Lymphoscintigraphy Maps Extra-axillary Nodal Drainage
NEW ORLEANS-Preoperative lymphoscintigraphy can be used to identify women with primary breast cancer who have multidirectional lymphatic drainage. This appears to occur in about 10% of breast cancer patients, who can then have these areas dissected or included in radiation ports.
NEW ORLEANSPreoperative lymphoscintigraphy can be used to identify women with primary breast cancer who have multidirectional lymphatic drainage. This appears to occur in about 10% of breast cancer patients, who can then have these areas dissected or included in radiation ports.
Findings from a large prospective study, funded by the US Department of Defense, were presented at the Society of Surgical Oncology (SSO) Cancer Symposium.
Elizabeth Dupont, MD, of H. Lee Moffitt Cancer Center, Tampa, said that the study included more than 500 breast cancer patients from 41 institutions.
She said that the study was initiated to define the role of preoperative lymphatic mapping combined with intraoperative imaging in identifying extra-axillary drainage.
We sought to identify a subgroup of patients who showed no lymph drainage to the axillae and, therefore, might not require an axillary staging procedure, but we were not reliably able to do so, Dr. Dupont said.
Lymphoscintigraphy has been an important diagnostic tool in melanoma, but has not been used routinely in breast cancer, since most surgeons have been concerned only with mapping to the axillae, she pointed out.
The researchers felt that preoperative lymphoscintigraphy might identify a subset of women with extra-axillary drainage, serve as an adjunct to sentinel lymph node (SLN) biopsy, and provide information about numbers and location of nodes to be harvested.
Preoperative lymphoscintigraphy images were produced using filtered technetium-99 sulfur colloid, and lymphatic drainage to the axillary and internal mammary nodes was noted. Intraoperatively, a hand-held gamma probe was used to identify the sentinel lymph nodes. Most patients then underwent axillary node dissection at levels 1 and 2.
Study Results
Drainage to an axillary sentinel lymph node was found in 336 patients (65%). No axillary nodes were shown preoperatively in 181 patients (35%), who were then taken to the operating room for intraoperative mapping.
At this point, 52 patients (10% of all patients imaged preoperatively) demonstrated an extra-axillary node, such as an internal mammary node; 45 of these patients showed bidirectional drainage to the axillae and internal mammary sites, and 7 drained only to the internal mammary, Dr. Dupont reported.
Although lymphoscintigraphy was unable to identify a sentinel lymph node in 181 patients, 153 (85%) of these patients had an axillary sentinel lymph node identified with intraoperative mapping using the sensitive hand-held gamma probe and vital blue dye.
There were 28 patients who failed to map either preoperatively or intraoperatively, Dr. Dupont said. Thirteen of these patients (47%) were found to have metastatic disease in the axillae upon complete axillary node dissection.
Nearly half of these patients had more than one positive node. Some had extensive positive nodes, such as extranodal extension or, in one case, positivity in all 25 nodes dissected.
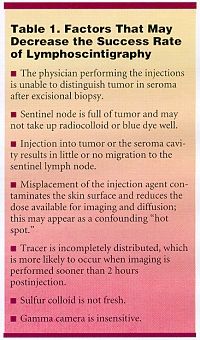
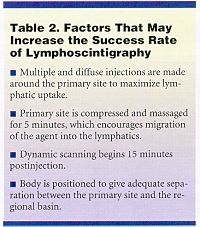
Four of the 13 had palpable tumors, and 6 patients had undergone previous excisional biopsy. In each of these 13 cases, there had been no massage with injection of the imaging agent, which might have improved mapping success, Dr. Dupont said. (See Table 1 for factors that may decrease success and Table 2 for factors that may improve success.)
In the majority of image-negative patients, sentinel lymph nodes were still identified intraoperatively. Patients who had negative imaging and no dye or radiocolloid in the axillae still need level 1 or 2 node dissection, as 47% will have metastatic disease, she said.
Dr. Dupont concluded, We showed through lymphoscintigraphy that drainage is variable
and there may be multiple routes, which is important in decision-making about treatment.
Treatment varied for the subset of patients with multidirectional drainage. Some of our institutions chose to observe nodes; others included them in radiation ports of breast-conserved patients; others removed them, she said. How to best handle this subset needs to be addressed in national trials.
David Craig, MD, of the University of Vermont, commented, This is a large trial, and we have to pay attention to it. Gamma camera imaging identifies extra-axillary nodes, but if you rely solely on the gamma camera, you are going to miss SLNs. However, SLNs not seen by the gamma camera are generally detected by hand-held probes. Our challenge is to apply all of our tools to these new problems.