Leptomeningeal Enhancement in a 58-Year-Old Woman
The patient is a 58-year-old woman who was diagnosed at an outside hospital with a World Health Organization (WHO) grade III non–contrast-enhancing right frontal anaplastic astrocytoma, with spread into the genu of the corpus callosum.
Figure 1: Brain MRI Post-Contrast, Axial View
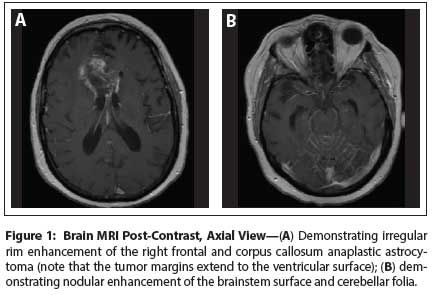
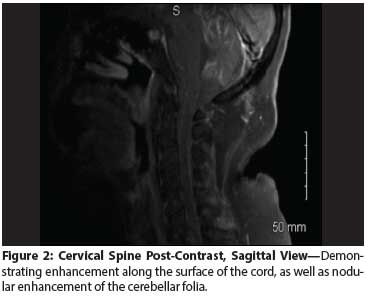
Figure 2: Cervical Spine Post-Contrast, Sagittal View
The Case:The patient is a 58-year-old woman who was diagnosed at an outside hospital with a World Health Organization (WHO) grade III non–contrast-enhancing right frontal anaplastic astrocytoma, with spread into the genu of the corpus callosum. The diagnosis was established by brain biopsy; genetic markers were not obtained. She subsequently was treated with standard chemoradiation. Approximately 4 weeks after the completion of chemoradiation, serial imaging showed new nodular rim enhancement of the right frontal tumor and new leptomeningeal enhancement of the cerebellar folia and the surface of the brainstem. Clinically, her family reported cognitive decline with waxing and waning confusion. She was restarted on dexamethasone, resulting in symptom resolution; in addition, adjuvant temozolomide was initiated. A follow-up brain MRI 1 month later showed significant improvement in the enhancement of the right frontal tumor bed, but increased leptomeningeal enhancement.
Over the following 4 weeks, the patient exhibited a more precipitous functional decline, with headache, confusion, vertigo, expressive aphasia, paraplegia, right arm weakness, and paresthesia of the extremities. Brain and spine MRIs demonstrated enlargement of the right frontal rim-enhancing lesion, with increased perfusion corresponding to the enhancing components. In addition, there was further increased extent and thickness of leptomeningeal enhancement along the surface of the brainstem, the cervical and thoracic spinal cord, and the cerebellar folia, as well as nodular enhancement of the cauda equina nerves. There was no ventriculomegaly. The patient was transferred to University of Colorado Hospital, where a diagnosis of leptomeningeal metastases from her glioma was established on the basis of known cancer abutting the ventricular system, symptoms and signs suggestive of leptomeningeal tumor spread, and corresponding imaging findings. The patient deferred lumbar puncture for cerebrospinal fluid (CSF) examination.
Discussion
Reports of leptomeningeal dissemination of malignant gliomas are rare. Clinically relevant leptomeningeal tumor dissemination occurs in 1% to 2% of cases of gliomas, and is seen most often in young patients with prolonged survival times.[1] However, one case series noted early leptomeningeal dissemination within a year of initial glioma diagnosis in 40% of reported cases.[2] An autopsy series reported leptomeningeal seeding in 6% to 20% of cases.[1]
The primary mechanism for leptomeningeal metastases in gliomas appears to be juxtaposition of the tumor and CSF spaces. Surgical opening of the ventricles during tumor resection has been reported to be a risk factor for leptomeningeal glioma dissemination in several series, and tumor seeding along a biopsy track is well-described.[1,3] Additional potential mechanisms of tumor dissemination include hematogenous spread with tumor spillage into the Virchow-Robin spaces and eventually into the subarachnoid space, or tumor spread into the choroid plexus, with subsequent CSF seeding.
The diagnosis of leptomeningeal metastases is based on clinical signs and symptoms, MRI, and CSF analysis. The clinical picture of leptomeningeal metastases classically involves symptoms and signs referable to multiple levels of the neuraxis-the brain, cranial nerves, spine, and nerve roots. Common symptoms include headache, confusion, nausea/vomiting, diplopia, cerebellar dysfunction, back pain, and leg weakness. Identification of malignant cells by CSF cytology is the diagnostic gold standard. However, 3 lumbar punctures are required to obtain a diagnostic sensitivity of 86% to 90% in leptomeningeal metastases, and even then 10% to 14% of patients with metastases will have a negative CSF cytological examination.[4] False-negative CSF cytology is particularly common in in glioma patients with leptomeningeal metastases, with case series uniformly reporting negative cytology in most, if not all, patients.[1,5] Elevated CSF protein has been proposed by some as a surrogate marker for leptomeningeal tumor dissemination in gliomas.[1]
MRI has proven to be an important diagnostic tool for leptomeningeal metastases, with a diagnostic sensitivity of nearly 70%.[6] An MRI with findings characteristic of leptomeningeal metastases in a patient with an established cancer diagnosis and signs and symptoms suggestive of leptomeningeal metastases is often the sole diagnostic tool for many clinicians.[4] A retrospective review of 187 patients diagnosed with leptomeningeal metastases at Memorial Sloan-Kettering Cancer Center reported that CSF analysis was not done in 45% of patients.[7] Subarachnoid-enhancing nodules of the brain, spinal cord, or nerve roots; sulcal or spinal cord surface enhancement; and cranial nerve or nerve root enhancement are characteristic of leptomeningeal tumor dissemination.[8] Communicating hydrocephalus and thickening of nerve roots in the cauda equina may also be seen.[8]
The diagnosis of leptomeningeal metastases in gliomas requires heightened suspicion, recognition of clinical symptoms and signs suggestive of leptomeningeal tumor seeding, as well as MRI findings consistent with this rare clinical entity and positive CSF cytology. There is an exceptionally high false-negative CSF cytology rate in glioma patients with leptomeningeal metastases, but additional CSF parameters can further support the diagnosis and serve to exclude other diagnoses.
Outcome of this case
Leptomeningeal metastasis is a uniformly fatal diagnosis, with an average survival of 4 months from the time of diagnosis, and only rare case reports of survival up to 20 months following diagnosis.[9] Therapeutic interventions are based on single case reports or small case series, and generally are focused on reversal of neurologic deficits and pain control. Potential interventions include corticosteroids, external beam irradiation to symptomatic areas, intravenous or intrathecal chemotherapy, craniospinal irradiation, and anti-angiogenic agents such as bevacizumab.[9,10] Our patient received bevacizumab therapy at standard dosing, with the most significant improvement seen in cognition, headache, vertigo, and right arm strength. Some improvement in paraplegia was also seen, but to date this has not been functionally significant.
Financial Disclosure: The author has no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Bae JS, Yang SH, Yoon WS, et al. The clinical features of spinal leptomeningeal dissemination from malignant gliomas. J Korean Neurosurg Soc. 2011;49:334-8.
2. Arita N, Taneda M, Hayakawa T. Leptomeningeal dissemination of malignant gliomas. Incidence, diagnosis and outcome. Acta Neurochir (Wien). 1994;126:84-92.
3. Pierallini A, Caramia F, Piattella MC, et al. Metastasis along the stereotactic biopsy trajectory in glioblastoma multiforme. Acta Neurochir (Wien). 1999;141:1011-2.
4. Clarke JL, Perez HR, Jacks LM, et al. Leptomeningeal metastases in the MRI era. Neurology. 2010;74:1449-54.
5. Onda K, Tanaka R, Takahashi H, et al. Symptomatic cerebrospinal fluid dissemination of cerebral glioblastoma. Computed tomographic findings in 11 cases. Neuroradiology. 1990;32:146-50.
6. van Oostenbrugge RJ, Twijnstra A. Presenting features and value of diagnostic procedures in leptomeningeal metastases. Neurology. 1999;53:382-5.
7. DeAngelis LM, Boutros D. Leptomeningeal metastasis. Cancer Invest. 2005;23:145-54.
8. Freilich RJ, Krol G, DeAngelis LM. Neuroimaging and cerebrospinal fluid cytology in the diagnosis of leptomeningeal metastasis. Ann Neurol. 1995;38:51-7.
9. Lawton CD, Nagasawa DT, Yang I, et al. Leptomeningeal spinal metastases from glioblastoma multiforme: treatment and management of an uncommon manifestation of disease. J Neurosurg Spine. 2012;17:438-448.
10. Fiorentino A, Caivano R, Chiumento C, et al. Radiotherapy and bevacizumab for intramedullary and leptomeningeal metastatic glioblastoma: a case report and review of the literature. Int J Neurosci. 2012;122:691-4.