Lorlatinib Boosts Progression-Free Survival in ALK+ NSCLC
Lorlatinib may show “unprecedented” improvements in outcomes for those with advanced ALK-positive NSCLC, according to Benjamin J. Solomon, MBBS, PhD.
"The systemic efficacy results coupled with prolonged intracranial efficacy from first line lorlatinib treatment indicate that this provides an unprecedented improvement in outcomes for patients with advanced ALK-positive NSCLC," according to Benjamin J. Solomon, MBBS, PhD.
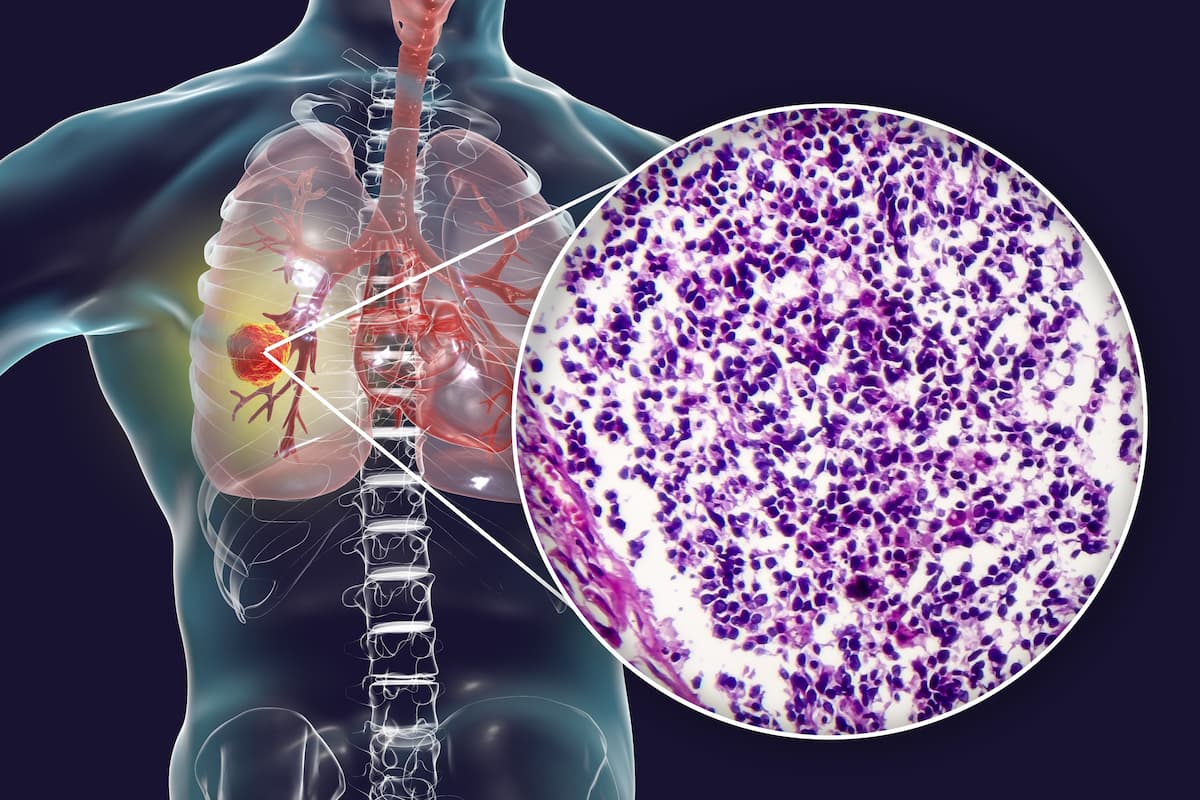
Frontline lorlatinib (Lorbrena) improved progression-free survival (PFS) compared with crizotinib (Xalkori) and demonstrated the longest PFS outcomes ever highlighted in advanced ALK-positive non–small cell lung cancer (NSCLC), according to findings from the phase 3 CROWN trial (NCT03052608) presented in a press briefing ahead of the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting.
Findings from the study revealed that the median PFS was not reached (NR; 95% CI, 64.3-NR) in the lorlatinib arm (n = 149) compared with 9.1 months (95% CI, 7.4-10.9) in the crizotinib arm (n = 147; HR, 0.19; 95% CI, 0.13-0.27). The 5-year PFS rates were 60% vs 8%, respectively, with a median duration of follow-up for PFS of 60.2 months (95% CI, 57.4-61.6) in the lorlatinib arm vs 55.1 months (95% CI, 36.8-62.5) in the crizotinib arm. No new safety signals were reported with lorlatinib.
“These results represent the most significant PFS benefit that has been reported in ALK-positive lung cancer to date. Overall survival [OS] follow-up is ongoing as insufficient survival events have been reached to trigger the protocol-specified analysis for OS,” Benjamin J. Solomon, MBBS, PhD, a medical oncologist atPeter MacCallum Cancer Centre in Melbourne, Australia, said in a presentation of the data.
“The PFS is outstanding; we have not seen anything close to this. Other great drugs that are available including alectinib [Alecensa] and brigatinib [Alunbrig] have not reported durable PFS events of this magnitude,” David R. Spigel, MD, a medical oncologist and the chief scientific officer at Sarah Cannon Research Institute in Nashville, Tennessee, added in a discussion of the data.
Treatment with the third-generation ALK-directed TKI also resulted in benefit across patient subgroups, regardless of presence of brain metastases, ethnic origin, sex, age, and smoking status. Patients with brain metastases at baseline experienced a median PFS of NR (95% CI, 32.9-NR) when treated with lorlatinib (n = 35) vs 6.0 months (95% CI, 3.7-7.6) with crizotinib (n = 38; HR, 0.08; 95% CI, 0.04-0.19). Patients without brain metastases at baseline in the lorlatinib arm (n = 114) experienced a median PFS of NR (95% CI, 64.3-NR) compared with 10.8 months (95% CI, 9.0-12.8) for those in the crizotinib arm (n = 109; HR, 0.24; 95% CI, 0.16-0.36); the 5-year PFS rates were 63% vs 10%, respectively.
“This study was originally reported in 2020 after 18 months of follow-up and was positive for its primary end point with a HR of 0.28 [95% CI, 0.19-0.41] and a median PFS that had not been reached with lorlatinib. On the basis of these initial results, lorlatinib was approved as first-line treatment globally [in March 2021],” Solomon added.
CROWN enrolled patients with stage IIIB/IV ALK-positive NSCLC who had not received prior systemic treatment for metastatic disease. Patients had an ECOG performance status of 2 or less and at least 1 extracranial measurable target lesion with no prior radiation required. Patients with asymptomatic treated or untreated central nervous system metastases were also eligible. Additionally, no crossover between treatment arms was permitted. Following random assignment, patients were stratified by presence of brain metastases (yes vs no) and ethnicity (Asian vs non-Asian).
Patients were randomly assigned 1:1 to receive lorlatinib 100 mg daily or crizotinib 250 mg twice daily. The primary end point of the study was PFS by blinded independent central review and secondary end points included OS, PFS by investigator assessment, safety, and objective response rate, among others.
Spigel added that a consideration for the trial included the comparator arm. “[In] this trial the comparator arm was crizotinib [which is] still used in some parts of the world [but it] is not really used in the United States much at all anymore; [it was] an outstanding drug at its time, but better drugs are available now. With that said, the results with lorlatinib are the best we’ve ever seen. It’s not good to compare studies [with] other studies, we have not had a randomized controlled trial of lorlatinib vs another modern next-generation TKI, but these are among the best [data in this patient population that] we’ve ever seen.”
Further, Solomon noted that time to intracranial progression was longer with lorlatinib compared with crizotinib in the presence or absence of brain metastases. In patients with brain metastases, the median time to intracranial progression was NR (95% CI, NR-NR) in the lorlatinib arm vs 7.2 months (95% CI, 3.7-11.0) in the crizotinib arm (HR, 0.03; 95% CI, 0.01-0.13). The median time to intracranial progression was NR (95% CI, NR-NR) vs 23.9 months (95% CI, 16.4-30.8), respectively, in patients without brain metastases and96% vs 27%, respectively, did not experience intracranial progression at 5 years.
Solomon added that as approximately 25% of patients with ALK-positive NSCLC have brain metastases at baseline, progressive CNS involvement remains a key concern.
“These results speak to the ability of lorlatinib not only to prevent progression of existing brain metastases, but to prevent or delay progression of new brain metastases,” Solomon said. “The systemic efficacy results coupled with prolonged intracranial efficacy from first line lorlatinib treatment indicate that this provides an unprecedented improvement in outcomes for patients with advanced ALK-positive NSCLC.”
Reference
Solomon BJ, Liu G, Felip E, et al. Lorlatinib vs crizotinib in treatment-naïve patients with advanced ALK+ non-small cell lung cancer: 5-year progression-free survival and safety from the CROWN study. J Clin Oncol. 2024;42(suppl 17):LBA8503. doi:10.1200/JCO.2024.42.17_suppl.LBA8503