Rapid Dose Titration With Controlled-Release Oxycodone
MIAMI, Florida-Two separate multicenter trials suggest that dose titration in patients with chronic, moderate to severe pain can be achieved as readily with controlled-release (CR) oral oxyco-done (OxyContin) given once every 12 hours as with an oral intermediate-release (IR) formulation given four times a day.
MIAMI, FloridaTwo separate multicenter trials suggest that dose titration in patients with chronic, moderate to severe pain can be achieved as readily with controlled-release (CR) oral oxyco-done (OxyContin) given once every 12 hours as with an oral intermediate-release (IR) formulation given four times a day.
In one study, 48 patients with cancer pain inadequately controlled by prior analgesic therapy were randomized to open-label titration with either CR or IR oxycodone to a maximum dose of 400 mg/d for a period of up to 21 days. A similar study included 57 patients with low back pain titrated to a maximum dose of 80 mg/d for a period of up to 10 days. The majority of patients in both studies were converted to oxycodone from other opioid analgesics.
Miami physician Robert T. Salzman, MD, reported that, in both studies, there were no significant differences between the two formulations with respect to the percentage of patients achieving stable pain control, the time to achieve stable pain control, and the degree of pain control achieved.
Stable Analgesia
Among the cancer patients, 85% achieved stable analgesia, 92% with the CR formulation and 79% with the IR agent. Nearly 60% of the cancer patients achieved stable pain control with no dose titration, Dr. Salzman said. Further, the majority of patients (68%) did not use a nonopioid analgesic during titration (J Pain Symptom Manage 18:271-279, 1999).
Among the cancer patients, the mean time to stable pain control was 1.6 days for patients receiving CR oxycodone and 1.7 days for those on IR oxycodone. The mean daily doses for the cancer patients who completed the titration period were 104 mg for CR oxycodone and 113 mg for IR oxycodone.
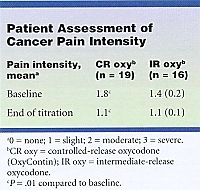
At the end of the titration period, the patients pain assessment diaries showed a slight level of pain in both groups, which met the criteria for stable pain control (see Table).
Patients reported reductions in pain intensity from baseline despite use of prestudy opioid analgesics by the majority, Dr. Salzman noted.
The most commonly reported adverse effects in both studies were similar for the two formulations and were those expected with opioid use: nausea, vomiting, constipation, somnolence, dizziness, and pruritus. Thirteen of the cancer patients discontinued treatment, eight because of ineffective treatment or intercurrent illnesses, three because of adverse events, and two for other reasons.
Many physicians start opioid therapy with an IR formulation, which they titrate to stable pain control before switching to a CR formulation for maintenance therapy, Dr. Salzman said. However, he noted, certain long-acting opioid forms, including CR oxycodone, exhibit a rapid absorption and prompt onset of action that make them suitable for titration.
CR oxycodone is characterized by an initial rapid absorption of 38% of the dose, providing onset of analgesia with 1 hour in most patients, he said. The initial phase is followed by slower absorption of the remaining 62% of the dose for prolonged analgesia duration.
The study was sponsored by Purdue Pharma, Norwalk, Connecticut.
Targeted Therapy First Strategy Reduces Need for Chemotherapy in Newly Diagnosed LBCL
December 7th 2025Lenalidomide, tafasitamab, rituximab, and acalabrutinib alone may allow 57% of patients with newly diagnosed LBCL to receive less than the standard number of chemotherapy cycles without compromising curative potential.