Supraclavicular Extraskeletal Myxoid Chondrosarcoma Presenting With a Sensorimotor Polyneuropathy Associated With Anti-Hu Antibodies
This case shows the importance of searching for antineural antibodies in oncologic patients with new neurologic deficits, and of having a judicious workup for occult malignancies in patients with known antineural antibodies.
ABSTRACT: Extraskeletal myxoid chondrosarcomas usually arise deep in the proximal extremities and limb girdles. Patients with this type of sarcoma have high rates of local recurrence and metastases, but do not typically have paraneoplastic syndromes. We report an unusual case of a 49-year-old man with anti-Hu syndrome in the setting of an extraskeletal myxoid chondrosarcoma. This case shows the importance of searching for antineural antibodies in oncologic patients with new neurologic deficits, and of having a judicious workup for occult malignancies in patients with known antineural antibodies.
Extraskeletal myxoid chondrosarcoma (EMC) is a rare tumor, representing less than 2.5% of soft-tissue sarcomas. EMC typically presents in the 5th or 6th decades of life; a male predominance is reported. Tumors are typically located in the proximal limbs.[1-3]
We report the case of a patient with EMC of the left supraclavicular fossa associated with anti-Hu antibodies, causing a generalized, mixed, axonal-demyelinating, but predominantly axonal, sensory-motor polyneuropathy.
Case Report
A 49-year-old man presented for further workup of a 7-cm left supraclavicular mass thought to be an extragonadal seminoma based on a fine-needle aspiration biopsy. The patient’s medical history was significant for basal cell carcinoma of the nose. His social history was pertinent for a recent trip to China. The patient reported self-resolving flu-like symptoms while in Asia, followed by hypesthesia localized to his abdomen. Later he developed bilateral hand paresthesias and impaired hand dexterity. Three days prior to admission, he developed paresthesias in both legs, most prominently below the knees, leading to an unsteady gait. He also complained of blurry vision, severe fatigue, and lightheadedness when arising.
Evaluation
FIGURE 1

Symmetrical Mydriasis-
Dilation of the pupils was noted in both eyes.
On physical exam the patient was orthostatic. Pupillary examination revealed symmetrical mydriasis (Figure 1), but decreased light reflex on the left only. Extraocular movements were intact bilaterally. The patient had decreased pinprick reaction throughout the trunk and limbs, and decreased vibration and joint position sensation of the fingers and toes. He also had a pinprick sensory level below T6 on the right, and T10–11 on the left. Joint position sensation was impaired, and areflexia and ataxia were noted. No motor strength deficits were seen at the time. One week after admission, the patient developed worsened sensory ataxia and loss of independent ambulation.
Cerebrospinal fluid (CSF) evaluation was notable for normal glucose, 101 erythrocytes, and 15 leukocytes/mm3 with lymphocytic predominance, and a protein content of 234 mg/dL (normal range, 12–60 mg/dL). CSF lyme polymerase chain reaction was negative. Electrophoretic analysis was suggestive of a monoclonal gammopathy. Serum immunofixation and electrophoresis showed an IgG lambda M-protein, but bone marrow biopsy was normal. Serum antibodies including anti-GQ1b, anti-GD1a, anti-GD1b, anti-GM1, Mycoplasma pneumoniae IgM and IgG, Campylobacter jejunii, Cytomegalovirus (CMV), and Epstein-Barr virus (EBV) IgM were all negative. However, CMV and EBV IgG titers were positive. The anti-Hu antibody titer that had been sent during the initial evaluation, returned positive at > 1:640 by Western Blot. Electromyography (EMG) showed evidence of a mild to moderate, multifocal, mixed but predominantly axonal sensorimotor polyneuropathy. A nerve conduction study (NCS) showed low sensory response amplitudes in the arms with sparing of distal legs consistent with Miller-Fisher syndrome. Chest computerized tomography revealed a large, centrally necrotic mass in the left supraclavicular fossa (Figure 2).
FIGURE 2
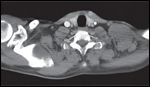
Computed Tomography of the Chest With Intravenous Contrast-
Large, centrally necrotic mass extending from the supraclavicular fossa toward the axilla, to the level of the lateral second and third ribs with adjacent adenopathy.
Magnetic resonance imaging of the cervical and thoracic spine and brain were unremarkable. In view of the fact that serum beta–human chorionic gonadotropin and alpha-fetoprotein levels were normal, surgical biopsy of the mass was performed.
Treatment
The patient was treated with intravenous immunoglobulins (IVIG) at 0.4 g/kg/d for 5 days without clinical response. Because of the rapidly deteriorating neurologic status, it was decided to start chemotherapy using etoposide at 165 mg/m2 and cisplatin at 50 mg/m2 for presumed extragonadal seminoma, followed by 2 additional days of IVIG.
Two weeks after admission orthostasis improved, but the patient had worsened hand incoordination. Both pupils were now unreactive to light and accommodation. He experienced mild pseudoathetosis of the arms, dysmetria in all four extremities, areflexia, moderate vibration loss of wrists and ankles, and impaired proprioception in the metacarpophalangeal joints, ankles, fingertips, and toes.
Repeat EMG showed an acquired predominantly demyelinating sensorimotor polyneuropathy of mild to moderate severity. Compared to the prior NCS, there was progression in loss of sensory responses and further slowing of motor conduction velocities in the arms and legs, suggesting progression of polyneuropathy and favoring a demyelinating form. Electrophysiology was not typical of a sensory neuropathy in view of motor nerve slowing.
After the single cycle of chemotherapy, the pathology report from the surgical biopsy was consistent with a high-grade EMC. The patient underwent en bloc resection of the supraclavicular mass with intraoperative radiation to a dose of 1,000 cGy. The final surgical pathology report confirmed a high-grade malignant neoplasm with a variegated morphologic appearance, large areas of solid, undifferentiated, small, blue round cell morphology, an anaplastic rhabdoid component, and myxoid areas. Most of the tumor showed a uniform cytomorphology, as well as positivity with synaptophysin and chromogranin suggestive of focal neuroendocrine differentiation. Presence of diffuse Fli1 reactivity was also detected, as well as reactivity for vimentin and Bcl-2. Anti-Hu antibody was strongly and diffusely positive (mainly cytoplasmic and focally nuclear). Florescence in situ hybridization for t(9;22)(q22;q12) was positive in the tumor, confirming the diagnosis of EMC.
After surgery, the patient was transferred to an acute rehabilitation service. The patient continued to receive IVIG to complete a total of five courses. He was started on tacrolimus (Prograf, 0.15 mg/kg/d), based on an experimental protocol from Rockefeller University.[4] He also received adjuvant external-beam radiation therapy at a dose totaling 5,400 cGy.
Follow-up
Repeat NCS after 3 months of tacrolimus revealed mild worsening of the sensorimotor polyneuropathy with further reduction of motor response amplitudes in the right leg and further generalized motor conduction slowing. The one hint of improvement was resolution of fibrillations in the right biceps muscle. Sensory response amplitudes remained absent, suggesting marked persistent sensory axon loss throughout. With physical therapy, the patient regained some functional improvement, but he still exhibited severe loss of joint sensation and muscle wasting, and complained of intermittent shooting pains in the hands and legs.
Discussion
This is a case of a rare malignancy arising in an unusual location and presenting with an anti-Hu antibody–related neurologic paraneoplastic syndrome. Our search of the literature revealed only one other case of myxoid chondrosarcoma associated with anti-Hu antibodies.[5]
Histopathologically, EMC has a multilobular or nodular configuration with well-defined margins, a fibrous capsule, and a 6- to 13-cm diameter.[2] The most common chromosomal aberrancy found in EMC is t(9;22)(q22;q12), resulting in fusion of the EWSR1 gene (located at 22q12) to the NR4A3 gene (located at 9q22).[2,6] Immunohistochemical features of EMC include reactivity for vimentin, synaptophysin, and S-100 protein.[1,6] Patients with EMC have 5-, 10-, and 15-year survival rates reported as 82%, 65%, and 58%, respectively.[7] These patients frequently endure local recurrences and metastasis.
Paraneoplastic neurologic disorders are the indirect, antibody-mediated effects of cancer on the nervous system.[8] They may present as classic syndromes, or less frequently as nonspecific neurologic complaints.[9] Anti-Hu is one of these antibodies, described mostly in patients with small-cell lung cancer.[10]
Its presence is useful diagnostically but not for disease monitoring, as there seems to be a lack of correlation between antibody titers and anticancer treatment or neurologic improvement.[11] It has been associated with paraneoplastic encephalomyelitis, paraneoplastic neuronopathy, cerebellar ataxia, limbic encephalitis, isolated autonomic dysfunction, progressive dysautonomia, and pupillary or oculomotor impairments.[12-16]
The immune mechanism by which the anti-Hu antibody precipitates the Hu syndrome remains unclear. Despite the high failure rate of therapies targeting the humoral immune response, an uncontrolled trial of rituximab (Rituxan) reported improvement in 3 of 9 patients with paraneoplastic neurologic disorders.[17] On the other hand, the presence of oligoclonal cytotoxic T-cell infiltrates in the brains and tumors of patients with anti-Hu–associated encephalomyelitis suggests that it might be mediated by T-cell immune responses that are probably directed against the target antigen of the accompanying antibody.[18] Such a presumption implies that medications such as tacrolimus might play a therapeutic role in the management of this disease.[19] Trials to define a protocol for tacrolimus are ongoing, and research suggests that tacrolimus might downregulate cdr2-specific T cells in patients with paraneoplastic cerebellar degeneration.[20]
The Hu syndrome may have a variety of presentations and resemble other neurologic entities, making its diagnosis cumbersome and misleading. This case exemplifies the importance of considering a search for antineural antibodies in cancer patients with new neurologic deficits. In addition, the immunohistochemical identification of the anti-Hu antibody within this patient’s tumor stresses the importance of having a judicious workup for occult malignancies in patients with documented antineural antibodies.
Financial Disclosure: The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Goh YW, Spagnolo DV, Platten M, et al: Extraskeletal myxoid chondrosarcoma: A light microscopic, immunohistochemical, ultrastructural and immuno-ultrastructural study indicating neuroendocrine differentiation. Histopathology 39:514-524, 2001.
2. Hisaoka M, Hashimoto H: Extraskeletal myxoid chondrosarcoma: Updated clinicopathological and molecular genetic characteristics. Pathol Int 55:453â463, 2005.
3. Tsuneyoshi M, Enjoji M, Iwasaki H, et al: Extraskeletal myxoid chondrosarcoma: A clinicopathological and electron microscopic study. Acta Pathol Jpn 31:439-447, 1981.
4. Darnell R: Immunotherapy of the paraneoplastic syndromes. Study ID: RDA-0572-0406. ClinicalTrials.gov identifier: NCT00378326. Available at http://www.ClinicalTrials.gov. Accessed August 15, 2008.
5. VerscHu uren J, Twijnstra A, De Baets M, et al: Hu antigens and anti-Hu antibodies in a patient with myxoid chondrosarcoma. Neurology 44:1551-1552, 1994.
6. Oliveira AM, Sebo TJ, McGrory JE, et al: Extraskeletal myxoid chondrosarcoma: A clinicopathologic, immunohistochemical, and ploidy analysis of 23 cases. Mod Pathol 13:900-908, 2000.
7. Drilon AD, Popat S, BHu char G, et al: Extraskeletal myxoid chondrosarcoma: A retrospective review from 2 referral centers emphasizing long-term outcomes with surgery and chemotherapy. Cancer Oct 24, 2008 (epub ahead of print).
8. Hoffmann LA, Jarius S, Pellkofer HL, et al: Anti-Ma and anti-Ta associated paraneoplastic neurologic syndromes: Twenty-two newly diagnosed patients and review of previous cases. J Neurol Neurosurg Psychiatry 79:767-773, 2008.
9. Graus F, Dalmau J: Paraneoplastic neurologic syndromes: Diagnosis and treatment. Curr Opin Neurol 20:732-737, 2007.
10. VerscHu uren JJ, Perquin M, ten Velde G, et al: Anti-Hu antibody titre and brain metastases before and after treatment for small cell lung cancer. J Neurol Neurosurg Psychiatry 67:353-357, 1999.
11. Oh SJ, Dropcho EJ, Claussen GC: Anti-Hu -associated paraneoplastic sensory neuropathy responding to early aggressive immunotherapy: Report of two cases and review of literature. Muscle Nerve 20:1576-1582, 1997.
12. Bataller L, Dalmau J: Paraneoplastic disorders of the central nervous system: Update on diagnostic criteria and treatment. Semin Neurol 24:461-471, 2004.
13. Palao S, Corral I, Vera R, et al: Progressive dysautonomia as initial manifestation of anti-Hu antibody-related syndrome. Neurologia 22:899-902, 2007.
14. Wilhelm H: The pupil. Curr Opin Neurol 21:36-42, 2008.
15. Chan JW: Subacute complete ophthalmoplegia: An anti-Hu paraneoplastic manifestation of myxoid liposarcoma. Clin Experiment Ophthalmol 35:491-492, 2007.
16. Camdessanché JP, Antoine JC, Honnorat J, et al: Paraneoplastic peripheral neuropathy associated with anti-Hu antibodies. A clinical and electrophysiological study of 20 patients. Brain 125(pt 1):166-175, 2002.
17. Shams’ili S, de Beukelaar J, Gratama JW, et al: An uncontrolled trial of rituximab for antibody associated paraneoplastic neurologic syndromes. J Neurol 253:16-20, 2006.
18. Dalmau J, Rosenfeld M: Paraneoplastic syndromes of the CNS. Lancet Neurol 7:327â340, 2008.
19. Darnell R, Posner J: Paraneoplastic syndromes involving the nervous system. N Engl J Med 349:1543-1554, 2003.
20. Albert ML, Austin LM, Darnell RB: Detection and treatment of activated T cells in the cerebrospinal fluid of patients with paraneoplastic cerebellar degeneration. Ann Neurol 47:9â17, 2000.
Sarcoma Awareness Month 2023 with Brian Van Tine, MD, PhD
August 1st 2023Brian Van Tine, MD, PhD, speaks about several agents and combination regimens that are currently under investigation in the sarcoma space, and potential next steps in research including immunotherapies and vaccine-based treatments.