A Large Cystic Pancreatic Mass in a 45-Year-Old Female
The patient is an otherwise healthy 45-year-old female who presented to her primary care physician with 6 weeks of increasing left upper quadrant abdominal pain with radiation to the back. She underwent an abdominal ultrasound, which revealed a large cystic abdominal mass.
The Case:The patient is an otherwise healthy 45-year-old female who presented to her primary care physician with 6 weeks of increasing left upper quadrant abdominal pain with radiation to the back. She underwent an abdominal ultrasound, which revealed a large cystic abdominal mass. Subsequent abdominal CT and MRI results confirmed a large 12 × 13-cm complex cystic mass arising from the tail of the pancreas, with multiple septations, peripheral calcifications, and septal enhancement (Figure 1). The patient’s imaging also showed chronic occlusion of the splenic vein with extensive collateral formation. Pertinent labs included a hemoglobin level of 11.2 g/dL and a white blood cell count of 19.6 × 106/L, with 93% neutrophils. Blood chemistries were normal; the serum albumin level was 3.3 g/dL; carbohydrate antigen 19-9 (CA 19-9) level was elevated at 84 U/mL. Cyst fluid sampling revealed an amylase level of 25 U/L.
FIGURE 1

The Patient's 13-cm Mucinous Cystic Neoplasm Is Indicated by Arrows.
After presentation at a multidisciplinary pancreas clinic, the differential diagnosis included intraductal papillary mucinous neoplasm (IPMN), solid pseudopapillary neoplasm, and mucinous cystic neoplasm (MCN). The patient was taken to the operating room, and a distal pancreatectomy and splenectomy were performed. Pathology revealed a 13-cm solid and cystic multiloculated MCN. Histology showed cysts lined by bland columnar mucinous epithelium with spindled pericystic “ovarian-type” stroma, which transitioned into complex high-grade dysplasia associated with an invasive, poorly differentiated carcinoma with anaplastic nuclei. The surgical margin was free of tumor. Lymphovascular invasion was identified (Figure 2), but all 20 examined lymph nodes were free of tumor.
FIGURE 2
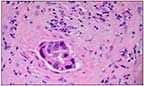
Lymphovascular Invasion Is Evident in the Center of This Pathology Slide.
The patient recovered from the surgery without incident. She was seen 3 weeks post-surgery for follow-up evaluation and possible enrollment in an adjuvant clinical trial, and had repeat CT imaging. The CT scan revealed numerous new liver metastases not seen on prior imaging. Interventional radiology obtained a hepatic biopsy specimen of a left lobe liver metastasis, which revealed metastatic poorly differentiated carcinoma consistent with the original pancreatic MCN. The patient was subsequently offered palliative chemotherapy for metastatic pancreatic cancer.
Discussion
Prior to the 1970s, cystic neoplasms of the pancreas were considered rare, and if discovered, were almost always found to be benign. However, in 1978, colleagues Compagno and Oertel published data that histologically delineated mucinous from serous cystic neoplasms (SCNs) of the pancreas.[1] Years later, the World Health Organization (WHO) further classified the mucin-producing cysts into two separate categories, MCNs and IPMNs, and in 2000 the WHO emphasized the importance of ovarian-type stroma for diagnosis of MCN.[2,3]
Recent data from the United Kingdom’s National Cancer Intelligence Network showed that between 1998 and 2006 there was a slight but significant increase in the incidence of cystic neoplasms in females aged 20 to 39 and 50 to 59. This recent increase can be attributed to the advent of enhanced CT and MRI imaging, which has yielded more diagnoses of these previously undetected and generally benign cysts, specifically the increased rates of MCN and IPMN diagnoses.
However, overall, MCNs are relatively uncommon tumors that comprise about 25% of all resected cystic neoplasms of the pancreas.[4] This patient’s presentation possessed typical features of MCNs, including a predilection for development in women (95%) and pancreatic body and tail involvement (> 95%).[5,6]
There are numerous imaging modalities that can assess for malignancy; however, the presence of peripheral calcifications within the patient’s tumor, found on imaging, is nearly pathognomonic for MCN and is a marker of increased malignant risk. Moreover, the patient was optimally imaged with MRI (in a recent study by Theruvath et al, CT proved less effective than MRI at predicting the diagnosis of MCN [9% vs 45%].[7]).
Cystic fluid analysis is also helpful in distinguishing between MCNs and SCNs; particularly helpful in this case was the positive mucin stain or high viscosity that was displayed in the patient’s fluid specimen. Also, the patient’s amylase level was 25 U/L, which was consistent with MCN; a high amylase level (> 5× the upper limit of normal) suggests pancreatic pseudocyst or IPMN
Histologically, MCNs are characterized by cysts lined by columnar mucin-producing cells surrounded by dense spindled ovarian-type stroma, which is immunoreactive for estrogen receptor and progesterone receptor. It has been suggested that the ovarian stroma results from the fact that the dorsal pancreas and the buds of the genital tract lie adjacent to one another during embryogenesis. MCNs can demonstrate various degrees of atypia, from adenoma to invasive carcinoma. Typically, they do not involve the main pancreatic duct, which distinguishes them from IPMNs.
FIGURE 3

The Arrows Identify Liver Metastases, Which Were Pathologically Confirmed on CT-Guided Biopsy.
This patient’s tumor contained features associated with increased malignant potential, including large tumor size (13 cm) and a visible solid component.[5,8] Interestingly, although the patient developed radiographic evidence of liver metastases (Figure 3) within 4 weeks of repeat imaging, all 20 peripancreatic lymph nodes were negative for tumor, indicating pure hematogenous spread.
Surgical excision is indicated for all MCNs considered premalignant or malignant. Gemcitabine is the standard chemotherapy for advanced pancreatic cancer, and its effectiveness against advanced MCNs has been reported.[9] Gemcitabine-oxaliplatin treatment has also been proposed to be effective if not superior in terms of clinical progression-free survival.[10] Otherwise, management is similar to that of pancreatic adenocarcinoma, including the use of FOLFIRINOX (5-fluorouracil, leucovorin, irinotecan, oxaliplatin) or gemcitabine plus albumin-bound paclitaxel (Abraxane).
Nonetheless, survival results remain disappointing, as patients with invasive MCNs have a 5-year survival rate of 20% to 60%.[11] In this case, in light of the patient’s high-grade histology and rapid progression, her chances of 3-year survival are estimated to be lower than 5%.[5,6]
References:
REFERENCES
1. Compagno J, Oertel JE. Mucinous cystic neoplasms of the pancreas with overt and latent malignancy (cystadenocarcinoma and cystadenoma). A clinicopathologic study of 41 cases. Am J Clin Pathol. 1978;69:573-80.
2. Kloppel G, Solcia E, Longnecker DS, et al. World Health Organization international histological classification of tumours: histological typing of tumors of the exocrine pancreas. Berlin: Heidelberg; NewYork: Springer; 1996.
3. Zamboni G, Kloppel G, Hruban RH, et al. Mucinous cystic neoplasms of the pancreas. In: Hamilton SR, Aaltonen LA, editors. World Health Organization classification of tumours: pathology and genetics of tumours of the digestive system. Lyon: IARC Press; 2000. p. 237-40.
4. Valsangkar NP, Morales-Oyarvide V, Thayer SP, et al. 851 resected cystic tumors of the pancreas: a 33-year experience at the Massachusetts General Hospital. Surgery. 2012;152(3 suppl 1):S4-S12.
5. Crippa S, Salvia R, Warshaw AL, et al. Mucinous cystic neoplasm of the pancreas is not an aggressive entity: lessons from 163 resected patients. Ann Surg. 2008;247:571-9.
6. Le Baleur Y, Couvelard A, Vullierme MP, et al. Mucinous cystic neoplasms of the pancreas: definition of preoperative imaging criteria for high-risk lesions. Pancreatology. 2011;11:495-9.
7. Theruvath TP, Morgan KA, Adams DB. Mucinous cystic neoplasms of the pancreas: how much preoperative evaluation is needed? Am Surg. 2010;76:812-7.
8. Goh BK, Tan YM, Chung YF, et al. A review of mucinous cystic neoplasms of the pancreas defined by ovarian-type stroma: clinicopathological features of 344 patients. World J Surg. 2006;30:2236-45.
9. Shimada K, Iwase K, Aono T, et al. A case of advanced mucinous cystadenocarcinoma of the pancreas with peritoneal dissemination responding to gemcitabine. Gan To Kagaku Ryoho. 2009;36:995-8.
10. Obayashi K, Ohwada S, Sunose Y, et al. Remarkable effect of gemcitabine-oxaliplatin (GEMOX) therapy in a patient with advanced metastatic mucinous cystic neoplasm of the pancreas. Gan To Kagaku Ryoho. 2008;35:1915-7.
11. Testini M, Gurrado A, et al. Management of mucinous cystic neoplasms of the pancreas. World J Gastroenterol. 2010;16:5682-92.