The Multidisciplinary Approach to Bone Metastases
With recent advances in the management of cancer, the clinicalcourse of patients with metastatic bone disease is more likely to beprolonged and accompanied by morbidity, including severe pain, hypercalcemia,pathologic fracture, and spinal cord and/or nerve root compression.The early identification of patients at higher risk for developingbone metastases enables practitioners to be proactive in their diagnosisand treatment. A multidisciplinary approach that integrates the diagnosisand treatment of the cancer, symptom management, and rehabilitationensures optimal care. Bisphosphonates can reduce the number ofskeletal-related complications, delay the onset of progressive disease inbone, and relieve metastatic bone pain caused by a variety of solidtumors with a resulting enhanced quality of life. The complexity of theclinical problem and the need to involve an array of health-careproviders present a logistical and clinical challenge. A strong argumentis made for a thematically integrated bone metastases program as partof the primary care of patients with cancer.
ABSTRACT: With recent advances in the management of cancer, the clinical course of patients with metastatic bone disease is more likely to be prolonged and accompanied by morbidity, including severe pain, hypercalcemia, pathologic fracture, and spinal cord and/or nerve root compression. The early identification of patients at higher risk for developing bone metastases enables practitioners to be proactive in their diagnosis and treatment. A multidisciplinary approach that integrates the diagnosis and treatment of the cancer, symptom management, and rehabilitation ensures optimal care. Bisphosphonates can reduce the number of skeletal-related complications, delay the onset of progressive disease in bone, and relieve metastatic bone pain caused by a variety of solid tumors with a resulting enhanced quality of life. The complexity of the clinical problem and the need to involve an array of health-care providers present a logistical and clinical challenge. A strong argument is made for a thematically integrated bone metastases program as part of the primary care of patients with cancer.
Bone metastases are most commonly associated with tumors of the breast, prostate, lung, and kidney, and with multiple myeloma. Bone metastases can also occur in association with other solid tumors. The spread of any cancer to bone can cause significant morbidity, including severe pain, hypercalcemia, pathologic fracture, and spinal cord and/or nerve root compression.[1] Randomized trials have determined that major skeletal events occur in patients with advanced breast cancer, on average, every 3 to 4 months, with 45% to 75% of patients developing pain and functional disability. Hypercalcemia occurs in 10% to 15% of patients, and fracture occurs in 10% to 20% of those with long bone metastases.[2,3]
Interdisciplinary assessments and interventions can result in improvement in quality of life and a decrease in the incidence of additional bone complications. However, the logistics and practicality of interdisciplinary assessments and interventions in this patient population are challenging. Physicians caring for patients with bone metastases should have ready access to all practitioners who can contribute to appropriate management. In addition to medical management, patients with bone metastases should be managed in the context of "whole/total" care, with the emphasis on psychosocial adaptation and quality of life.
FIGURE 1

Higher Risk for Bone Metastasis
Clinical pathways should be developed with early assessment and intervention for patients at higher risk for bone metastases (Figure 1), or with evident metastases, ensuring access, evaluation, and treatment by the full range of health-care providers. Such a team may include primary care physicians, medical/radiation/surgical oncology specialists, orthopedic surgeons, physiatrists, advanced practice nurses, social workers, and physical therapists.
That said, few health-care systems have formalized clinical pathways for the management of bone metastases. The object of this paper is to review the evidence for multidisciplinary care of patients with bone metastases.
Pathophysiology of Bone Metastases
Roodman reviewed the biology of the osteoclast and the pathophysiology of bone metastases and provided a foundation for clinical management.[ 4] The fundamental hypothesis of the development of bone metastases is that an interaction between tumor and bone cells leads to an increase in bone destruction and proliferation of tumor cells within the bony compartment. Local production of osteolytic factors by cancer cells in bone stimulates osteoclast-mediated bone resorption, which induces the produc tion of numerous growth factors and stimulates secretion of osteolytic cytokines, resulting in local foci of osteolysis.
The tumor and cancer cytokines have both a local and systemic impact. Locally, the tumor can stimulate osteoclasts in the microenvironment to produce interleukin (IL)-6, IL-1, tumor necrosis factor (TNF)-alpha, and macrophage inflammatory protein- 1-alpha. Systemically, the tumor can produce parathyroid hormonerelated protein, the mediator of the humoral hypercalcemia of malignancy. The combination of these effects can induce further stimulation of cancer cell growth, initiating a vicious cycle. Bone resorption may also play a role in formation of the osteoblastic lesions in patients with prostate cancer and occasionally in patients with other cancers.
Disease-Specific Issues
Breast Cancer
Bone metastases in women with breast cancer are a major clinical issue. Of the 200,000 women who are diagnosed with breast cancer annually in the United States, approximately 30% will develop bone metastases.[5] Body's review of bone metastasis statistics in women with breast cancer provides the rationale for early assessment and intervention.[2] The bones are the most common site of metastatic disease, both at initial presentation of metastases and as a site of first recurrence.[6] The common sites of bone metastases in decreasing order of probability are the thoracolumbar spine, pelvis, lower extremities, upper extremities, and skull.
Body and others estimate that among women with bone metastases as their first site of recurrence, approximately one-third can expect to develop major complications. The probability of bone complications is greatest in patients with bone-only disease compared to patients with extraosseous first recurrences, 81% vs 21%. The incidence of fractures is more common in women with breast cancer than in men with prostate cancer, because fractures are more common in lytic than in blastic bone metastases.[7]
A rationale for proactive management in women with breast cancer and bone-dominant metastases is provided by the observation that these women have a better prognosis than those without bone metastases, can expect a major skeletal event on average every 3 to 4 months, and usually live beyond 2 years. Indeed, approximately 10% live 5 to 10 years from the diagnosis of bone metastases. In other words, women with initial presentations involving bone metastases as opposed to other sites show increased survival times, with a median survival of 48 months compared to 17 months. Women who have bone-only disease are more likely to be older, to have axillary node involvement, and to have lobular carcinoma.[6]
The International Breast Cancer Study Group (IBCSG) has formulated risk assessment guidelines for breast cancer patients. Their study evaluated patterns of recurrence among 6,792 patients included in IBCSG trials of adjuvant treatment and found that the highest cumulative incidence of bone metastases occurred among patients presenting with four or more positive axillary nodes at the time of diagnosis (15% at 2 years and 41% at 10 years) and among those who had a locoregional recurrence or a recurrence in soft tissue as their first event, without other evident metastases (22% at 2 years from first recurrence and 37% at 10 years).[8] The authors proposed that this higher-risk subset of patients could benefit most from early assessments and interventions for bone metastases.
Prostate Cancer
Bone metastases from prostate cancer differ significantly from those of other primary cancer sites, in light of the usual occurrence of both osteoblastic and osteolytic lesions. Predictors of skeletal morbidity are generally thought to be the extent of bone involvement, the severity of pain, the patient's overall performance status, the serum alkaline phosphatase level, the urinary deoxypyridinoline level (which maintained its significance in a multivariate analysis), and androgen deprivation.[9]
Dawson[10] and others have provided statistics demonstrating the profound impact of bone metastases on men with prostate cancer. For example, 80% of men who die of prostate cancer have bone metastases at autopsy, and bone pain is a clinical problem in 88% of such patients. In a prospective study of 112 men with hormone-refractory prostate cancer and bone metastases, 30% had documented skeletal complications at death or last follow-up (at an annual incidence of 12%). In 18%, the complication involved vertebral collapse or deformity, 9% had pathologic fractures, and 6% had spinal cord compression. The median time to initial skeletal complication was 9.5 months.[11]
With the availability of prospective clinical trials in men with bone metastases from prostate cancer, we now have data to predict skeletally related events. In a 15-month prospective study period of observation alone in prostate cancer patients with bone metastases, 44% had at least one skeletal event, 22% had a fracture, and the time to first occurrence of any skeletal event was 321 days. These statistics put into perspective the importance of reducing skeletally related events and morbidity in this high-risk population.[12]
Myeloma
Multiple myeloma, which is newly diagnosed in approximately 14,000 people per year in the United States, is another cancer in which skeletal complications are clinically important. The mechanisms of bone destruction are related to cytokines produced by the myeloma cell and normal bone marrow stromal cells. The important bone resorbing factors are thought to be IL-1, IL-6, TNF, and the receptor for activation of nuclear factor kappa- B ligand.[13-15] The increased osteoclastic activity in the bone marrow causes loss of bone structure and pathologic fractures, hypercalcemia, and pain. The radiographic appearance is almost always purely lytic with little or no osteoblastic component and is more likely to fracture, resulting in significant morbidity. These fractures are most troublesome when associated with collapse in the vertebral spine.
Other Tumor Types
Bone-related complications occur in other solid tumors as well. Approximately 30% to 60% of patients with advanced lung cancer develop bone metastases.[16] Among patients with invasive bladder cancer, 22% develop bone metastases,[17] and of patients with locally advanced or metastatic renal cancer, 35% have bone metastases at their initial diagnosis.[ 18] Aggressive solid tumors are often refractory to current therapies, and treatment of the primary cancer rarely achieves responses in bone. Furthermore, bisphosphonates have not been extensively studied in these patient populations.
Bone Metastasis Markers
Markers of bone metastases could potentially be used to establish the diagnosis and/or to predict which patients are at higher risk. In general, the ability to associate specific biomarkers with the presence of or increased likelihood of developing bone metastases has value. These bone biomarkers could either be elevated in patients with bone metastases or related to tumor-specific markers. Bone markers would be of value for early detection and follow-up to assess the clinical course of metastatic bone disease. These markers could also provide targets for novel therapeutic approaches that interfere with growth and enhance apoptosis in bone stromal compartments.[19]
Immunohistochemical methods may offer useful predictors of patients at higher risk for bone relapse. Although not validated in large numbers of patients, elevated serum levels of bone sialoprotein and parathyroid hormone- related protein appear to correlate with an increased incidence of bone metastases in breast cancer patients. More recent studies have supported this hypothesis by demonstrating that serum bone sialoprotein level is the most important independent prognostic marker for subsequent development of bone metastasis in patients with breast cancer.[20]
Other studies have shown that transforming growth factor (TGF)- beta-1 levels are increased in prostate cancer patients with metastases to regional lymph nodes and bone.[21] In men without clinical or pathologic evidence of metastases, an elevated preoperative plasma TGF-beta 1 level is an independent predictor of progression and associated with occult metastatic disease. Elevated preoperative levels of IL-6 and soluble IL-6 receptor may also be associated with bone relapse in men with prostate cancer.[22]
Fewer studies exploring markers of bone metastases in primary lung cancers have been published. Izumi et al demonstrated that urinary pyridinoline cross-linked N-telopeptides of type I collagen may be the most useful biomarker in the assessment of bone metastases in patients with lung carcinoma.[23]
Diagnosis
The frequency with which metastases are observed varies with the type of primary tumor, the associated risk factors, and the modality used for detection (Figure 1). The primary methodologies used clinically are regular clinical screening and assessment of symptoms that could be attributable to bone metastases, especially pain, plain film radiography, bone scintigraphy, nuclear imaging, and magnetic resonance imaging (MRI). The use of positron-emission tomography (PET) to identify metabolically active areas of tumor growth is also being explored.[24]
Plain Film Radiographs
Plain film radiographs provide a fast, inexpensive, and readily available technique for evaluating bone metastases and are often the first test ordered in the evaluation of bone pain. Although not the most sensitive test, plain films offer the best integration of overall bone structure and alignment and correlate best with clinical features.[25] It is important that the entire bone be imaged, so that all lesions can be addressed and stabilized during the same operative procedure. In addition, sequential radiographs of involved areas are key for monitoring response to treatment, local recurrence, and disease progression.
Computed Tomography
Computed tomography (CT) images are more sensitive than plain film radiographs, more specific than bone scans, and can image the extent of involvement and anatomic relationship to normal structures. They can also be used to predict fracture through metastatic bone tumors. Cordio et al prospectively studied breast cancer patients with spinal metastases and showed that CT-based structural analysis was as sensitive and more specific than radiographic criteria (59% vs 24% accurate) in predicting fracture.[26]
Bone Scintigraphy
Bone scintigraphy provides an efficient means of measuring the metabolic activity of the entire skeleton. Whereas 30% to 50% of bone mineral must be lost for a lesion to appear on plain radiography, technetium diphosphate bone scans demonstrate bone involvement much earlier. Bone scans are especially useful in identifying sites of both symptomatic and asymptomatic lesions and in establishing potential sources of referred pain.
Magnetic Resonance Imaging
MRI provides helpful three-dimensional (3D) anatomic information and is excellent in defining soft tissues and delineating soft-tissue involvement by tumor. Altehoefer et al retrospectively compared MRI of the axial skeleton with whole-body bone scintigraphy in 81 patients with histologically proven breast cancer.[27] MRI detected bone metastases in 54 (67%) of 81 patients, proving to be the better modality for the detection of metastases, determination of the extent of axial skeletal metastatic disease, and assessment of therapeutic implications. In retrospect, the bone scan was falsely negative in 7 (13%) of 54 patients with spinal metastases and underestimated the extent of disease in 26 (49%) of 53 patients.
On a patient-by-patient comparison of the presence or absence of bone metastases, the comparative sensitivities and specificities of the imaging techniques were 98% and 100% for MRI and 87% and 100% for bone scintigraphy, respectively.[27] The authors concluded that the higher sensitivity of MRI in detecting spinal lesions, even in regions that were negative on bone scintigraphy, make it especially suitable as a screening method for bone lesions. They recommend, however, that bone scintigraphy be performed in addition in patients with a positive MRI, to screen remote skeletal regions. Detection is thus maximally effective when MRI is correlated with additional imaging studies.
Spinal Cord Compression
Spinal cord compression presents a diagnostic challenge. It can be a devastating complication of malignancy with irreversible loss of neurologic function and profound effects on quality of life. A retrospective analysis of the features of 123 episodes of suspected spinal cord compression among 93 breast cancer patients by CT scan of the spine identified four independent predictors of thecal sac compression. These factors include known bone metastases for 2 or more years, metastatic disease at initial diagnosis, objective weakness, and vertebral compression fracture on spine radiograph.[28]
In order to assess risk adequately in this population, the evaluation of patients with suspected spinal cord compression should include both clinical information about the disease course as well as neurologic examination and imaging studies. Presumably, these observations in women with breast cancer can be generalized to other clinical diagnoses involving spinal metastases. Patients with progressive symptoms of spinal cord compression should be empirically started on steroids before undergoing MRI to establish a diagnosis.
Treatment
Surgery
FIGURE 2

Bone Metastasis Program
• Clinical Pathways and Medical Decision-Making-Among patients with bone metastases or considered to be at risk, bone lesions should be monitored continuously with periodic bone imaging to prevent progression to pathologic fracture, and when clinically indicated, should be treated prophylactically with surgery, radiotherapy, chemotherapy, hormonal manipulation, bisphosphonates, and/or receive supportive services (Figure 2).
A practical scoring system that combines four roentgenographic and clinical risk factors into a single score may be of value in the selection of patients for prophylactic fixation.[29] Although controversial, this score delineates the following radiologic features as predictors of imminent fracture: pain, anatomic site of the lesion, its radiologic characteristics, and its size. As the mean score described in the study rises above 7, the percentage risk of fracture increases accordingly.
In developing a care plan, the merits of prophylactic surgery should be considered for the patient with bone lesions. Aggressive local therapy is necessary to alleviate pain and restore skeletal stability. Proactive orthopedic management enables a simpler and safer operation. With early diagnosis, timely intervention is essential to prevent pathologic fractures in patients with a malignancy. Lesions that will predictably fracture, involve joints, or cause catastrophic consequences if fracture occurs should be strongly considered for prophylactic surgical stabilization. In addition, rapid rehabilitation is important because bone tissue in these lesions undergoes significant structural changes.[30]
Colyer makes the point that neoplasm control should not override concern for function, especially since objective cure of the neoplasm is so rarely achieved in patients with metastatic bone disease. Even if the metastasis is removed, a bone that has lost its structural integrity (even if not grossly fractured) will not support weight-bearing for months.[31]
The clinical decision to perform a surgical intervention must be made in the context of the patient's overall situation. The major consideration in this situation is the patient's functional status and what can be done to preserve it in the face of bone metastases. On the other hand, a surgical intervention that would require months to restore function must be put in the context of a patient's anticipated survival.
• Surgical Interventions-Surgical treatment of bone metastases is generally palliative. All procedures must guarantee stability, early mobilization, and brief hospitalization, in light of what is usually a shortened life expectancy.[ 32] Surgery is indicated in patients with pathologic fractures of the long bones and those involving the hip joints, in patients with spinal lesions, and in patients with compression of peripheral nerves. In advanced cancer patients in poor overall condition, intramedullary nailing without resection of metastasis is palliative,[ 33] providing pain relief and partial restoration of function in the involved area.
Healy and Brown reported that of 55 patients who underwent reconstruction of the acetabulum for metastatic disease, only 9% incurred a late fixation failure.[34] Of the 41 patients evaluable at 3 months, 83% continued to experience significant pain relief and 50% of nonambulatory patients regained the ability to walk as a result of the procedure. Another strategy for management is a more extensive local excision of tumor tissue and filling of the defect with methylmethacrylate, augmented by internal fixation, which can provide pain relief and an improved quality of life.[35]
Methylmethacrylate enhances the stability of pathologic fractures and furthers the goals of treatment by improving the results of fracture management in severely compromised patients.[36] Various studies have supported the use of this substance in procedures that aim to restore function to affected extremities and relieve pain.[37]
Radiation Therapy
Good clinical practice requires that all patients with symptomatic bone metastases and lesions in long bones be evaluated for radiation therapy prior to surgical intervention. In treating pain and its underlying cause, symptom- appropriate medical analgesia and localized external-beam radiation therapy are the complementary cornerstones in the management of patients with symptomatic osseous metastases. More favorable lesions in long bones may be effectively irradiated without risk of fracture, whereas more unfavorable lesions may require prophylactic internal fixation prior to irradiation. The therapeutic intent is to relieve pain, and if a patient has undergone prophylactic fixation or surgical stabilization of an existing fracture, radiation therapy significantly reduces the risk of further tumor growth and bone destruction.
For most patients, external-beam radiotherapy provides excellent palliation for localized metastatic bone pain. Radiotherapy may also be indicated for patients at risk of pathologic fracture and neurologic complications arising from spinal cord compression, nerve root pain, or cranial nerve involvement. Studies have shown that single-fraction regimens (mostly 8 Gy), which can be more convenient for patients and providers, are at least as effective as various fractionated regimens.[38] A meta-analysis of eight completed randomized trials of single-fraction radiotherapy (median: 8 Gy) vs multifraction radiotherapy (median: 20 Gy in five fractions) showed no significant difference in complete overall pain response between the two regimens.[39]
Radiopharmaceuticals are also available for the palliation of metastatic bone pain. Strontium-89 (Metastron) has been shown to be as effective as wide-field radiotherapy in patients with prostate cancer.[40] Studies have also demonstrated that samarium-153 (Quadramet) has a significant effect on bone pain, but boneseeking radiopharmaceuticals have a dose-limiting toxicity that results in thrombocytopenia. Further studies are indicated to compare radioisotope treatment with high-dose bisphosphonates and to determine whether the two therapies are complementary.
Bisphosphonates
• Preclinical Studies-Bisphosphonates, a class of synthetic compounds, have a strong affinity for the hydroxyapatite crystal of bone, inhibiting bone resorption and, therefore, providing an effective treatment option for hypercalcemia of malignancy. Bisphosphonates have also been shown to decrease bone complications of cancer by reducing the number of skeletal complications in multiple myeloma and breast cancer; by delaying the onset of progressive bone disease following palliative chemotherapy for breast cancer, prostate cancer, and myeloma; and by relieving metastatic bone pain caused by a variety of solid tumors.[41]
Bisphosphonates contain a P-C-P bond that promotes binding to mineralized hydroxyapatite crystal bone matrix and fosters the inhibitory effect on bone resorption. The remainder of the bisphosphonate molecule varies according to structural differences in each drug's specific side chain, which directly determines its exact mechanism of action, relative potency, and side effects.
First-, second-, and third-generation bisphosphonates such as clodronate, pamidronate (Aredia), and zoledronate (Zabel, Zometa), respectively, have differing potencies and effects. All bisphosphonates are alike, however, in that they localize preferentially to sites of active bone remodeling. Compared to pamidronate, zoledronate is a more potent inhibitor of osteoclast-mediated bone resorption, because of the heterocyclic twonitrogen- containing side chain.[42]
Preclinical research has also recognized that bisphosphonates inhibit the formation of osteoclasts, interfere with signaling between osteoclasts and osteoblasts, and induce apoptosis in osteoclasts. The impact of bisphosphonates on decreasing bone resorption is evident by a reduction in bone resorption markers. The cellular and molecular mechanisms of action are influenced by the nitrogen moiety of the bisphosphonate. Clodronate does not contain a nitrogen moiety and can be metabolized to an ATP analog that is toxic for macrophages and osteoclasts. Pamidronate and zoledronate do contain a nitrogen moiety, and thus interfere with the mevalonate pathway that is crucial for the maintenance of cell membrane integrity.
Preclinical studies of zoledronate have demonstrated possible direct anticancer activity. Recent cell culture data indicate that nitrogen-containing bisphosphonates, including pamidronate and zoledronate, exert antitumor properties and interact synergistically with other antineoplastic agents.[43] Further investigation must determine whether this effect also plays a role in vivo.
A murine model was created to assess the impact of bisphosphonates on bone pain. In this animal model, investigators studied spontaneous and elicited behaviors, as well as neurochemical analysis and immunohistochemical detection of hyperalgesic peptides and neurochemical markers. Clohisy found that the pain created by bone cancers was biochemically distinct from inflammatory and neuropathic pain states.[44] This supports the hypothesis that bisphosphonates relieve pain through a unique mechanism of action.
In a rat model of metastatic cancer pain, zoledronate was shown to be unique in its pronounced antinociceptive effects.[45] This study demonstrated that zoledronate reverses hyperalgesia, whereas pamidronate and clodronate do not. Indeed, zoledronate may have analgesic effects that could be used in a broader range of pain indications.
In another preclinical study, Padalecki et al investigated in vivo evidence that androgen-deprivation therapy triggers bone loss and may increase prostate metastases to the skeleton.[46] Using PC-3 inoculated mice, they found that treatment with zoledronate prevented bone loss due to androgen deprivation and reduced prostate cancer metastases to the skeleton. Further research is needed to determine whether hypogonadal men with advanced prostate cancer would benefit from adjuvant use of bisphosphonates.
• Pharmacology-The pharmacokinetics of bisphosphonates differ by route of administration. Oral bisphosphonates have low and variable absorption rates, require frequent dosing, and are associated with adverse gastrointestinal effects. By contrast, intravenous bisphosphonates have characteristic biphasic pharmacokinetics. The initial elimination occurs by rapid renal clearance in the first 24 hours, accounting for approximately one-third to two-thirds of the administered dose. The terminal elimination phase is prolonged because bisphosphonates bind to bone, thus supporting the rationale for monthly administration. Urinary elimination continues for periods of months, indicating long-term retention in bones. The half-life of these agents is greater than 6 months. Of note, bisphosphonates are not significantly bound to plasma and are excreted unaltered in the urine.[47]
Chen et al described the pharmacokinetics and dynamics of zoledronate in patients with bone metastases.[48] As with the other in- travenous bisphosphonates, 40% of a zoledronate dose is excreted in the urine in the first 24 hours after administration, with persistent low-level urinary excretion continuing for extended periods of time consistent with the prolonged half--ife. The data suggest that even after multiple administrations, uptake in bone is not saturable and retention in bone is greatest in the area of bone resorption.
TABLE 1
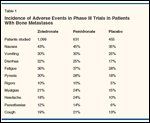
Incidence of Adverse Events in Phase III Trials in Patients With Bone Metastases
• Toxicology-The toxicity of the bisphosphonates in cancer patients have been best assessed in phase III randomized studies comparing the bisphosphonates to placebo and directly comparing two bisphosphonates, pamidronate and zoledronate. The most common toxicities of these agents are the acute-phase symptoms associated with intravenous bisphosphonates- ie, fatigue, anemia, myalgia, weakness, and pyrexia. These toxicities were reported more frequently by patients treated with zoledronate than by those receiving placebo (Table 1).
The incidence of renal toxicity from the bisphosphonates varies with the rate, dose, and volume of administration. The 8-mg dose of zoledronate is more toxic than the 4-mg dose, and 5-minute infusions are more toxic than 15-minute infusions. A partial explanation, based on in vitro data, is that insoluble bisphosphonate precipitates accumulate with higher concentrations. The incidence of renal toxicity associated with bisphosphonate use also varies depending on the patient population. The best estimates of renal toxicity can be made by comparing bisphosphonates with each other and with placebo.
For example, in the prospective comparison of zoledronate vs placebo in men with bone metastases from prostate cancer, the incidence of significant renal impairment was 15% for the zoledronate group compared to 13% for the placebo group.[12] No apparent difference in incidence or in the estimates of time to first renal dysfunction occurred between groups. In another study comparing pamidronate to zoledronate in patients with bone metastases from breast cancer or multiple myeloma, the incidence of grade 3/4 serum creatinine elevation was approximately 1%.[49]
• Efficacy-The bisphosphonates have potential therapeutic benefit in a variety of clinical scenarios. Compared to placebo in patients with known bone metastases, the bisphosphonates have reduced the number of skeletally related events, with corroboration by secondary end points. In patients without known bone metastases but at high risk for such disease, these agents have increased the time to their development. In patients with osteoporosis-for example, as a consequence of androgen ablation- bisphosphonates can prevent bone loss.
The evidence demonstrating the efficacy of the bisphosphonates in the management of bone metastases is based on prospective, often randomized clinical trials with clearly defined end points. The most commonly used primary study end point is a skeletal-related event (SRE), which is usually defined as (1) a pathologic fracture, (2) the need to irradiate bone because of progressive symptoms, (3) surgical intervention for bone metastases, (4) spinal cord compression, and in most studies, (5) the develop- ment of hypercalcemia. In addition, a change in antineoplastic therapy to treat progressive bone pain could be considered an SRE.
Time to first SRE is an important clinical end point. Another timerelated end point is the metastasesfree interval, which can be expressed as a site-specific parameter (eg, bone metastases-free interval or nonbone metastases-free interval). The skeletal mortality rate is the ratio of the number of SREs divided by the observation time. Both the total number of events and the time to each event are clinically relevant end points.
The Andersen-Gill multiple events analysis method can be used to account for multiple SREs over time.[50] This analysis includes the proportion of patients who experienced a skeletal event and the time to the first such event. Other end points used in prospective clinical trials include change in bone density, pain score, qualityof- life measures,performance status, Functional Assessment of Cancer Therapy (FACT) scores, and serum markers of bone biochemistry.
Based on these end points, the second- generation bisphosphonate pamidronate became a standard of care for treating complications of bone lesions. Coleman demonstrated that the use of pamidronate in patients with pretreated progressive bone metastases (52 with breast carcinoma, 17 with prostate carcinoma, and 17 others), without any other systemic anticancer treatment, reduced a symptom score measuring pain (World Health Organization [WHO] performance status) and analgesic consumption and/or improved quality of life compared with placebo.[1] Symptomatic response also correlated with a minor decrease in tumor marker levels, suggesting a possible effect of bisphosphonates on tumor activity.
Disease-Specific Indications for Bisphosphonate Therapy
• Breast Cancer-Pamidronate has proven useful for the treatment of bone pain in patients with breast cancer and known bone metastases. One placebo- controlled, double-blind randomized trial demonstrated that pain relief occurred in 48% of patients who received pamidronate.[41] However, patients with high rates of bone resorption, correlating with elevated levels of bone-specific markers derived from the breakdown of type I collagen, did not respond to pamidronate. Intermediate markers would be useful in selecting patients likely to respond to long-term bisphosphonate treatment.
In a randomized placebo-controlled trial in patients with advanced breast cancer and lytic bone lesions, Theriault et al found that 90 mg of pamidronate used together with systemic hormonal and radiation therapy resulted in a significant decrease in the frequency of skeletal morbidity.[51] The study also demonstrated that pamidronate, given as a 2-hour infusion every 4 weeks, induced a sustained decrease in biochemical markers of bone resorption and formation. Overall survival did not differ between study groups. Pamidronate improved quality of life in patients with bone lesions.
The 2000 American Society of Clinical Oncology (ASCO) guidelines on the role of pamidronate in breast cancer recommend its use as an adjunct to systemic chemotherapy and/ or hormonal therapy in women with bone pain due to osteolytic bone metastases.[ 52] Given the conflicting published results, the panel advised that current standards of care for cancer pain from bone metastases- primarily analgesics and local radiotherapy- not be displaced by bisphosphonates. The use of bisphosphonates in patients with no evidence of bone metastases was not recommended; these agents decrease the rate of skeletal morbidity but do not completely eliminate bone complications. The ASCO guidelines are being updated.
Rosen et al conducted a doubleblind, randomized phase III international study in 1,116 patients with bone metastases from breast cancer (n = 766) or multiple myeloma (n = 350) that was designed and powered to demonstrate the similar efficacydronate.[53] Prior to randomization, patients were stratified into three groups: (1) breast cancer patients receiving hormonal therapy; (2) breast cancer patients receiving chemotherapy; and (3) myeloma patients.
The 9-month analysis showed that a 15-minute infusion (4 mg) of zoledronate was as effective as a 2-hour infusion of pamidronate (90 mg), with patients experiencing an increase in bone density, decrease in bone resorption and bone resorption markers, and fewer bone fractures. Adverse events were similar for both pamidronate and zoledronate. The shorter infusion time resulted in greater convenience for patients and an improvement in compliance.
The final analysis of the entire study population performed at 24 months continued to show the noninferiority of zoledronate. However, in the multiple- events analysis, zoledronate decreased the risk of developing an SRE by 16% (hazard ratio = 0.841; 95% confidence interval [CI] = 0.719- 0.983; P = .030). In a retrospective subset analysis of patients in the breast cancer-hormonal stratum, zoledronate significantly extended the time to first SRE to a median of 415 days, compared to 370 days for pamidronate (P = .047). In a multiple-events analysis, zoledronate reduced the risk of developing an SRE by 20% (hazard ratio = .80; P = .025) compared to pamidronate. This difference was not apparent in the breast cancer-chemotherapy stratum.[53,54]
• Myeloma-The phase III study described above included 350 patients with Durie-Salmon stage III multiple myeloma and at least one osteolytic bone lesion; 183 were randomized to zoledronate and 167, to pamidronate.[ 53] The primary end point data are included in the breast cancer analysis above. In a retrospective subset analysis of results in patients with myeloma, the median time to first SRE was 380 days in the 4-mg zoledronate group and 286 days in the 90-mg pamidronate group (P = .538). In the multiple-event analysis, the hazard ratio for the risk of developing an SRE did not reach statistical significance (P = .593).[53]
• Prostate Cancer-Two multicenter, double-blind, randomized placebo-controlled trials investigated pamidronate in 378 men with bone metastases from prostate cancer. Pamidronate was ineffective in reducing the number of SREs or other clinical end points.[55]
Smith et al established the efficacy of pamidronate in preventing bone loss in the hip and lumbar spine in men undergoing treatment for prostate cancer with a gonadotropin-releasing hormone agonist.[56] By preventing a decrease in bone mineral density-an important determinant of the risk of fracture typically seen in patients receiving this therapy-pamidronate is now indicated for the prevention of pathologic fracture in prostate cancer patients. Pamidronate is an alternative to testosterone-replacement therapy for the prevention of hypogonadal bone loss in men with contraindications to testosterone therapy, but the optimal dose and schedule in these men is still being determined.
In a double-blind, placebo-controlled, phase III trial, Saad et al demonstrated that zoledronate at 4 mg every 3 weeks for 15 months reduced the incidence of SREs in hormonerefractory prostate cancer patients with bone metastases.[12] Entrance criteria included bone metastases, a rising prostate-specific antigen level, demonstrated disease progression despite hormonal therapy, a baseline serum testosterone within the castrate range, appropriate antineoplastic therapy, and an Eastern Cooperative Oncology Group performance status less than 3. A total of 643 men were randomized with the initial intent of including an 8-mg dose; 221 patients received the 8-mg dose, but this group was dropped from the analysis because of drugrelated deterioration in renal function, leaving 214 patients in the treated group and 208 patients in the placebo group.
Among patients who received a placebo, 44% developed SREs compared to 33% who had received zoledronate at 4 mg (difference = -11.0%, 95% CI = -20.3% to -1.8%; P = .021). With additional follow-up, corroborating data have become evident (personal communication, F. Saad, 2002). Zoledronate significantly reduced the number of skeletal complications a patient experiences in a year from 1.47 to 0.77 events (P = .005) and delayed the median time to first SRE from 321 to 488 days (P = .009). In a multiple- events analysis, treatment decreased the risk of developing a skeletal complication by 36%, with a hazard ratio at 24 months of 0.64 (95% CI = 0.485-0.845; P = .002).
Supporting these therapeutic benefits of zoledronate was the statistically significant decrease in levels of urinary markers of bone resorption in patients who received zoledronate at either dose (P = .001). In addition, pain and analgesic scores increased to a greater extent among patients who received placebo than among those who received zoledronate, but there were no differences in disease progression, performance status, or quality- of-life scores between groups.
The adjuvant role of zoledronate is currently being explored in advanced prostate cancer. Although bone lesions in prostate cancer are typically osteoblastic, biochemical and histologic studies have shown that osteoblastic bone formation is preceded by osteoclast activation. Because the primary cellular target of bisphosphonates is the osteoclast, these drugs appear to be indicated for the treatment of prostate cancer.
Two prospective, randomized, double- blind, placebo-controlled, multicenter phase III trials are ongoing. The first is a primary prevention study exploring the effects of zoledronate on bone metastases-free survival in 500 men with prostate cancer at high risk of developing bone metastases but with no radiologically detectable metastatic disease. Men were randomized to receive standard antitumor adjuvant therapy and zoledronate or placebo. The second study is an openlabel, randomized, multicenter study examining the effects of zoledronate on bone mineral density in 200 men with recurrence of prostate cancer.
• Other Solid Tumors-The efficacy of zoledronate on SREs in other solid tumors was evaluated in a randomized, double-blind, placebo-controlled, international, multicenter study that enrolled 773 patients. The trial compared zoledronate at 4 mg (n = 257) and 8 mg (n = 266) via 5-minute infusion every 3 weeks to placebo (n = 250). After enrollment was complete, the study was amended based on interim renal toxicity analysis to increase the infusion time to 15 minutes and the infusate volume to 100 mL, and reduce the 8-mg dose of zoledronate to 4 mg. The latter group was excluded from the efficacy analysis. In the remaining group, 49% had non-small-cell lung cancer, 10% had renal cell carcinoma, and 8% had small-cell lung cancer, 23% with known and 7% with unknown primary solid tumors.[57]
At the 9-month first planned analysis, 38% of zoledronate patients vs 47% of placebo patients experienced an SRE (P = .039). Zoledronate delayed the time to first SRE by 67 days (P = .023). At the 21-month second planned analysis, zoledronate significantly reduced the percentage of patients who experienced an SRE (39% vs 48% for placebo; P = .039) and the number of skeletal complications in a year from 2.7 to 1.7 (P = .12), and significantly delayed the onset of skeletal complications from a median time to first SRE of 155 days to 236 days (P = .009). In a multiple-events analysis, zoledronate reduced the risk of developing an SRE by 31% compared with placebo (hazard ratio = .693; 95% CI = 0.542-0.886; P = .003).
Chemotherapy and Hormone Therapy
In patients with bone metastases, the goals of chemotherapy and hormonal therapy are pain control, disease stabilization, and a reduction in the risk of skeletal morbidity. Systemic therapy for cancer is evidencebased and disease- and clinical circumstance-specific. Several sets of guidelines have been published for disease-specific treatments.
There is no evidence to suggest that bone metastases are more or less responsive to chemotherapy or hormonal therapy than other metastatic sites. In planning chemotherapy or hormonal therapy, the assumption is that the most effective systemic treatment for metastatic disease would also be the indicated treatment for patients with bone metastases. The manage ment of systemic therapy should be integrated with the multidisciplinary approach to bone metastases, with the goal of reducing skeletal-related morbidity.
Pain Management
Pain is the most frequent symptom of bone metastases, developing slowly and becoming progressively more severe. The management of cancer pain is well established in internationally accepted guidelines for repetitive assessment and treatment of reversible causes of cancer pain, with concurrent use of analgesics. Palliation of pain can result in a significant return of quality of life. Analgesic therapy is indicated with the combination of an acetaminophen-based analgesic or nonsteroidal anti-inflammatory drug and/or opioids used in accordance with the WHO Ladder Approach for Relief of Cancer Pain.[58] These guidelines stratify pain into levels of intensity and suggest adjusting the strength and potency of prescribed analgesics accordingly.
• Adjuvant Agents-The guidelines also suggest adding an adjuvant medication to these narcotic and nonnarcotic agents when appropriate. Adjuvant medications are defined as those whose initial use was not for pain, but rather for the treatment of other conditions. These medications, which include steroids, bisphosphonates, antidepressants, anticonvulsants, antihistamines, and sedatives, are often useful in treating opioidrefractory pain in combination with opioids.
For bone pain specifically, the most commonly used adjuvant analgesics are bisphosphonates, corticosteroids, calcitonin, and radiopharmaceuticals. Corticosteroids can be used throughout the course of cytotoxic chemotherapy and radiation therapy to treat the inflammatory component of the pain. Nonsteroidal anti-inflammatory agents (NSAIDs) and cyclooxygenase- 2 (COX-2) inhibitors may be used as adjuvants after platelet count and function have recovered following chemotherapy and radiation therapy. Zoledronate has been used successfully to treat patients with bone pain, but further research is needed to determine its exact analgesic properties in patients with metastatic disease to the skeleton.
Patient/Family Education and Psychosocial Support
In the multidisciplinary approach to the treatment of bone metastases, an integral part of the care team's role is the education of patients and their families. By offering diagnosis-and treatment-specific information to patients who have misconceptions and may be hesitant to ask for such information, education aims to reduce the patient's sense of helplessness and inadequacy due to lack of knowledge. Coping-skills training, emotional support, and targeted counseling have also been shown to ease the disruption and distress that accompanies cancer diagnosis.
Patients with bone metastases can benefit from education about fracture prevention, pain management, and maintenance of daily activities. First, patients should learn about the drugs available to minimize bone loss. For example, the incidence of fracture can be reduced by the use of bisphosphonates as well as nonpharmaceutical measures, such as maintaining body weight, increasing non-weight-bearing exercise, minimizing caffeine and alcohol intake, and stopping smoking. Educating patients about the risks of falls and developing individualized programs to increase physical stability are also critical.
Perhaps most importantly, patients should be aware that pain is a part of metastatic disease and that it can be controlled. Myths about cancer pain and treatment are widespread and often lead to undertreatment. For example, many patients prefer to avoid strong opioids like morphine due to the fear of addiction. Also, some patients express a desire to reserve the use of opioids in case pain worsens over time. These myths can best be dispelled through comprehensive patient and family education.
When educating patients and families about bone metastases, it is key to remember that skeletal metastases have an impact on the ability to main- tain both physical and psychosocial functions. Nursing models such as the Roy Adaptation Model identify three spheres that are commonly impaired in patients with bone metastases. They are primary (self), secondary (family and occupation), and tertiary (community) roles.[59] Patient education and active interventions such as relaxation therapy, guided imagery, music, meditation, and therapeutic touch have been shown to promote adaptation. Assessment, patient education, and symptom management can assist in the physical and psychosocial adaptation of patients with bone metastases.
Rehabilitation
From a rehabilitative standpoint, patient adaptation to the changes that accompany bone metastases, like those related to daily performance, loss of function, and modification of lifestyle, is of special interest. The goals of care are heterogeneous, with patient preferences strongly influenced by age, disease status, and expectations for recovery. In addition, problems such as nutrition, psychosocial concerns, and treatment of pain need to be integrated into the rehabilitation program.
Physiatrists, occupational therapists, physical therapists, recreation therapists, nutritionists, and psychologists may all be part of the rehabilitation team. Physiatrists assess functional ability, relative strength and stamina, and the biomechanics of the skeleton, and typically coordinate rehabilitation services and prepare a plan for treatment and follow-up. Occupational therapists determine which supportive services are available to a person and identify interventions to improve quality of life. Physical therapists provide treatment of human motion and frequently help to relieve painful skeletal symptoms via nonpharmacologic modalities.[60] Recreation therapists help patients increase activity levels and use social supports.
Psychologists provide emotional support and guidance, and nutritionists focus on the cancer-associated weight changes and recommend dietary adjustments. They also evaluate the appropriateness of appetite-stimulating drugs, such as cannabinoids or progestational agents, but consideration must be given to the impact of hormonal agents on bone density.[61] Enteral feeding may also contribute to complete rehabilitation after cancer therapy.
When prescribing exercise in this population, treatment goals should be individualized to what patients can do safely, while also promoting independence at minimal risk. Early mobilization is an important goal. Exercise that promotes fitness with a minimal impact on bone, such as aquatics, is suggested. Other recommended options include isometric rather than resistive strengthening and activities that minimize single-limb weight bearing for the lower extremities. Education to maximize safety in performing such exercise is also critical.
REFERENCE GUIDE
Therapeutic Agents
Mentioned in This Article
Clodronate
Morphine
Pamidronate (Aredia)
Samarium-153 (Quadramet)
Strontium-89 (Metastron)
Zoledronate (Zabel, Zometa)
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
The person with cancer confronts a range of psychosocial distresses, including loss of self-esteem, anxiety, and fear. Each of these responses needs to be addressed and managed individually, with the support of the rehabilitative team. Emotional support, comfort, and education, provided by the oncology and rehabilitation teams, are key factors in promoting and preserving quality of life. By addressing both the physiologic and psychosocial needs of the patient, the rehabilitation team can promote a return to function and improved quality of life in patients with bone metastases.
Conclusions
The management of bone metastases has improved with advances in assessment, detection, cancer treatment, and the use of bisphosphonates. Even with these developments, patients suffer from skeletal complica- tions. The interdisciplinary team involved in the care of the patient with bone metastases ideally should work collaboratively, using state-of-the-art assessments and interventions to minimize morbidity, maintain quality of life, and maximize patient convenience. Improved clinical outcomes in all of these areas will emerge as research identifies optimal treatment models for the care of these patients.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1.
Coleman RE: Skeletal complications ofmalignancy. Cancer 80(8 suppl):1588-1594,1997.
2.
Body JJ: Bisphosphonates in the treatmentof metastatic breast cancer. J MammaryGland Biol Neoplasia 6:477-485, 2001.
3.
Hortobagyi GN, Theriault RL, Porter L,et al: Efficacy of pamidronate in reducing skeletalcomplications in patients with breast cancerand lytic bone metastases. Protocol 19Aredia Breast Study group. N Engl J Med335:1785-1791, 1996.
4.
Roodman GD: Biology of osteoclast activationin cancer. J Clin Oncol 19:3562-3571,2001.
5.
Lipton A: Bisphosphonates and metastaticbreast cancer. Cancer 97(3 suppl):848-853,2003.
6.
Solomayer EF, Diel IJ, Meyberg GC, etal: Metastatic breast cancer: Clinical course,prognosis, and therapy related to the first site ofmetastasis. Breast Cancer Res Treat 59:271-278, 2000.
7.
Coleman RE, Rubens RD: The clinicalcourse of bone metastases from breast cancer.Br J Cancer 55:61-66, 1987.
8.
Colleoni M, O’Neill A, Goldhirsch A, etal: Identifying breast cancer patients at highrisk for bone metastases. J Clin Oncol 18:3925-3935, 2000.
9.
Carlin BI, Andriole GL: The natural history,skeletal complications, and managementof bone metastases in patients with prostatecarcinoma. Cancer 88(12 suppl):2989-2994,2000.
10.
Dawson NA: Bisphosphonates: Theirevolving role in the management of prostatecancer-related bone disease. Curr Opin Urol12:413-428, 2002.
11.
Berruti A, Dogliotti L, Bitossi R, et al:Incidence of skeletal complications in patientswith bone metastatic prostate cancer and hormonerefractory disease: Predictive role of boneresorption and formation markers evaluated atbaseline. J Urol 164:1248-1253, 2000.
12.
Saad F, Gleason DM, Murray R, et al: Arandomized, placebo-controlled trial ofzoledronic acid in patients with hormone-refractorymetastatic prostate carcinoma. J NatlCancer Inst 94:1458-1468, 2002.
13.
Croucher PI, Apperley JF: Bone diseasein multiple myeloma. Br J Haematol 103:902-910, 1998.
14.
Croucher PI, Shipman CM, Lippitt J, etal: Osteoprotegerin inhibits the development ofosteolytic bone disease in multiple myeloma.Blood 98:3534-3540, 2001.
15.
Giuliani N, Bataille R, Mancini C, et al:Myeloma cells induce imbalance in the osteoprotegerin/osteoprotegerin ligand system inthe human bone marrow environment. Blood98:3527-3533, 2001.
16.
Quint LE, Tummala S, Brisson LJ, et al:Distribution of distant metastases from newlydiagnosed non-small cell lung cancer. Ann ThoracSurg 62:246-250, 1996.
17.
Wallmeroth A, Wagner U, Moch H, etal: Patterns of metastasis in muscle-invasivebladder cancer (pT2-4): An autopsy study on367 patients. Urol Int 62:69-75, 1999.
18.
Koga S, Tsuda S, Nishikido M, et al:The diagnostic value of bone scan in patientswith renal cell carcinoma. J Urol 166:2126-2128, 2001.
19.
Koeneman KS, Yeung F, Chung LW:Osteomimetic properties of prostate cancer cells:A hypothesis supporting the predilection ofprostate cancer metastasis and growth in thebone environment. Prostate 39:246-261, 1999.
20.
Diel IJ, Solomayer EF, Seibel MJ, et al:Serum bone sialoprotein in patients with primarybreast cancer is a prognostic marker forsubsequent bone metastasis. Clin Cancer Res5:3914-3919, 1999.
21.
Shariat SF, Shalev M, Menesses-Diaz A,et al: Preoperative plasma levels of transforminggrowth factor beta1 (TGF-b1) strongly predictprogression in patients undergoing radicalprostatectomy. J Clin Oncol 19:2856-2864.
22.
Shariat SF, Andrews B, Kattan MW, etal: Plasma levels of interleukin-6 and its solublereceptor are associated with prostate cancerprogression and metastasis. Urology 58:1008-1015, 2001.
23.
Izumi M, Nakanishi Y, Takayama K, etal: Diagnostic value of bone-turnover metabolitesin the diagnosis of bone metastases inpatients with lung carcinoma. Cancer 91:1487-1493, 2001.
24.
Ryback LD, Rosenthal DI: Radiologicalimaging for the diagnosis of bone metastases.Q J Nucl Med 45:53-64, 2001.
25.
Brown H, Healey JH: Metastatic cancerof the bone, in Devita VT, Hellman S, RosenbergS (eds): Cancer Principles and Practice inOncology, 6th ed, pp 2713-2729. Philadelphia,Lippincott Williams & Wilkins, 2001.
26.
Cordio MA, Snyder BD, Wilson S: Noninvasiveprediction of fracture in patients withmetastatic breast cancer to the spine (abstract).Third North American Symposium on SkeletalComplications of Malignancy, p 44, Bethesda,Md, 2002.
27.
Altehoefer C, Ghanem N, Hogerle S, etal: Comparative detectability of bone metastasesand impact on therapy of magnetic resonanceimaging and bone scintigraphy in patients withbone metastases. Eur J Radiol 40:16-23, 2001.
28.
Lu C, Stomper PC, Drislane FW, et al:Suspected spinal cord compression in breastcancer patients: A multidisciplinary risk assessment.Breast Cancer Res Treat 51:121-131,1998.
29.
Mirels H: Metastatic disease in longbones. A proposed scoring system for diagnosingimpending pathologic fractures. Clin Orthop249:256-264, 1989.
30.
Giunto A, Lijoi F, Innao V: The surgicaltreatment of bone metastases. Ital J OrthopTraumato 8:245-255, 1982.
31.
Colyer RA: Surgical stabilization ofpathological neoplastic fractures. Curr ProblCancer 10:117-168, 1986.
32.
Wirbel RJ, Mutschler WE: Surgical therapyof bone metastases. Zentralbl Chir 120:707-715, 1995.
33.
Friedl W: Indication, management andresults of surgical treatment of surgical therapyfor pathological fractures in patients with bonemetastases. Eur J Surg Oncol 16:380-396, 1990.
34.
Healey JH, Brown HK: Complicationsof bone metastases: Surgical management. Cancer88(12 suppl): 2940-2951, 2000.
35.
Sabato S, Stein H: The surgical managementof pathological fractures. Int Orthop 7:65-68, 1983.
36.
Habermann ET, Sachs R, Stern RE, et al:The pathology and treatment of metastatic diseaseof the femur. Clin Orthop 169:70-82, 1982.
37.
Sattel W, Schneider J, Hartog C: Operativetreatment of metastasis related pathologicand incipient fractures of the extremities. ZentralblChir 109:418-427, 1984.
38.
Jeremic B: Single fraction external-beamradiation therapy in the treatment of localizedmetastatic bone pain. A review. J Pain SymptomManage 22:1048-1058, 2001.
39.
Wu JS, Whelan T, Bezjak A, et al: Metaanalysisof single-fraction versus multi-fractionradiotherapy trials for palliation of painfulbone metastases. Int J Radiat Oncol Biol Phys51(suppl 1):53, 2001.
40.
Coleman RE: Management of bone metastases.Oncologist 5:463-470, 2000.
41.
Vinholes JJ, Purohit OP, Abbey ME, etal: Relationships between biochemical andsymptomatic response in a double-blind randomizedtrial of pamidronate for metastatic bonedisease. Ann Oncol 8:1243-1250, 1997.
42.
Green JR, Rogers MJ: Pharmacologicprofile of zoledronic acid: A highly potent inhibitorof bone resorption. Drug Dev Res55:210-224, 2002.
43.
Green J: Anti-tumor effects of bisphosphonates.Cancer 97(3 suppl):840-847, 2003.
44.
Clohisy DR, Mantyh: Bone cancer pain.Cancer 97(3 suppl):866-873, 2003.
45.
Medhurst SJ, Walker K, Bowes M, et al:A rat model of bone cancer pain. Pain 96:129-40, 2002.
46.
Padalecki SS, Carreon M, Grubbs B:Androgen deprivation enhances bone loss andprostate cancer metastases to bone: Preventionby zoledronic acid (abstract). Third North AmericanSymposium on Skeletal Complications ofMalignancy, p 34, Bethesda, Md, 2002.
47.
Lin JH: Bisphosphonates: A review oftheir pharmacokinetic properties. Bone 18:75-85, 1996.
48.
Chen T, Berbson J, Vescio R, et al:Pharmacokinetics and pharmacodynamics ofzoledronic acid in cancer patients with bonemetastases. J Clin Pharmacol 42:1228-1236,2002.
49.
Rosen LS, Gordon D, Kaminski M, et al:Zoledronic acid versus pamidronate in the treatmentof skeletal metastases in patients withbreast cancer or osteolytic lesions of multiplemyeloma: A phase III, double-blind, comparativetrial. Cancer J 7:377-387, 2001.
50.
Bernardo MV, Harrington DP: Samplesize calculations for the two-sample problemusing the multiplicative intensity model. StatMed 20:557-79, 2001.
51.
Theriault RL, Lipton A, Hortobagyi GN,et al: Pamidronate reduces skeletal morbidityin women with advanced breast cancer andlytic bone lesions: A randomized, placebo-controlledtrial. Protocol 18 Aredia Breast CancerStudy Group. J Clin Oncol 17:846-854, 1999.
52.
Hillner BE, Ingle JN, Berenson JR, et al:American Society of Clinical Oncology guidelineon the role of bisphosphonates in breastcancer. American Society of Clinical OncologyBisphosphonates Expert Panel. J Clin Oncol18:1378-1391, 2000.
53.
Rosen L, Gordon DH, Dugan W Jr, et al:Zoledronic acid (4 mg) is more effective thanpamidronate (90 mg) for treating bone metastasesin breast cancer patients with at leastone osteolytic lesion (abstract 629). Presentedat the 27th European Society for Medical OncologyCongress, Nice, France, 2002.
54.
Coleman RE, Rosen LS, Gordon D, etal: Zoledronic acid (4 mg) significantly reducesthe relative risk of developing a skeletalrelatedevent compared with pamidronate (90mg) in patients with breast cancer and bonemetastasis (abstract). Presented at the 25th AnnualSan Antonio Breast Cancer Symposium,San Antonio, Tex, 2002.
55.
Small E, Smith M, Seaman J, et al: Amulticenter study of pamidronate disodium forthe palliation of bone pain in patients withadvanced prostate cancer. J Clin Oncol. In press.
56.
Smith MR, McGovern FJ, Zietman AL,et al: Pamidronate to prevent bone loss duringandrogen-deprivation therapy for prostate cancer.N Engl J Med 345:948-955, 2001.
57.
Rosen L, Gordon D, Tchekmedyian S, etal: Zoledronic acid (Zol) significantly reducesskeletal-related events (SREs) in patients withbone metastases from solid tumors (abstract1179). Proc Am Soc Clin Oncol 21:295a, 2002.
58.
Twycross RG: Management of pain inskeletal metastases. Clin Orthop 312:187-196,1995.
59.
Maxwell T, Givant E, Kowalski MO:Exploring the management of bone metastasisaccording to the Roy Adaptation Model. OncolNurs Forum 28:1173-1181, 2001.
60.
Gerber L, Hicks J, Shah J: Rehabilitationof the cancer patient, in DeVita VT, Hellman S,Rosenberg S (eds): Cancer Principles and Practicein Oncology, 6th ed, ch 57. Philadelphia,Lippincott Williams & Wilkins, 2001.
61.
Body JJ, Lossignol D, Ronson A: Theconcept of rehabilitation of cancer patients. CurrOpin Oncol 9:332-340, 1997.
Oncology Peer Review On-The-Go: Cancer-Related Fatigue Outcome Measures in Integrative Oncology
September 20th 2022Authors Dori Beeler, PhD; Shelley Wang, MD, MPH; and Viraj A. Master, MD, PhD, spoke with CancerNetwork® about a review article on cancer-related fatigue published in the journal ONCOLOGY®.