outcomes in Patients ≥70 Years Based on Use of Neoadjuvant Chemotherapy Before and After Adjustment by Propensity Score Weighting
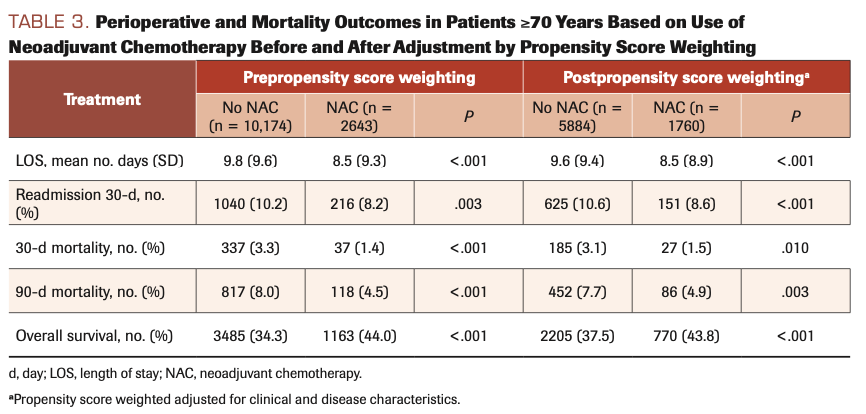
When controlling for all other variables, NAC was a predictor of slightly lower LOS (β, –0.66 days; 95% CI, –1.08 to –0.24; P = .002), as well as lower 30- and 90-day mortality (OR, 0.62; 95% CI, 0.46-0.83; P = .002; and OR, 0.72; 95% CI, 0.60-0.87; P < .001, respectively). NAC was not associated with readmission rate. Notably, compared with the patients aged 70 to 80 years, patients ≥80 years had longer LOS (β, 0.77; 95% CI, 0.30-1.23; P = .001), higher 30-day readmission rate (OR, 1.20; 95% CI, 1.01-1.41; P = .032), and higher 30- and 90-day mortality (OR, 2.39; 95% CI, 1.78-3.21; P < .001; and OR, 1.76; 95% CI, 1.45-2.13; P < .001, respectively) (Supplementary Tables 3-5).
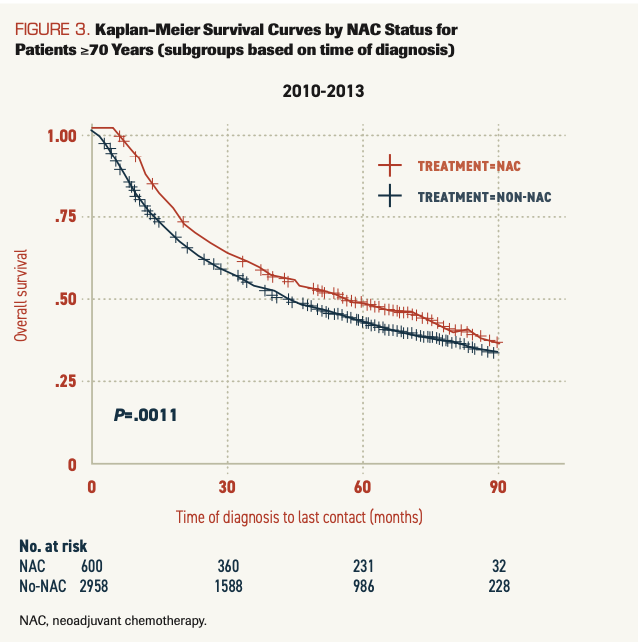
Five-year OS was 49.4% for the NAC group vs 40.2% in the no-NAC group. Upon multivariate OS analysis, in patients treated between 2010 and 2013, NAC was not independently associated with OS; for those treated between 2014 and 2016, NAC was a predictor of improved OS (HR, 0.75; 95% CI, 0.65-0.86; P < .001) (Supplementary Table 6). Kaplan-Meier curves were constructed for the entire cohort, 2010 to 2016; patients receiving NAC had improved OS (P < .0001) (Supplementary Figure). However, the increased utilization of NAC over time resulted in a proportional hazards violation. Separate Kaplan-Meier analyses performed for 2010 to 2013 and 2014 to 2016 confirmed improved OS with NAC compared with RC alone in both time periods (P = .0011 and P < .001, respectively) (Figure 3).
FIGURE 3. Kaplan-Meier Survival Curves by NAC Status for Patients ≥70 Years (subgroups based on time of diagnosis)
Discussion
As the US population ages, with the number of Americans 65 years and older expected to double in the next 40 years,13 it is critical to understand treatment patterns and outcomes in the elderly. In this large population-based analysis using PSW to decrease selection bias, we found that patients 70 years or older are half as likely to receive GST with NAC and RC. Despite this, we found that older patients treated with NAC and RC had shorter LOS, lower 30-day readmission rates, and decreased perioperative mortality compared with those undergoing surgery alone. Older patients receiving NAC also had improved OS. Our results suggest that in properly selected elderly patients, NAC does not result in increased surgical morbidity and that advanced age should not preclude offering NAC prior to RC.
Underutilization of curative therapy in elderly patients is well documented. A prior NCDB study showed that the likelihood of receiving aggressive therapy (defined as radical or partial cystectomy or chemoradiotherapy) declined with increased patient age, with an OR of 0.68 for those aged 71 to 80 years and of 0.34 for those aged 81 to 90 years.14 A population-based United Kingdom cancer registry showed that in patients with MIBC, RC or radical radiotherapy was used in 50% of patients aged under 69 years but in only 34% aged 70 to 79 years and 12% of those 80 years or older.15 Similar results have also been demonstrated using the SEER database.16-18 This is consistent with our analysis showing that 61.0% of patients aged under 70 years received definitive treatment compared with 42.7% of those 70 years or older (P < .001). The decision to forgo aggressive treatment in elderly patients with MIBC may be a result of weighing risk of cancer-specific mortality (CSM) vs other-cause mortality (OCM). SEER data have shown that although both CSM and OCM are higher in older patients, CSM is the leading cause of mortality regardless of age or pathological subgroup.19 This suggests that definitive treatment is justified in a subset of older patients.
American Urological Association (AUA) and National Comprehensive Cancer Network (NCCN) guidelines define GST as NAC and RC2,20; however, this is often underutilized. We found that only 7.2% of patients 70 years or older received GST compared with 20.9% of those aged under 70 years. A number of demographic factors were predictive of GST, including high school completion, insurance status, and income. Whether these findings are a result of physician bias or differences in patients’ decision-making is unknown. Patients treated at an academic center or integrated network cancer program received GST more often, which may point to higher rates of guideline adherence within these practice types. Guidelines also recommend PLND at the time of RC. We found that PLND was less commonly performed in patients 70 years or older (30.4% vs 55.8%; P < .001). Patients receiving PLND were also more likely to receive NAC, potentially indicating that adherence to one guideline is associated with adherence to others. In a recent study, Abdollah et al found that PLND was omitted more often in patients aged over 80 years and that omitting PLND resulted in a 1.2-fold greater mortality in this age group.21 Given that AUA and NCCN guidelines are based on extensive data showing improved overall survival with NAC and PLND, these recommendations should be considered in patients of all ages.
Concerns regarding perioperative outcomes may dissuade surgeons from offering RC to elderly patients. A recent systematic review found that perioperative mortality increased with age, with reported incidence of 1% to 6% for patients aged under 70 years vs 0% to 15% for patients 70 years or older.9 However, several studies have shown no difference in surgical complications between older and younger patients.22-27 Additionally, a recent analysis of the National Surgery Quality Improvement Program database found that incidence of cardiac, pulmonary, and thromboembolic complications after RC were comparable in septuagenarians and octogenarians, suggesting that even well-selected “very old” patients may be offered cystectomy.28 Furthermore, cancer-specific survival and OS are higher in octogenarians undergoing RC compared with transurethral resection of bladder tumor or radiotherapy.29 The introduction of Enhanced Recovery after Surgery protocols may further decrease morbidity for elderly surgical patients.30 As the majority of evidence on RC in elderly patients is from retrospective studies, surgical selection bias undoubtedly plays a role, with less comorbid patients being more likely to be offered surgery. This healthier, surgically selected subgroup of elderly patients may also be better able to withstand the negative effects of chemotherapy; thus, they should be considered for NAC prior to RC.
Data on use of NAC in elderly patients are lacking. Grossman et al found that in the cohort of patients 65 years or older, NAC and RC resulted in an OS of 61 months vs 30 months for RC alone; however, only 135 patients were in this subgroup.3 In a retrospective study of 83 patients with MIBC undergoing RC or definitive radiotherapy, Chau et al found that patients 70 years or older had OS, relapse-free survival, and response rates that were similar to those of patients aged under 70 years. Patients 70 years or older were just as likely to proceed with definitive local treatment: 87.9% vs 84.0% of those aged
under 70 years.5 Leone et al reported similar findings, with no difference in oncologic outcomes in younger vs older patients undergoing NAC prior to RC. Rates of nephrotoxicity, bone marrow suppression, and thromboembolic events were similar. Older patients did not require dose reduction more often than younger patients.6
Disparity in treatment of elderly patients with MIBC can be partially attributed to the increase in comorbidities and frailty seen in advanced age. Certainly, not all elderly patients are candidates for NAC and RC, and it is well known that renal function, a prerequisite for receipt of cisplatin-based chemotherapy, declines with age.32 However, it is important to recognize that not all individuals 65 years or older are “elderly,” and to know that a distinction should be made between chronological and functional age.33 A number of tools that incorporate factors such as comorbidity, functional status, cognition, and physical strength have been developed to help surgeons and medical oncologists assess frailty.34 A formal geriatrics consultation or the Comprehensive Geriatric Assessment can also help predict postoperative and chemotherapy-related morbidity.35,36 Advanced age should not be used as the sole factor in making decisions about treatment, and it should be considered as just one part of a patient’s overall health; functional status and other individual social and psychological factors must also be taken into account. Our data indicate that properly selected elderly patients can undergo NAC and RC, allowing them the best chance at survival. Further prospective studies that would include expert geriatric assessment in their design are needed to determine optimal management for this patient cohort.
Strengths and Limitations
Our study is the first to examine use of NAC in elderly patients undergoing RC using the NCDB. We found that patients ≥70 years receiving NAC and RC had perioperative morbidity comparable with those undergoing RC alone, and they had improved OS compared with those undergoing RC alone. Patients receiving RC and AC were included in the no-NAC cohort; however, given the typical timing of AC, we would not expect this to affect analysis of perioperative outcomes. We performed extensive PSW calculations based on patient and disease characteristics to balance the NAC and no-NAC subgroups to better mirror a clinical research design. Undoubtedly, healthier elderly patients are more often referred for NAC prior to surgery due to perceived increased robustness and lack of comorbidities. This may explain some of the improved perioperative outcomes in the NAC cohort. We attempted to account for this by including CCI score in our propensity matching. Although CCI score is a commonly used metric and higher scores have been associated with higher bladder cancer mortality,31 it is limited by its component parts. Nevertheless, our findings provide compelling evidence that, at the least, NAC does not increase perioperative morbidity and may improve overall survival in appropriately selected patients 70 years or older.
Limitations of this study include those inherent in a retrospective large national database study. Although we employed PSW to control for pretreatment characteristics, there are likely confounders we could not control for. Variables such as type of chemotherapy agents used, dose and number of cycles, renal function, performance status, and other comorbidities that might impact receipt of chemotherapy were not available in the NCDB. Furthermore, NCDB data are dependent on accuracy of data reporting and of billing/coding; this can be variable among individual coders and institutions. We were also faced with substantial missing data in our GST analysis. These data were excluded from our multivariate analysis, and presumably, missing data would be similar between both age cohorts; however, we cannot exclude the possibility that this may have affected our results. We were also limited in assessment of cancer-specific survival and quality-of-life outcomes, as these data are not coded in the NCDB. Finally, the NCDB includes only data for CoC-accredited facilities and, therefore, may not be generalizable to other institutions.
Conclusions
NAC is more frequently omitted in patients 70 years or older, but in appropriately selected elderly patients, NAC and RC has comparable perioperative outcomes and improved OS to RC alone. This patient population deserves increased consideration for GST and advanced age should not independently preclude patients from being offered NAC prior to RC. Further study is needed to develop better prognostic tools to identify the elderly patients who may benefit from receipt of chemotherapy.
AUTHOR AFFILIATIONS:
Natasza Posielski, MD1; Hannah Koenig, MPH1; On Ho, PhD1; Christopher Porter, MD1; John Paul Flores, MD1
1. Virginia Mason Hospital and Seattle Medical Center, Seattle, WA
Acknowledgment
The National Cancer Database (NCDB) is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society. The data used in the study are derived from a deidentified NCDB file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed or for the conclusions drawn from these data by the investigators.
Funding: None
Conflicts of interest: None
References
1. Cancer stat facts: bladder cancer. National Cancer Institute / Surveillance, Epidemiology, and End Results Program. Accessed April 9, 2021. https://seer.cancer.gov/statfacts/html/urinb.html
2. NCCN. Clinical Practice Guidelines in Oncology. Bladder cancer, version 6.2021. Accessed December 9, 2020. https://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf
3. Grossman HB, Natale RB, Tangen CM, et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N Engl J Med. 2003;349(9):859-866. doi:10.1056/NEJMoa022148
4. Advanced Bladder Cancer (ABC) Meta-analysis Collaboration. Neoadjuvant chemotherapy in invasive bladder cancer: update of a systematic review and meta-analysis of individual patient data advanced bladder cancer (ABC) meta-analysis collaboration. Eur Urol. 2005;48(2):202-205; discussion 205-206. doi:10.1016/j.eururo.2005.04.006
5. Chau C, Wheater M, Geldart T, Crabb SJ. Clinical outcomes following neoadjuvant cisplatin-based chemotherapy for bladder cancer in elderly compared with younger patients. Eur J Cancer Care (Engl). 2015;24(2):155-162. doi:10.1111/ecc.12282
6. Leone AR, Zargar-Shoshtari K, Diorio GJ, et al. Neoadjuvant chemotherapy in elderly patients with bladder cancer: oncologic outcomes from a single institution experience. Clin Genitourin Cancer. 2017;15(4):e583-e589. doi:10.1016/j.clgc.2017.01.014
7. Huo J, Ray-Zack MD, Shan Y, et al. Discerning patterns and quality of neoadjuvant chemotherapy use among patients with muscle-invasive bladder cancer. Eur Urol Oncol. 2019;2(5):497-504. doi:10.1016/j.euo.2018.07.009
8. Galsky MD. How I treat bladder cancer in elderly patients. J Geriatr Oncol. 2015;6(1):1-7. doi:10.1016/j.jgo.2014.11.006
9. Fonteyne V, Ost P, Bellmunt J, et al. Curative treatment for muscle invasive bladder cancer in elderly patients: a systematic review. Eur Urol. 2018;73(1):40-50. doi:10.1016/j.eururo.2017.03.019
10. Froehner M, Koch R, Hübler M, et al. Predicting 90-day and long-term mortality in octogenarians undergoing radical cystectomy. BMC Urol. 2018;18(1):91. doi:10.1186/s12894-018-0402-z
11. Thiruthaneeswaran N, Choudhury A. Exploring trends in advanced bladder cancer using the NCDB: turning data into information and information into insight. Transl Androl Urol. 2018;7(4):754-756. doi:10.21037/tau.2018.06.15
12. Olmos A, Govindasamy P. A practical guide for using propensity score weighting in R. Practical Assessment, Research and Evaluation. 2015; 20(13). doi:10.7275/JJTM-R398
13. The US population is aging. Urban Institute. December 16, 2014. Accessed April 21, 2021. https://www.urban.org/policy-centers/cross-center-initiatives/program-retirement-policy/projects/data-warehouse/what-future-holds/us-population-aging
14. Gray PJ, Fedewa SA, Shipley WU, et al. Use of potentially curative therapies for muscle-invasive bladder cancer in the United States: results from the National Cancer Data Base. Eur Urol. 2013;63(5):823-829. doi:10.1016/j.eururo.2012.11.015
15. Noon AP, Albertsen PC, Thomas F, Rosario DJ, Catto JWF. Competing mortality in patients diagnosed with bladder cancer: evidence of undertreatment in the elderly and female patients. Br J Cancer. 2013;108(7):1534-1540. doi:10.1038/bjc.2013.106
16. Konety BR, Joslyn SA. Factors influencing aggressive therapy for bladder cancer: an analysis of data from the SEER program. J Urol. 2003;170(5):1765-1771. doi:10.1097/01.ju.0000091620.86778.2e
17. Williams SB, Huo J, Chamie K, et al. Underutilization of radical cystectomy among patients diagnosed with clinical stage T2 muscle-invasive bladder cancer. Eur Urol Focus. 2017;3(2-3):258-264. doi:10.1016/j.euf.2016.04.008
18. Gore JL, Litwin MS, Lai J, et al; Urologic Diseases in America Project. Use of radical cystectomy for patients with invasive bladder cancer. J Natl Cancer Inst. 2010;102(11):802-811. doi:10.1093/jnci/djq121
19. Lughezzani G, Sun M, Shariat SF, et al. A population-based competing-risks analysis of the survival of patients treated with radical cystectomy for bladder cancer. Cancer. 2011;117(1):103-109. doi:https://doi.org/10.1002/cncr.25345
20. Chang SS, Bochner BH, Chou R, et al. Treatment of non-metastatic muscle- invasive bladder cancer: AUA/ASCO/ASTRO/SUO guideline. J Urol. 2017;198(3):552-559. doi:10.1016/j.juro.2017.04.086
21. Abdollah F, Sun M, Shariat SF, et al. The importance of pelvic lymph node dissection in the elderly population: implications for interpreting the 2010 National Comprehensive Cancer Network practice guidelines for bladder cancer treatment. J Urol. 2011;185(6):2078-2084. doi:10.1016/j.juro.2011.02.022
22. Schmid M, Rink M, Traumann M, et al; PROMETRICS 2011 Research Group. Evidence from the ‘PROspective MulticEnTer RadIcal Cystectomy Series 2011 (PROMETRICS 2011)’ study: how are preoperative patient characteristics associated with urinary diversion type after radical cystectomy for bladder cancer? Ann Surg Oncol. 2015;22(3):1032-1042. doi:10.1245/s10434-014-4029-3
23. Fairey A, Chetner M, Metcalfe J, et al. Associations among age, comorbidity and clinical outcomes after radical cystectomy: results from the Alberta Urology Institute radical cystectomy database. J Urol. 2008;180(1):128-134; discussion 134. doi:10.1016/j.juro.2008.03.057
24. Yamanaka K, Miyake H, Hara I, Inoue TA, Fujisawa M. Significance of radical cystectomy for bladder cancer in patients over 80 years old. Int Urol Nephrol. 2007;39(1):209-214. doi:10.1007/s11255-006-9122-5
25. Figueroa AJ, Stein JP, Dickinson M, et al. Radical cystectomy for elderly patients with bladder carcinoma: an updated experience with 404 patients. Cancer. 1998;83(1):141-147. doi:10.1002/(sici)1097-0142(19980701)83:1<141::aid-cncr19>3.0.co;2-x
26. Tilki D, Zaak D, Trottmann M, et al. Radical cystectomy in the elderly patient: a contemporary comparison of perioperative complications in a single institution series. World J Urol. 2010;28(4):445-450. doi:10.1007/s00345-009-0482-1
27. Portella Fontana P, Alonso y Gregorio S, Rivas JG, et al. Perioperative and survival outcomes of laparoscopic radical cystectomy for bladder cancer in patients over 70 years. Cent European J Urol. 2015;68(1):24-29. doi:10.5173/ceju.2015.01.498
28. Haden TD, Prunty MC, Jones AB, Deroche CB, Murray KS, Pokala N. Comparative perioperative outcomes in septuagenarians and octogenarians undergoing radical cystectomy for bladder cancer—do outcomes differ? Eur Urol Focus. 2018;4(6):895-899. doi:10.1016/j.euf.2017.08.005
29. Trulson JJ, Sharma P, Haden T, Kheterpal E, Pokala N. Comparative survival following different treatment modalities for stage T2 bladder cancer in octogenarians. World J Urol. 2014;32(2):425-429. doi:10.1007/s00345-013-1123-2
30. Mottet N, Ribal MJ, Boyle H, et al. Management of bladder cancer in older patients: position paper of a SIOG Task Force. J Geriatr Oncol. 2020;11(7):1043-1053. doi:10.1016/j.jgo.2020.02.001
31. Boorjian SA, Kim SP, Tollefson MK, et al. Comparative performance of comorbidity indices for estimating perioperative and 5-year all cause mortality following radical cystectomy for bladder cancer. J Urol. 2013;190(1):55-60. doi:10.1016/j.juro.2013.01.010
32. Dash A, Galsky MD, Vickers AJ, et al. Impact of renal impairment on eligibility for adjuvant cisplatin-based chemotherapy in patients with urothelial carcinoma of the bladder. Cancer. 2006;107(3):506-513. doi:10.1002/cncr.22031
33. Bellmunt J, Mottet N, De Santis M. Urothelial carcinoma management in elderly or unfit patients. EJC Suppl. 2016;14(1):1-20. doi:10.1016/j.ejcsup.2016.01.001
34. Skinner EC. Treatment of muscle-invasive bladder cancer in older patients. Am Soc Clin Oncol Educ Book. 2016;35:e228-e233. doi:10.1200/EDBK_158974
35. Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet. 1993;342(8878):1032-1036. doi:10.1016/0140-6736(93)92884-V
36. Wedding U, Ködding D, Pientka L, Steinmetz HT, Schmitz S. Physicians’ judgement and comprehensive geriatric assessment (CGA) select different patients as fit for chemotherapy. Crit Rev Oncol Hematol. 2007;64(1):1-9. doi:10.1016/j.critrevonc.2007.05.001