Management of Relapsed Mantle Cell Lymphoma: Still a Treatment Challenge
Mantle cell lymphoma (MCL) is a distinct subtype of non-Hodgkin lymphoma that occurs most commonly in older patients with advanced-stage disease.
Mantle cell lymphoma (MCL) is a distinct subtype of non-Hodgkin lymphoma that remains incurable, and is associated with a median survival of approximately 5 years. Management of patients with relapsed or refractory disease is challenging. The major therapeutic goal in MCL management is to improve survival and quality of life whenever possible. Progress has been made in MCL therapy in the past decade based on clinical experimentation with novel agents and combinations. There is a growing list of conventional and novel agents in our armamentarium, consisting of not only additional chemotherapy combinations including high-dose approaches, but also biologically targeted reagents such as the monoclonal antibody rituximab, the proteasome inhibitor bortezomib, the mTOR inhibitor temsirolimus, immunomodulatory and antiangiogenic agents including thalidomide and lenalidomide, and cyclin-dependent kinase inhibitors, as well as a renewed interest in older compounds such as bendamustine and metronomic regimens. Efficacy evaluations for individual agents and rational combinations are in various stages of development, while treatment selection based on molecular and clinical prognostic scores is yet to be tested. In the absence of evidence demonstrating relative survival advantages of various second-line options, management of relapsed and refractory disease should be individualized. Involvement of a lymphoma center participating in clinical trials of novel MCL treatments is encouraged.
Mantle cell lymphoma (MCL) is a distinct subtype of non-Hodgkin lymphoma that occurs most commonly in older patients with advanced-stage disease. The typical clinical course is characterized by frequent relapse after initial therapy, with a reported median survival of 5 years. Median failure-free survival has been reported as approximately 8 to 20 months with upfront standard therapies such as CHOP-like regimens (cyclophosphamide, doxorubicin HCl, vincristine [Oncovin], prednisone),[1-3] although longer progression-free survival (PFS) has been reported with high-intensity chemotherapy, such as the hyper-CVAD regimen (hyperfractionated cyclophosphamide, vincristine, doxorubicin [Adriamycin], dexamethasone), with or without autologous stem-cell transplantation (ASCT).[4,5] The relative merits of these approaches are difficult to fully appreciate due to the differences in eligible patient populations and limited randomized comparative data.
Management of recurrent disease is an expected yet difficult clinical problem in MCL due to both disease and patient factors. MCL is a relatively uncommon entity that accounts for roughly 5% to 8% of all lymphomas.[6,7] Despite many important therapeutic advances in the past decade, there remains a paucity of evidence demonstrating relative survival advantages of various salvage regimens, partially limited by the low patient numbers and enrollment on clinical studies. Most MCL patients are older, and may be less able to tolerate more aggressive therapy due to age or comorbid illnesses. The major therapeutic goal in MCL management is to extend survival and improve quality of life whenever possible. Thus, an individualized treatment approach should be devised after reviewing options, taking into consideration the clinical characteristics of the disease such as MCL-related symptoms and pace of disease, and the patient’s performance status and preferences, with an emphasis on clinical trial participation.
Treatment Options
A growing list of novel regimens for MCL has been introduced to the clinic in the past 2 decades. In a retrospective survival analysis of two historical patient cohorts followed in Germany 20 years apart, Herrmann and colleagues reported a median overall survival (OS) of 2.7 years for the earlier Kiel Lymphoma Study Group patients as compared with 4.8 years for the contemporary German Low Grade Lymphoma Study Group (GLSG) patients.[8] The longer median overall survival in the later cohort is likely largely due to improvements in therapy, perhaps mostly in the second-line setting, in recent decades. This review will discuss agents and combinations with utility in the recurrent disease setting.
Intensive Chemotherapy-Based Approach
• Second-Line Chemotherapy-For younger patients with aggressive disease, outside of clinical trials there are several commonly employed chemotherapeutic options including R-ICE (rituximab [Rituxan], ifosfamide, carboplatin, etoposide), R-DICE (rituximab, dexamethasone, ifosfamide, cisplatin, etoposide), R-DHAP (rituximab, dexamethasone, high-dose cytarabine [Ara-C], cisplatin [Platinol]), R-ESHAP (rituximab, etoposide, methylprednisolone [SoluMedrol], high-dose cytarabine, cisplatin) or R-hyperCVAD (rituximab, hyperfractionated cyclophosphamide, vincristine, doxorubicin [Adriamycin], dexamethasone, alternating with high-dose methotrexate and cytarabine). Based on clinical factors, including prior treatments and their effect and tolerability, patients who have not received intensive treatment initially sometimes receive high-dose therapy with ASCT. While comparisons are limited, this group as well as those who were previously treated intensively upfront (including stem cell transplant) may also receive chemotherapy followed by allogeneic nonmyeloablative stem cell transplantation (NSCT).
• Hematopoietic Stem Cell Transplantation-Both ASCT and NSCT have been studied in relapsed MCL. Compared with ASCT in first remission, inferior outcomes have generally been reported in the relapsed setting-but treatment responsiveness in any setting is greater upfront vs in recurrence, and no study has randomized patients to early vs late ASCT in MCL. An estimated 4-year disease-free survival of 31% was reported in a Dana-Farber Cancer Center series with 20 relapsed MCL patients receiving purged autologous bone marrow graft.[9] Gopal and colleagues reported apparently more successful outcomes (3-year OS of 93% and PFS of 61%) combining the high-dose iodine-131–labeled anti-CD20 antibody tositumomab (Bexxar) with etoposide and cyclophophamide followed by ASCT.[10]
In a recent report from M.D. Anderson Cancer Center on high-dose therapy from 1990 to 2007, 36 patients (aged 42–76) received ASCT with conditioning regimens including high-dose cyclophosphamide and total-body irradiation (Cy/TBI), R-Cy/TBI and R-BEAM (carmustine [BCNU], etoposide, cytarabine, melphalan), and 35 patients (aged 43–68) received NSCT with conditioning regimens of either PFA (cisplatin, fludarabine, cytarabine) or FCR (fludarabine, cyclophosphamide, rituximab).[11] For the ASCT patients, the median PFS and OS were 27 and 52 months, and transplant-related mortality rates were 8% at 3 months and 1 year. Inclusion of rituximab in the treatment regimen was not associated with an improved outcome. For the NSCT patients, the median PFS duration was 60 months and the median OS has not been reached, with a median follow-up of 56 months. In contrast to the ASCT patients, plateaus in the survival curves were observed for both PFS and OS in nine NSCT patients followed between 63 and 110 months. The transplant-related mortality rates were 0% at 3 months and 9% at 1 year. The actuarial risk of acute graft-vs-host disease (GVHD) was 37%, and chronic GVHD risk was 60%.
Other studies using variations of conditioning regimens have reported variable clinical outcomes, and patient selection is clearly a major factor in results.[12,13] Nevertheless, reduced-intensity allogeneic SCT represents a promising salvage strategy that warrants continued and cautious investigation.
Biologic and Targeted Agents
TABLE 1
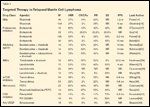
Targeted Therapy in Relapsed Mantle Cell Lymphoma
For many patients with relapsed MCL, intensive salvage and high-dose therapy are not options because of either comorbidities or personal preferences. Several novel compounds have shown meaningful clinical activities as single agents, and in some cases have demonstrated durable disease control when used in rational combinations while preserving quality of life (Table 1). Given the array of options and unanswered questions in this area, we believe that patients with MCL should be encouraged to participate in clinical trials whenever possible.
• Monoclonal Antibody–Based Therapies-Rituximab, a chimeric antibody directed against the CD20 antigen, has been widely employed in B-cell malignancies. In mantle cell lymphoma, the standard regimen of four weekly infusions of 375 mg/m2/wk has been demonstrated to have modest activity, with an overall response rate (ORR) of 37% in the relapsed setting, and a median duration of response of 1.2 years.[14] Ghielmini and colleagues reported that prolonged treatment with rituximab did not significantly improve response rate, duration of response, or event-free survival after induction with rituximab alone.[15]
Other results from a randomized study by the GLSG showed that maintenance rituximab led to a statistically significant prolongation of response duration after second-line therapy with R-FCM (rituximab, fludarabine, cyclophosphamide, mitoxantrone; P = .049).[16] After a median observation of 26 months, median response duration was slightly prolonged by rituximab maintenance (14 vs 12 months) but with a significantly higher proportion of patients with ongoing remission beyond 2 years (45% vs 9%). The bottom line is that rituximab is commonly included in MCL treatment regimens, but its impact as a single agent, in combinations, and for maintenance seems to be more limited than that in other lymphoma histologies.
REFERENCE GUIDE
Therapeutic Agents
Mentioned in This Article
Bevacizumab (Avastin)
Bortezomib (Velcade)
Carboplatin
Carmustine (BCNU)
Cisplatin
Cyclophosphamide
Cytarabine
Dexamethasone
Doxorubicin
Etoposide
Flavopiridol
Fludarabine
Ifosfamide
Lenalidomide (Revlimid)
Melphalan
Methotrexate
Mitoxantrone
Prednisone
Procarbazine (Matulane)
Rituximab (Rituxan)
Temsirolimus (Torisel)
Thalidomide (Thalomid)
Tositumomab/
131
I-tositumomab (Bexxar)
Vincristine
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
• Bortezomib-Bortezomib (Velcade), a dipeptidyl boronic acid derivative, selectively inhibits the 26S proteasome, which is essential in the degradation of intracellular proteins including p53, nuclear factor kappa B (NFB), bcl-2, and cyclin-dependent kinase (CDK) inhibitors such as p21 and p27. Inhibition of the ubiquitin-proteasome pathway in tumor cells in part hinders tumor growth by inducing cell-cycle arrest, apoptosis, and inhibition of tumor metastasis and angiogenesis.
Results from multiple phase II reports demonstrate that bortezomib is an active agent in relapsed and refractory mantle cell lymphoma, producing ORRs of 33% to 50%, and complete response (CR) rates of 4% to 8%.[17-20] When given at 1.3 mg/m2 on days 1, 4, 8, and 11 of a 21-day cycle, bortezomib demonstrated an ORR of 33%, including 8% CR/unconfirmed CR, with a median duration of response of 9.2 months and time to progression of 6.2 months in a multicenter pivotal phase II trial, leading to US Food and Drug Administration (FDA) approval of bortezomib for this indication.[19] The most common grade 3/4 adverse events were peripheral neuropathy, fatigue, and thrombocytopenia. Currently, multiple trials are ongoing to further examine the efficacy of bortezomib either as a single agent or in combination with other active regimens including rituximab or CHOP plus rituximab (R-CHOP) in non-Hodgkin lymphoma.
• Bendamustine-Bendamustine is a novel agent consisting of a mechlorethamine group, a benzimidazole ring, and a butyric acid side chain. Bendamustine causes direct DNA damage and apoptosis, inhibition of mitotic checkpoints, and induction of mitotic catastrophe.[21] Phase II studies of the combination of rituximab plus bendamustine have shown marked clinical responses. Bendamustine was given at a dose of 90 mg/m2 on days 1 and 2, combined with rituximab at 375 mg/m2 on day 1, given every 4 weeks for a maximum of four cycles.
Rummel and colleagues reported an ORR of 75% with a CR rate of 50% in 16 patients with recurrent MCL.[22] The median PFS for MCL patients was 18 months. A recent international phase II study included 12 patients with MCL. Rituximab was administered on day 1, and bendamustine on days 2 and 3 of each 28-day cycle for a total of 4-6 cycles. An additional dose of rituximab was administered 1 week before the first cycle and 4 weeks after the last cycle. The investigators reported an ORR of 92%, CR of 42%, and CRu of 17% for the MCL patients, with a median duration of response of 19 months.[23] Similar clinical activities were reported for the combination of bendamustine with mitoxantrone and rituximab.[24] In general, bendamustine regimens were well tolerated, with primary toxicities of myelosuppression including grade 3/4 neutropenia and thrombocytopenia.
• IMiDs-Immunomodulatory drugs (IMiDs) are a series of synthetic compounds that have been developed based on the glutamate-derivative backbone of the prototype drug thalidomide (Thalomid). Thalidomide has wide-ranging functions including anti-inflammatory, immunomodulatory, antiangiogenic, and direct anticancer activities.[25] The second-generation compound lenalidomide (Revlimid) has enhanced immunologic and anticancer properties with fewer side effects.
Drach and colleagues have reported clinical activity of thalidomide and rituximab in a small clinical study for patients with relapsed/refractory MCL.[26] Of 16 evaluable subjects, 13 demonstrated objective responses (5 CR, 8 partial response [PR], ORR of 81%, and CR rate of 31%) while taking thalidomide at 200 to 400 mg daily in combination with rituximab, with median time to progression at 20 months. The main toxicities of thalidomide include fatigue, somnolence, neuropathy and thromboembolic events.
Lenalidomide has demonstrated significant clinical activity either as a single agent or in combination with rituximab in MCL. Single-agent lenalidomide given at 25 mg orally daily on days 1 to 21 every 28 days in relapsed aggressive lymphoma subtypes demonstrated an ORR of 35%, including 53% ORR for 15 MCL patients.[27] An international study of lenalidomide in aggressive non-Hodgkin lymphoma subtypes by Czuczman and colleagues reported a 28% ORR, with 36% ORR for 22 MCL patients, and identified low tumor burden and longer duration from prior rituximab as two favorable predictive factors.[28]
Wang and colleagues explored the combination of lenalidomide and rituximab in a phase I/II study in patients with relapsed/refractory MCL.[29] At a 20-mg daily dose of lenalidomide (on days 1–21 of a 28-day cycle), five out of six patients achieved responses including one CR, one PR, and one case of progressive disease, following two cycles of treatment. Longer follow-up with additional patients will be of interest. Fatigue and myelosuppression with thrombocytopenia and neutropenia are the most common adverse effects of lenalidomide therapy. Coleman and colleagues from our center have reported preliminary clinical experience on the THRIL regimen, which includes alternating daily thalidomide at 50 mg with lenalidomide at 10 mg on a continuous basis in combination with maintenance rituximab every 6 months to minimize cytopenias. In three patients with MCL, two achieved CR and one PR.[30]
• mTOR Inhibitor Temsirolimus-The mammalian target of rapamycin (mTOR) is a serine/threonine kinase downstream of the PI3-kinase/AKT pathway.[31] mTOR-mediated phosphorylation activates downstream targets that are essential in the regulation of cell growth, proliferation, and survival.[32] Selective mTOR inhibitors have shown antiangiogenic activities by inhibiting hypoxia-inducible factor (HIF)-1–mediated vascular endothelial growth factor (VEGF) production downstream of the PI3-kinase/AKT/mTOR pathway, as well as a direct inhibitory effect on endothelial cell proliferation.[33,34]
Witzig and colleagues reported the first phase II trial of the mTOR inhibitor temsirolimus (CCI-779, Torisel) in patients with relapsed mantle cell lymphoma. Temsirolimus was given at 250 mg intravenously every week as a single agent. A 38% response rate was observed in 34 evaluable patients, with a median time to progression of 6.5 months. Thrombocytopenia was dose-limiting, but of short duration.[35] A subsequent randomized, open-label phase III study compared the antitumor activity of temsirolimus with an investigator’s choice of therapy in patients with relapsed MCL. Patients were randomly assigned to one of two schedules of IV temsirolimus, 175 mg three times weekly followed by either 75 mg (175/75 mg) or 25 mg (175/25 mg) weekly, or the investigator’s choice of therapy. Treatment with the temsirolimus 175/75 mg arm resulted in significant improvement in PFS (4.8 months vs 1.9 months, P = .0009), objective response rate (22% vs 2%, P = .0019), and a trend toward longer OS (10.9 months vs 5.8 months, P = .0714), compared with the investigator’s choice. The most common grade 3/4 adverse events were cytopenias.[36]
Metronomic Therapy
Case Report: A Man With a Cecal Mass
Mr. D. is a 70-year-old man who was initially diagnosed with mantle cell lymphoma after presenting with gastrointestinal complaint and lethargy. A colonoscopy revealed a 6-cm cecal mass. Staging workup was consistent with stage IV disease. He was initially treated with six cycles of R-CHOP chemotherapy and achieved an overall partial response. Six months later, he began to have worsening abdominal bloating, and scan documented progression of disease. He was treated with bortezomib at 1.3 mg/m
2
for three cycles and achieved stable disease.
The patient now presents with a 10-cm cecal mass which is causing significant abdominal discomfort. Mr. D. runs a small business, and prefers the therapy that would take the least amount of time from work.
What are the salvage therapy options for this patient?
(1) Salvage chemotherapy followed by autologous stem cell transplant for consolidation
(2) Debulking surgery to relieve impending bowel obstruction, followed by systemic therapy
(3) Participation in a clinical study
Indeed, any of the above options could be considered, depending on the patient’s comorbidity and preference. The authors would recommend participation in a clinical trial. In fact, the patient had the large cecal mass removed, and enrolled in a phase II clinical study that combines metronomic therapy of PEPC (prednisone, etoposide, procarbazine, and cyclophosphamide) with thalidomide and rituximab. He achieved a complete response, and has been in remission for 4 years, enjoying excellent quality of life.
Metronomic chemotherapy refers to the administration of low doses of medications on a frequent or continuous schedule without extended drug-free breaks. The main targets of metronomic therapy are the endothelial cells of the growing tumor vasculature.[37] An effective, convenient, and well-tolerated therapy in relapsed MCL that has been used by our group is the PEPC (C3) regimen.[38] PEPC consists of low-dose prednisone (20 mg), etoposide (50 mg), procarbazine (Matulane, 50 mg), and cyclophosphamide (50 mg) administered orally, with dosing frequency titrated to hematologic parameters (ie, absolute neutrophil count > 1,000/µL). In 22 patients with relapsed MCL, an ORR of 82% and a CR of 46% were observed with this regimen.
We have further combined the PEPC regimen with two agents that are active against MCL-rituximab and thalidomide[39]-to comprise the RT-PEPC regimen, in order to further improve the therapeutic index of metronomic therapy for relapsed/refractory MCL in an ongoing study.[40]
Other Novel Agents
• Cyclin-Dependent Kinase Inhibitors-The overexpression of cyclin D1 in mantle-cell lymphoma makes cell-cycle inhibition an attractive therapeutic target. Flavopiridol, a synthetic N-methylpiperidinyl, chlorophenyl flavone compound, can induce cell-cycle arrest by direct inhibition of CDKs. Modest activity was observed for single-agent flavopiridol in a phase II study, which demonstrated an 11% PR rate, 71% stable disease rate, and a median duration of response of 3.3 months.[41] Other doses, schedules, and combinations of flavopiridol are under active investigation by several groups.
A pilot study of PD 0332991, a specific and potent CDK4/6 inhibitor, also showed modest activity as a single agent in relapsed MCL (50% stable disease in 16 patients),[42] while clearly demonstrating inhibitory effects on cell-cycle pathways in translational assays. Additional studies of other CDKs with rational dosing schedules and in combination with agents with potentially synergistic activities are ongoing.
• Anti-VEGF Agents-Stopeck and the Southwest Oncology Group (SWOG) reported prolonged stabilization of disease in a significant subset (25%) of patients with relapsed aggressive NHL subtypes (including 15 patients with relapsed MCL) treated with single-agent bevacizumab (Avastin) at 10 mg/kg every 2 weeks on the SWOG S0108 study.[43] Combinations with chemoimmunotherapy such as R-CHOP and other antiangiogenic compounds are in various stages of clinical development.
Recommendations
MCL is recognized as one of the most challenging forms of lymphoma, with emergence of resistance to chemotherapy and a relatively rapid clinical progression in the majority of cases. Traditional CHOP-based chemotherapy affords moderate response rates, but relapse is expected within 1 to 3 years. Addition of the monoclonal anti-CD20 antibody rituximab improves response rates; however, the benefit cannot clearly be translated into a progression-free or overall survival advantage. More intensive regimens such as hyper-CVAD are largely prohibitive for many patients because of treatment-related toxicities, although in selected patients, rates of complete response and time to progression appear superior to those achieved with other regimens. Whether this regimen and/or autologous stem cell transplant improve overall survival remains debatable. For most MCL patients, recurrent/resistant disease is ultimately expected, and further strategies are needed.
Management of relapsed disease is a challenging task that requires a thoughtful and individualized approach. The good news is that we are providing our MCL patients with improved therapeutic and supportive care regimens, which will likely translate into better overall survival. Importantly, we now have a growing list of biologic agents that target tumor cells and the tumor microenvironment in various stages of clinical development and maturity. Rational application of these compounds, either alone or in combination, has brought about durable disease control with minimal toxicities in selected MCL patients. Particularly promising regimens include the bendamustine/rituximab combination, bortezomib, lenalidomide, temsirolimus, and schedules based on metronomic therapy.
Limitations are the lack of clear evidence demonstrating relative survival advantages of various treatments, and the lack of routinely available clinicopathologic biomarkers to guide selection of a particular regimen.
In our practice, we have adapted an individualized treatment strategy by placing great emphasis on clinical trial participation. Without an available suitable clinical study, treatment can be chosen based on the clinical setting. For patients with extensive, rapidly progressive disease, a chemotherapy-based approach is appropriate in order to achieve a rapid response. After response is achieved, depending on previous treatments, expectations regarding response durability, and comorbid illnesses, stem cell transplant options may be considered. Generally speaking, allogeneic approaches seem to have greater potential than autologous options in the relapsed setting. In our experience, for many patients who are elderly or have comorbidities, less aggressive approaches are more appropriate in relapse. These patients typically cycle through the array of lower-intensity options, including metronomic approaches and novel biologic agents, with the choice in part based on the goal of achieving meaningful disease control and preservation of quality of life. While these clinical situations always require time and thoughtful consideration, there is reason for optimism that the availability of new approaches will further improve outcomes for MCL patients in the coming years.
Financial Disclosure: Dr. Ruan has received research support from Genentech and Sigma-Tau. Dr. Leonard has received research support and/or served as a consultant for Genentech, Celgene, Millenium, Cephalon, Novartis, and Sigma-Tau.
References:
1. Fisher RI, Dahlberg S, Nathwani BN, et al: A clinical analysis of two indolent lymphoma entities: Mantle cell lymphoma and marginal zone lymphoma (including the mucosa-associated lymphoid tissue and monocytoid B-cell subcategories): A Southwest Oncology Group study. Blood 85:1075-1082, 1995.
2. Howard OM, Gribben JG, Neuberg DS, et al: Rituximab and CHOP induction therapy for newly diagnosed mantle-cell lymphoma: Molecular complete responses are not predictive of progression-free survival. J Clin Oncol 20:1288-1294, 2002.
3. Lenz G, Dreyling M, Hoster E, et al: Immunochemotherapy with rituximab and cyclophosphamide, doxorubicin, vincristine, and prednisone significantly improves response and time to treatment failure, but not long-term outcome in patients with previously untreated mantle cell lymphoma: Results of a prospective randomized trial of the German Low Grade Lymphoma Study Group (GLSG). J Clin Oncol 23:1984-1992, 2005.
4. Romaguera J, Fayad L, Rodriguez MA, et al: Rituximab plus hypercvad (R-HCVAD) alternating with rituximab plus high-dose methotrexate-cytarabine (R-M/A) in untreated mantle cell lymphoma (MCL): prolonged follow-up confirms high rates of failure-free survival (FFS) and overall survival (OS) (abstract 128). Blood 104, 2004.
5. Dreyling M, Lenz G, Hoster E, et al: Early consolidation by myeloablative radiochemotherapy followed by autologous stem cell transplantation in first remission significantly prolongs progression-free survival in mantle-cell lymphoma: Results of a prospective randomized trial of the European MCL networks. Blood 105:2677-2684, 2005.
6. Weisenburger DD, Armitage JO: Mantle cell lymphoma-an entity comes of age. Blood 87:4483-4494, 1996.
7. Morton LM, Wang SS, Devesa SS, et al: Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood 107:265-276, 2006.
8. Herrmann A, Hoster E, Zwingers T, et al: Improvement of overall survival in advanced stage mantle cell lymphoma. J Clin Oncol 27:511-518, 2009.
9. Freedman AS, Neuberg D, Gribben JG, et al: High-dose chemoradiotherapy and anti-B-cell monoclonal antibody-purged autologous bone marrow transplantation in mantle-cell lymphoma: no evidence for long-term remission. J Clin Oncol 16:13-18, 1998.
10. Gopal AK, Rajendran JG, Petersdorf SH, et al: High-dose chemo-radioimmunotherapy with autologous stem cell support for relapsed mantle cell lymphoma. Blood 99:3158-3162, 2002.
11. Tam CS, Bassett R, Ledesma C, et al: Mature results of the MD Anderson Cancer Center risk-adapted transplantation strategy in mantle cell lymphoma. Blood 113:4144-4152, 2009.
12. Maris MB, Sandmaier BM, Storer BE, et al: Allogeneic hematopoietic cell transplantation after fludarabine and 2 Gy total body irradiation for relapsed and refractory mantle cell lymphoma. Blood 104:3535-3542, 2004.
13. Morris E, Thomson K, Craddock C, et al: Outcomes after alemtuzumab-containing reduced-intensity allogeneic transplantation regimen for relapsed and refractory non-Hodgkin’s lymphoma. Blood 104:3865-3871, 2004.
14. Foran JM, Rohatiner AZ, Cunningham D, et al: European phase II study of rituximab (chimeric anti-CD20 monoclonal antibody) for patients with newly diagnosed mantle-cell lymphoma and previously treated mantle-cell lymphoma, immunocytoma, and small B-cell lymphocytic lymphoma. J Clin Oncol 18:317-324, 2000.
15. Ghielmini M, Schmitz SF, Cogliatti S, et al: Effect of single-agent rituximab given at the standard schedule or as prolonged treatment in patients with mantle cell lymphoma: A study of the Swiss Group for Clinical Cancer Research (SAKK). J Clin Oncol 23:705-711, 2005.
16. Forstpointner R, Unterhalt M, Dreyling M, et al: Maintenance therapy with rituximab leads to significant prolongation of response duration after salvage therapy with a combination of rituximab, fludarabine, cyclophosphamide, and mitoxantrone (R-FCM) in patients with recurring and refractory follicular and mantle cell lymphomas: Results of a prospective randomized study of the German Low Grade Lymphoma Study Group (GLSG). Blood 108:4003-4008, 2006.
17. O’Connor OA, Wright J, Moskowitz C, et al: Phase II clinical experience with the novel proteasome inhibitor bortezomib in patients with indolent non-Hodgkin’s lymphoma and mantle cell lymphoma. J Clin Oncol 23:676-684, 2005.
18. Goy A, Younes A, McLaughlin P, et al: Phase II study of proteasome inhibitor bortezomib in relapsed or refractory B-cell non-Hodgkin’s lymphoma. J Clin Oncol 23:667-675, 2005.
19. Fisher RI, Bernstein SH, Kahl BS, et al: Multicenter phase II study of bortezomib in patients with relapsed or refractory mantle cell lymphoma. J Clin Oncol 24:4867-4874, 2006.
20. Belch A, Kouroukis CT, Crump M, et al: A phase II study of bortezomib in mantle cell lymphoma: the National Cancer Institute of Canada Clinical Trials Group trial IND.150. Ann Oncol 18:116-121, 2007.
21. Leoni LM, Bailey B, Reifert J, et al: Bendamustine (Treanda) displays a distinct pattern of cytotoxicity and unique mechanistic features compared with other alkylating agents. Clin Cancer Res 14:309-317, 2008.
22. Rummel MJ, Al-Batran SE, Kim S-Z, et al: Bendamustine plus rituximab is effective and has a favorable toxicity profile in the treatment of mantle cell and low-grade non-Hodgkin’s lymphoma. J Clin Oncol 23:3383-3389, 2005.
23. Robinson KS, Williams ME, van der Jagt RH, et al: Phase II multicenter study of bendamustine plus rituximab in patients with relapsed indolent B-cell and mantle cell non-Hodgkin’s lymphoma. J Clin Oncol 26:4473-4479, 2008.
24. Weide R, Hess G, Koppler H, et al: High anti-lymphoma activity of bendamustine/mitoxantrone/rituximab in rituximab pretreated relapsed or refractory indolent lymphomas and mantle cell lymphomas. A multi-center phase II study of the German Low Grade Lymphoma Study Group (GLSG). Leuk Lymphoma 48:1299-1306, 2007.
25. Bartlett JB, Dredge K, Dalgleish AG: The evolution of thalidomide and its IMiD derivatives as anticancer agents. Nat Rev Cancer 4:314-322, 2004.
26. Drach J, Kaufmann H, Puespoek A, et al: Marked anti-tumor activity of rituximab plus thalidomide in patients with relapsed/resistant mantle cell lymphoma (abstract 606). Blood 100:162a, 2002.
27. Wiernik PH, Lossos IS, Tuscano JM, et al: Lenalidomide monotherapy in relapsed or refractory aggressive non-Hodgkin’s lymphoma. J Clin Oncol 26:4952-4957, 2008.
28. Czuczman MS, Reeder CB, Polikoff J, et al: International study of lenalidomide in relapsed/refractory aggressive non-Hodgkin’s lymphoma (abstract 8509). J Clin Oncol 26(15S):456s, 2008.
29. Wang M, Fayad L, Hagemeister F, et al: A phase I/II study of lenalidomide (Len) in combination with rituximab (R) in relapsed/refractory mantle cell lymphoma (MCL) with early evidence of efficacy (abstract 8030). J Clin Oncol 25(18S):448s, 2007.
30. Coleman M, Martin P, Ruan J, et al: The THRIL (thalidomide, rituximab, and lenalidomide) regimen for chronic lymphocytic leukemias, small lymphocytic lymphoma, and mantle cell lymphoma: daily alternating IMiDs and rituximab maintenance (abstract 7079). J Clin Oncol 26(15S):391s, 2008.
31. Bjornsti MA, Houghton PJ: The TOR pathway: A target for cancer therapy. Nat Rev Cancer 4:335-348, 2004.
32. Witzig TE, Kaufmann SH: Inhibition of the phosphatidylinositol 3-kinase/mammalian target of rapamycin pathway in hematologic malignancies. Curr Treat Options Oncol 7:285-294, 2006.
33. Mayerhofer M, Valent P, Sperr WR, et al: BCR/ABL induces expression of vascular endothelial growth factor and its transcriptional activator, hypoxia inducible factor-1alpha, through a pathway involving phosphoinositide 3-kinase and the mammalian target of rapamycin. Blood 100:3767-3775, 2002.
34. Guba M, von Breitenbuch P, Steinbauer M, et al: Rapamycin inhibits primary and metastatic tumor growth by antiangiogenesis: Involvement of vascular endothelial growth factor. Nat Med 8:128-135, 2002.
35. Witzig TE, Geyer SM, Ghobrial I, et al: Phase II trial of single-agent temsirolimus (CCI-779) for relapsed mantle cell lymphoma. J Clin Oncol 23:5347-5356, 2005.
36. Hess G, Romaguera JE, Verhoef G, et al: Phase III study of patients with relapsed, refractory mantle cell lymphoma treated with temsirolimus compared with investigator’s choice (abstract 8513). J Clin Oncol 26(15S):457s, 2008.
37. Bertolini F, Paul S, Mancuso P, et al: Maximum tolerable dose and low-dose metronomic chemotherapy have opposite effects on the mobilization and viability of circulating endothelial progenitor cells. Cancer Res 63:4342-4346, 2003.
38. Coleman M, Martin P, Ruan J, et al: Low-dose metronomic, multidrug therapy with the PEP-C oral combination chemotherapy regimen for mantle cell lymphoma. Leuk Lymphoma 49:447-450, 2008.
39. Kaufmann H, Raderer M, Wohrer S, et al: Antitumor activity of rituximab plus thalidomide in patients with relapsed/refractory mantle cell lymphoma. Blood 104:2269-2271, 2004.
40. Ruan J, Coleman M, Furman RR, et al: Targeting angiogenesis in mantle cell lymphoma: clinical efficacy and correlative studies of a phase II trial of RT-PEPC (rituximab, thalidomide and metronomic oral chemotherapy with prednisone, etoposide, procarbazine and cyclophosphamide) in relapsed/refractory disease (abstract 2751). Blood 108(11), 2006.
41. Kouroukis CT, Belch A, Crump M, et al: Flavopiridol in untreated or relapsed mantle-cell lymphoma: Results of a phase II study of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 21:1740-1745, 2003.
42. Leonard JP, LaCasce A, Smith MR, et al: Cdk4/6 inhibitor PD0332991 demonstrates cell cycle inhibition via FLT-PET imaging and tissue analysis in patients with recurrent mantle cell lymphoma (abstract 264). Blood 112(11), 2008.
43. Stopeck AT, Unger JM, Rimxza LM, et al: A phase II trial of single agent bevacizumab in patients with relapsed, aggressive non-Hodgkin lymphoma: Southwest Oncology Group study S0108. Leuk Lymphoma 50:728-735, 2009.