Large Study Confirms Accuracy of Sentinel Node Biopsy
LOS ANGELES-A large German multicenter study has shown that sentinel lymph node (SLN) biopsy for breast cancer accurately predicts the status of the axillary lymph node. In addition, the study found that physician experience and the choice of lymphography technique-blue dye or scintigraphy-influence the detection rate significantly.
LOS ANGELESA large German multicenter study has shown that sentinel lymph node (SLN) biopsy for breast cancer accurately predicts the status of the axillary lymph node. In addition, the study found that physician experience and the choice of lymphography techniqueblue dye or scintigraphyinfluence the detection rate significantly.
Speaking at the 49th Annual Meeting of the Society of Nuclear Medicine (abstract 1170), Andreas Buck, MD, of the University of Ulm, Germany, reported results from 814 breast cancer patients who underwent SLN biopsy and consecutive axillary lymph node dissection.
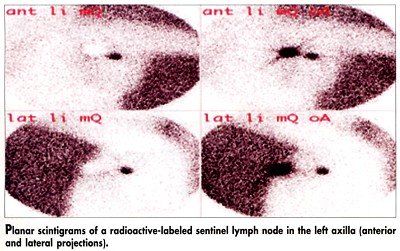
The 80 surgeons involved in the study were free to choose their lymphography technique. The blue dye technique was used in 137 patients, scintigraphy in 169 (see Figure), and combined blue dye/scintigraphy in 503. The results showed that detection of the sentinel lymph node was highest when the blue dye and scintigraphy techniques were combined (89.6%). Use of blue dye and scintigraphy alone gave SLN detection rates of 71.6% and 78.8%, respectively.
In the scintigraphy technique, the combined subdermal/peritumoral injection of the radiotracer produced a significantly higher SLN detection rate than subdermal or peritumoral injection alone (96.8%, 84.6%, and 78.6%, respectively; P < .001). Furthermore, there was a close relationship between the number of sentinel lymph node procedures performed by a physician and the detection rate.
The overall sensitivity for SLN biopsy in detecting lymph node metastases was 91.3%. "Sentinel lymph node biopsy is a powerful tool to estimate the axillary lymph node status with minimal invasiveness," Dr. Buck said. "If the SLN tumor is negative, the whole axillary lymph node status can be considered negative." He added that "it remains unclear how the sensitivity of SLN biopsy can be increased and what rate of false-negative findings is acceptable."
Not All Are Eligible
Dr. Andreas pointed out that not all breast cancer patients are eligible for SLN scintigraphy. It is most appropriate in women with unifocal breast cancers less than 3 cm, who have negative clinical examination by palpation and ultrasound of the axilla, and who have not had previous surgery. The detection rate of SLN scintigraphy is lower in patients who have had lumpectomies, he said.
Giredestrant Combo Yields Positive PFS in Subgroups After CDK4/6i in ER+/HER2– Breast Cancer
December 13th 2025“The magnitude of clinical benefit was clinically meaningful and consistent, and was regardless of PIK3CA mutations or alterations in the PIK3CA pathway, duration of prior CDK4/6 inhibitors, including patients who progress within 6 to 12 months, and the choice of prior CDK4/6 inhibitors,” said Hope S. Rugo, MD.