Liposomal Irinotecan Yields High Responses, Similar OS Vs Topotecan in SCLC
Overall survival and progression-free survival appear comparable in patients with relapsed small cell lung cancer treated with liposomal irinotecan vs topotecan.
Patients with relapsed small cell lung cancer (SCLC) who were treated with liposomal irinotecan experienced comparable overall survival (OS) and progression-free survival (PFS) vs topotecan, although the former induced more responses, according to data from part 2 of the phase 2/3 RESILIENT study (NCT03088813).
Among patients with relapsed SCLC, liposomal irinotecan produced a higher overall response rate vs topotecan in part 2 of the phase 2/3 RESILIENT study.
The median OS was 7.9 months (95% CI, 6.9-9.2) in the liposomal irinotecan arm compared with 8.3 months (95% CI, 7.3-9.1) in the topotecan arm (hazard ratio [HR], 1.11; 95% CI, 0.90-1.37; P = .3094). Additionally, PFS by blinded independent central review was 4.0 months (95% CI, 3.0-4.2) vs 3.3 months (95% CI, 2.8-4.1) in each respective arm (HR, 0.96; 95% CI, 0.77-1.20; P = .7053)
The overall response rate (ORR) in the experimental arm was 44.1% (95% CI, 37.6%-50.8%) compared with 21.6% in the control arm (95% CI, 16.4%-27.4%; P <.0001). Investigators reported a complete response (CR) rate of 5.2%, a partial response (PR) rate of 38.9%, a stable disease rate of 29.7%, and a progressive disease rate of 12.2% in the liposomal irinotecan cohort; the CR, PR, stable disease, and progressive disease rates in the topotecan arm were 3.0%, 18.5%, 42.2%, and 21.6%, respectively.
In part 2 of the open-label phase 2/3 RESILIENT trial, patients were randomly assigned 1:1 to receive either 70 mg/m2 of intravenous liposomal irinotecan every 2 weeks or 1.5 mg/m2 of intravenous topotecan daily for 5 days every 3 weeks.
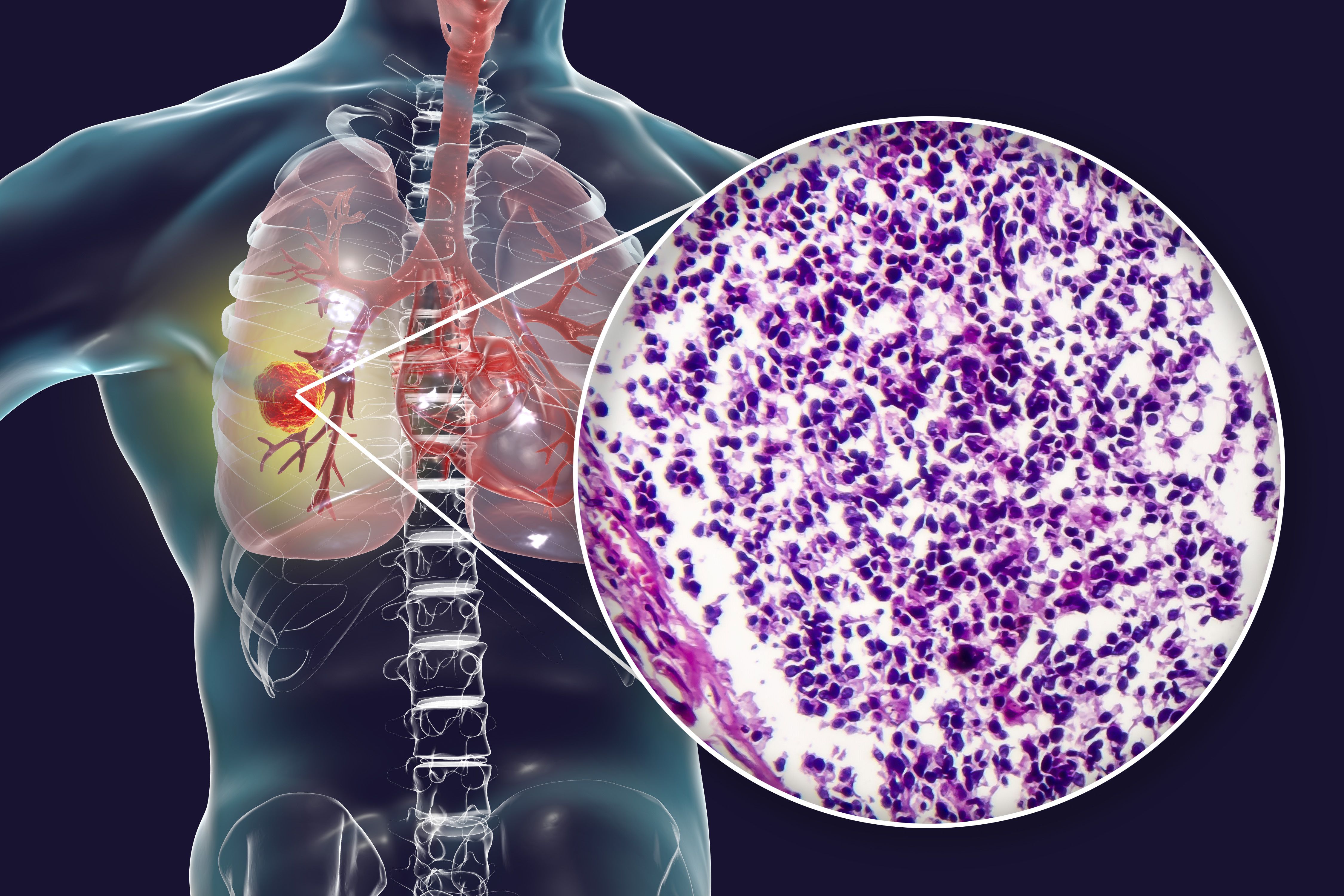
The study included a total of 461 patients with histologically or cytologically confirmed SCLC and radiographically confirmed progression following 1 line of platinum-based chemotherapy. Patients also needed to have an ECOG performance status of 0 or 1.
The primary end point was OS, with key secondary end points including PFS and ORR.
Patients across both cohorts had a median age of 62.3 years, and 32.1% were women. Additionally, most patients had an ECOG performance status of 1 (74.2%) and metastatic disease (88.7%). Sites of metastases included the brain and/or central nervous system (28.6%), hepatic (6.9%), and bone and locomotor (23.6%). Patients previously received treatment with radiotherapy (51.0%), immunotherapy (18.4%), and targeted therapy (0.4%).
The median duration of treatment was 19 weeks in each arm. In the liposomal irinotecan arm and topotecan arms, respectively, any-grade treatment-emergent adverse effects (TEAEs) occurred in 96.0% and 99.1% of patients. Moreover, any treatment-related TEAEs were identified in 86.3% and 96.0% of patients in each respective group.
Most patients in each arm experienced grade 3 or higher AEs (62.4% vs 87.9%). Additionally, 46.5% vs 39.5% of patients in each respective arm had serious TEAEs, and 8.4% vs 4.0% had TEAEs leading to death.
Common grade 3 or higher TEAEs in the experimental arm included diarrhea (13.7%), neutropenia (8.0%), neutrophil count decrease (4.4%), leukopenia (4.0%), anemia (2.7%), platelet count decrease (1.3%), and thrombocytopenia (0.4%). In the control arm, common high-grade TEAEs included neutropenia (51.6%), anemia (30.9%), leukopenia (29.1%), thrombocytopenia (29.1%), neutrophil count decrease (17.5%), platelet count decrease (17.5%), white blood cell count decrease (10.8%), and diarrhea (1.3%).
Investigators presented these findings at the European Lung Cancer Congress 2023.
Reference
Rudin CM, Dowlati A, Chen Y, et al. RESILIENT part 2: a randomized, open-label phase 3 study of liposomal irinotecan versus topotecan in adults with relapsed small cell lung cancer (SCLC). Presented at: European Lung Cancer Congress 2023; March 29-April 1, 2023; Copenhagen, Denmark. Abstract 1610. https://bit.ly/3GSnxhM