Neoadjuvant Chemoradiation for Rectal Cancer: Is More Better?
Neoadjuvant chemoradiation has become the favored adjuvant treatment for stages II and III rectal cancer. Compared to postoperative chemoradiation, this modality of treatment has been shown to be superior in terms of toxicity, local relapse, and sphincter-saving.[1] This article will focus on the evolution of neoadjuvant chemotherapy over the past 2 decades, current acceptable neoadjuvant standards, and current investigational regimens.
ABSTRACT: Neoadjuvant chemoradiation is now considered the clear preferable adjuvant standard of care in the management of stage II/III rectal cancer. Neoadjuvant fluorouracil (5-FU) plus radiation results in a decrease in local relapse rates and a favorable toxicity profile in comparison with postoperative adjuvant 5âFU plus radiation therapy. Recent nonrandomized comparative studies have shown that capecitabine (Xeloda) plus radiation result in downstaging and pathologic complete responses equivalent to those of 5-FU plus radiation, making this combination an acceptable alternative neoadjuvant treatment. The addition of oxaliplatin (Eloxatin) or irinotecan (Camptosar) to 5-FU or capecitabine concurrently with radiation therapy appears to result in more favorable pathologic responses in phase I/II trials. These combinations should be investigated further in larger phase III studies before they are endorsed in the routine neoadjuvant treatment of rectal cancer. This article will review the progress of chemoradiation over the past 2 decades, current standards of care, and investigational treatments in the neoadjuvant treatment of rectal cancer.
Neoadjuvant chemoradiation has become the favored adjuvant treatment for stages II and III rectal cancer. Compared to postoperative chemoradiation, this modality of treatment has been shown to be superior in terms of toxicity, local relapse, and sphincter-saving.[1] This article will focus on the evolution of neoadjuvant chemotherapy over the past 2 decades, current acceptable neoadjuvant standards, and current investigational regimens.
Neoadjuvant Radiation for Rectal Cancer
In the Pre–Total Mesorectal Excision Era
While adjuvant radiation therapy (RT) has never been shown to improve overall survival, there is evidence-at least from the pre–total mesorectal excision (TME) era-that neoadjuvant RT improves both local control rates and overall survival.[2-6]
A Swedish rectal cancer trial randomly assigned 1,168 patients with resectable rectal cancer to undergo preoperative irradiation (5 Gy/fraction × 5 days) followed by surgery within 1 week or to undergo surgery only.[6] The preoperative RT arm showed a significant decrease in local relapse (11% vs 27%, P < .001) and improvement in the 5-year survival rate (58% vs 48%, P = .004). A recent update of this study confirmed that the survival benefits seen with neoadjuvant radiation persisted at 13 years.[7] The survival advantage of neoadjuvant radiation therapy in rectal cancer has been confirmed by two independent meta-analyses, both of which included 14 randomized trials and close to 6,000 patients.[8,9]
In contrast, randomized studies and one meta-analysis of adjuvant radiation studies failed to show any improvement in survival in patients receiving postoperative radiation vs surgery only.[3,4,9,10]
A randomized phase III study comparing neoadjuvant RT to adjuvant RT for stage II/III rectal cancer lends further support to a neoadjuvant radiation strategy. In this study, 471 patients were randomized to receive either preoperative short-term radiation (25.5 Gy in 1 week) or prolonged postoperative radiation (60 Gy in 7 to 8 weeks). After a minimum follow-up of 5 years, investigators found a significant decrease in the local relapse rate in favor of the preoperative RT arm (13% vs 22%, P = .02) but no overall survival benefit.[5]
To summarize, the historic data from the pre-TME era supports the use of neoadjuvant radiation in patients with rectal cancer. However, evidence is inadequate to support a survival impact for single-modality adjuvant radiation therapy.
In the Total Mesorectal Excision Era
Total mesorectal resection requires sharp dissection beyond the plane of the mesorectum, thus permitting en bloc removal of intact tumor with its lymphatics and vascular supply. This technique is more likely to result in a negative circumferential margin and is now endorsed as the standard of care for rectal cancer surgery. In contrast with blunt dissection, TME is associated with low local relapse rates of up to 8% in patients with stage II/III rectal cancer.[11-15]
Given the low relapse rates with TME, two large trials have explored the role of preoperative radiotherapy in this setting.[16,17] A Dutch study randomized 1,861 patients with rectal cancer to receive neoadjuvant RT (5 Gy × 5) followed by TME vs TME alone to assess the impact of neoadjuvant RT on recurrence rate and overall survival. The rate of local relapse at 2 years was 2.4% in the radiotherapy-plus-surgery group and 8.2% in the surgery-only group (P < .001). Neoadjuvant RT did not affect the risks of distant relapse or overall survival.[16] A subgroup post hoc analysis of this study suggested that there was no benefit from RT in patients with stage I disease or with proximal T3, N0 tumors.[16] This study highlights the value of neoadjuvant RT in patients with stage II/III rectal cancer-despite the routine integration of TME in surgical management.
The second trial, the Medical Research Council (MRC) CR07, randomized 1,350 patients with clinically resectable rectal cancer to short-course preoperative radiation therapy (5 Gy × 5) and TME vs TME followed by selective postoperative chemoradiation for patients with a positive circumferential margin (45 Gy in 25 fractions plus fluorouracil [5-FU]). Preliminary results presented at the 2006 annual meeting of the American Society of Clinical Oncology showed a significant decrease in local relapse (4.7% vs 11.1%) and an improved 3-year disease-free survival (79.5% vs 74.9%) in favor of the preoperative RT arm.[17]
This study further confirms that preoperative RT is favored over postoperative chemoradiation in patients with high-risk disease. Also of note, unlike the Dutch trial, MRC CR07 patients with proximal lesions had a significant decrease in local relapse when receiving preoperative RT. No data were presented on the impact of preoperative chemoradiation on the T3, N0 proximal tumor subgroup.
Neoadjuvant Chemoradiation for Rectal Cancer
5-FU Plus RT
Interest in the use of neoadjuvant 5-FU plus radiation stemmed from adjuvant chemoradiation studies of rectal cancer. A randomized adjuvant clinical trial confirmed an improvement in local relapse rates with a survival benefit in favor of 5-FU–based RT in comparison with RT alone.[10] A subsequent randomized adjuvant chemoradiation study reported a disease-free and overall survival advantage favoring protracted continuous-infusion 5-FU over bolus 5-FU with RT.[18] However, an intergroup study showed no advantage for protracted continuous-infusion 5-FU plus RT over bolus 5-FU/leucovorin (LV) plus RT.[19] Thus, current adjuvant 5-FU–based chemoradiation regimens incorporate either continuous-infusion 5-FU or 5-FU and leucovorin.
FIGURE 1

Design of NSABP-R04 Trial
Neoadjuvant 5-FU–based chemoradiation regimens have been largely extrapolated from prior adjuvant studies. Protracted 5-FU infusion regimens (300 mg/m2/d on radiation days or 225 mg/m2/d including weekends) have been shown to have significant antitumor activity and are commonly implemented in clinical practice in the United States.[20,21] Neoadjuvant bolus 5-FU and leucovorin plus RT (5-FU/LV 350/20 mg/m2/d mg/m2/d including weekends) have been shown to have significant antitumor activity and are adjuvant studies. Protracted 5-FU infusion regimens (300 mg/m2/d on radiation days or 225 Neoadjuvant 5-FU–based chemoradiation regimens have been largely extrapolated from prior × 5 days on weeks 1 and 5 of RT) was developed at Memorial Sloan-Kettering Cancer Center and was similarly associated with favorable antitumor activity and toxicity profile.[22] Both continuous and bolus 5-FU/LV–based chemoradiation were given concurrently with 45 to 50.4 Gy of radiation. The ongoing National Surgical Adjuvant Breast and Bowel Project (NSABP)-R04 neoadjuvant rectal cancer trial has endorsed 5-FU at 225 mg/m2/d with RT at 50.4 Gy as its standard control arm (Figure 1).
Neoadjuvant 5-FU/LV Plus RT vs RT Alone
5-FU–based chemoradiation compares favorably to RT alone in the neoadjuvant treatment of rectal adenocarcinoma. A large phase III French study, Fdration Francophone de Cancrologie Digestive (FFCD) 9203, randomized patients with stage II/III rectal cancer to receive RT alone (45 Gy in 25 fractions) or 5-FU/LV with RT (FU/LV 350/20 mg/m2/d on days 1 to 5 and 29 to 33 of RT).[23] Patients in both arms subsequently underwent surgery and four cycles of 5-FU/LV. The preoperative chemoradiation arm showed a significant improvement in pathologic complete response (pCR) rate (11.4% vs 3.6%, P < .05) and local relapse rate (8.1 vs 16.5%, P < .05). The 5-year survival in both arms was 67%.[23]
Another large phase III study, European Organisation for Research and Treatment of Cancer (EORTC) 22921, randomized patients with stage II/III rectal cancer to receive neoadjuvant RT alone (45 Gy in 25 fractions) vs RT with bolus 5-FU/LV (350/20 mg/m2/d during the first and fifth weeks of preoperative RT), with a subsequent randomization to postsurgical (3 to 10 weeks after chemoradiation) 5-FU/LV chemotherapy or no postsurgical chemotherapy.[24] The study demonstrated no significant difference in overall survival between the groups that received chemotherapy preoperatively and those who received it postoperatively. The 5-year cumulative incidence rates for local relapse were 8.7%, 9.6%, and 7.6% in the groups receiving chemotherapy preoperatively, postoperatively, or both, respectively, and 17.1% in the group that did not receive chemotherapy (P = .002).The authors concluded that in patients with rectal cancer who receive preoperative radiotherapy, adding 5-FU–based chemotherapy either preoperatively or postoperatively conferred a significant advantage in terms of local control.[24]
Neoadjuvant 5-FU/RT vs Adjuvant 5-FU/RT
The German Rectal Cancer Study Group randomly assigned 823 patients with clinical stage T3 or T4 or node-positive disease to receive either preoperative or postoperative chemoradiotherapy.[1] Radiation therapy was delivered at 50.4 Gy, with an additional 5.4 Gy delivered as a boost in the postoperative arm. 5-FU was given in a 120-hour continuous intravenous infusion at a dose of 1,000 mg/m2/d during the first and fifth weeks of RT. Surgery (TME) was performed 6 weeks after the completion of chemoradiotherapy. At 1 month after surgery, four 5-day monthly cycles of 5-FU (500 mg/m2/d) were given.
The results from this study showed a significantly lower 5-year cumulative incidence of local relapse in favor of the preoperative treatment group (6% vs 13%). The 5-year disease-free (68% vs 65 %) and overall survival rates (76% vs 74%) were similar for preoperative and postoperative therapy and the differences between the groups were not statistically significant. Significant tumor downstaging was seen after preoperative combined-modality treatment, with an 8% pCR rate. Posttrial review showed that sphincter-saving surgeries were more likely to occur in the neoadjuvant chemoradiation group than in the adjuvant group (39% vs 19%, P = .004).
Furthermore, acute and delayed grade 3/4 toxicities were less frequent in the preoperative group (27% vs 40%).[1] Despite the lack of survival advantage, the improvements in local relapse rate and toxicity profiles have clearly established neoadjuvant chemoradiation as the standard adjuvant modality in rectal cancer.
Capecitabine Plus RT
Capecitabine (Xeloda) is an oral, tumor-activated fluoropyrimidine carbamate that delivers 5-FU preferentially to tumor cells via a three-step in vivo enzymatic conversion. The final step is mediated by the enzyme thymidine phosphorylase, which is upregulated in tumor tissue compared with adjacent healthy tissue.[25] This also gives capecitabine a theoretical advantage of differential radiosensitization in the tumor, sparing normal tissues.[26] The equivalence of capecitabine to intravenous 5-FU/LV in the treatment of metastatic colorectal cancer has led to its incorporation in the chemoradiation of rectal cancer.[27-31] The advantages of capecitabine over 5-FU include its ease of administration and its favorable toxicity profile.[32]
TABLE 1
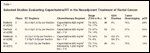
Selected Studies Evaluating Capecitabine/RT in the Neoadjuvant Treatment of Rectal Cancer
Dunst et al evaluated the combination of capecitabine and radiotherapy in a phase I clinical trial. Capecitabine at 825 g/m2 twice daily (including weekends) concurrently with 50.4 Gy was determined as the recommended dose with promising efficacy results.[33] Several phase II clinical trials have evaluated this dose and schedule in patients with stage II/III rectal cancer and have shown pCR rates ranging from 12% to 24% (Table 1).[34-37]
There are no efficacy data available from randomized clinical trials comparing capecitabine/RT with 5-FU/RT in the neoadjuvant setting in locally advanced rectal cancer. However, two well-conducted retrospective studies have evaluated the efficacy of capecitabine/RT with 5-FU/RT in locally advanced rectal cancer with comparable response and overall survival rates.[38,39] Kim et al compared 145 patients who received either 5-FU/LV (5-FU at 400 mg/m2/d with LV at 20 mg/m2/d for 3 days in the first and fifth weeks of RT), to 133 patients receiving capecitabine (825 mg/m2 twice daily for the duration of RT), both with concurrent RT (50.4 Gy in 28 fractions).[39] Comparable downstaging (5-FU/LV: 44.3%, capecitabine: 49.9%; P = .571) and pCR rates (5-FU/LV: 11.3%, capecitabine: 16.1%; P = .758) were noted.[38]
Das et al compared outcomes in 89 patients receiving capecitabine at 1,650 mg/m2/d concurrently with RT (45 Gy) and 87 patients receiving protracted infusional 5-FU (300 mg/m2/d).[39] No significant differences in pCR (21% vs 12%, P = .19) or downstaging (52% vs 62%, P = .20) were seen for capecitabine and 5-FU, respectively. Local relapse, distant control, and overall survival were similar across both arms.[39]
The randomized phase III NSABP-R04 study (Figure 1) is currently comparing capecitabine/RT to 5-FU/RT (with and without concurrent oxaliplatin [Eloxatin]). This will help determine if capecitabine can substitute for 5-FU in the neoadjuvant treatment of rectal cancer.
Oxaliplatin/5-FU Plus RT
Significant interest has arisen in the past several years in developing combinations of 5-FU, oxaliplatin, and RT in the neoadjuvant treatment of rectal cancer. This interest has been supported by the systemic synergistic activity between oxaliplatin and fluoropyrimidines and the added radiation-sensitizing activity of oxaliplatin.[40,41]
The Cancer and Leukemia Group B (CALGB) investigated a combination of escalating weekly doses of oxaliplatin in combination with continuous-infusion 5-FU at 200 mg/m2/d and radiation therapy at 1.8 Gy/fraction for a total of 50.4 Gy in a phase I/II study.[42] The recommended phase II dose of oxaliplatin in this combination was identified as 60 mg/m2/wk (in six doses).[42] Among 32 patients treated at the recommended dose, 25% had a pCR. However, this was associated with an excessive rate of grade 3/4 diarrhea (38%).
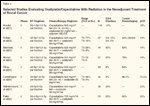
TABLE 2

Selected Studies Evaluating Oxaliplatin/5-FU With Radiation in the Neoadjuvant Treatment of Rectal Cancer
patients with T3/4 or N+ rectal cancer.[43] Two doses of 5-FU were investigated (200 and 225 In Europe, Aschele et al conducted a similar phase I/II study of 5-FU, oxaliplatin, and RT in mg/m2/d) concurrently with escalating doses of weekly oxaliplatin × 6 and a fixed dose of radiation at 50.4 Gy in 28 fractions. The recommended dose of this combination was in line with the CALGB study (5-FU at 225 mg/m2/d concurrently with oxaliplatin at 60 mg/m2/wk × 6 plus radiation therapy). This recommended dose was associated with a grade 3/4 diarrhea rate of 16% and a pCR rate of 28%.[43]
Other studies have evaluated variant schedules of concurrent oxaliplatin/bolus 5-FU and radiation in the neoadjuvant setting (Table 2).[42-45] These regimens have been associated with increased toxicity and a generally less impressive pCR rate of 7% to 8%.
The randomized NSABP-R04 trial is currently addressing the value of adding oxaliplatin to 5-FU radiation therapy (Figure 1).
Oxaliplatin/Capecitabine Plus RT
Capecitabine/oxaliplatin combinations have demonstrated efficacy and tolerability comparable to that of 5-FU/oxaliplatin in the first-line treatment of metastatic colorectal cancer.[41,46-49] Several studies have investigated the combination of capecitabine, oxaliplatin, and radiation in the neoadjuvant treatment of rectal cancer in hopes of improving both local and systemic disease control.
In a phase I/II study, daily capecitabine (including weekends) was combined with a fixed dose of oxaliplatin at 130 mg/m2 on days 1 and 29 concurrently with RT 45 Gy (25 fractions) in patients with borderline or unresectable rectal cancer. The maximum tolerated dose of capecitabine in this combination was 650 mg/m2 twice daily.[50] A total of 96 patients were enrolled across the phase I and II portions of this study. Among the patients undergoing surgery, 75 (88%) had R0 resection with 16 (19%) resected specimens showing a pCR. Only 21 patients (22%) experienced grade 3/4 adverse events, the most common being gastrointestinal.
Roedel et al conducted a phase II neoadjuvant study of capecitabine and oxaliplatin (XELOX) plus radiation in 110 patients with locally advanced rectal cancer.[51] The regimen consisted of capecitabine at 825 mg/m² twice daily on days 1 to 14 and 22 to 35 along with oxaliplatin 50 mg/m² on days 1, 8, 22, and 29, plus RT (50.4 Gy in 28 fractions). TME was scheduled 4 to 6 weeks after completion of preoperative XELOX/RT. Full-dose preoperative chemoradiation was administered to 90% of patients. Grade 3 toxicity, mainly diarrhea, occurred in 14% of patients. The R0 resection rate was 97%, with 15% of resected specimens showing a pCR.
TABLE 3
Selected Studies Evaluating Oxaliplatin/Capecitabine With Radiation in the Neoadjuvant Treatment or Rectal Cancer
The Capecitabine Oxaliplatin Radiotherapy and Excision (CORE) study investigated a variant regimen of capecitabine twice daily on Mondays through Fridays and weekly oxaliplatin at 50 mg/m2 concurrently with radiation at 45 Gy in patients with threatened or positive circumferential margins by magnetic resonance imaging. Initial results from this multicenter phase II study showed an R0 resection rate of 67% and a pCR rate of 13%.[52] Other researchers have investigated a capecitabine/oxaliplatin regimen similar to the one used in the CORE study (Table 3).[53-57] These studies were associated with pCR rates of 14% to 24%, tumor-downstaging rates of 52% to 78%, and grade 3/4 diarrhea rates of 8% to 30%.
The current recommended dose for capecitabine given twice daily on radiation days with weekly oxaliplatin and RT (1.8 Gy × 25–28 fractions) is 825 mg/m2 twice daily and 50 mg/m2 weekly for capecitabine and oxaliplatin, respectively. This recommended dose is based on several European studies[52-55,58] and is currently endorsed in the NSABP-R04 study. Of note, the only phase I study of this combination conducted in the United States found this dose to be intolerable secondary to a high rate of grade 3/4 diarrhea.[59] This phase I study established capecitabine at 725 mg/m2 per dose twice daily plus oxaliplatin at 50 mg/m2/wk × 5 concurrently with RT (50.4 in 28 fractions) as the maximum tolerated dose.[59]
The same investigators evaluated this dose in a subsequent neoadjuvant phase II study in patients with stage II and III rectal cancer.[60] An impressive antitumor activity with a pCR of 24% was noted. This was associated with a 20% incidence of grade 3/4 diarrhea.
The recommended doses of capecitabine, oxaliplatin, and radiation therapy may tend to be lower in the United States than in Europe, because higher rates of toxicity have been reported in the US for capecitabine monotherapy or capecitabine/oxaliplatin combinations.[61] The exact etiology for the discrepancy in toxicity at equal capecitabine dosing may be related to increased folic acid supplementation in the American diet. It is prudent at this time to consider 725 mg/m2 twice daily dosing for capecitabine in combination with weekly oxaliplatin (50 mg/m2) and RT (50.4 Gy) in the US until further safety data become available from NSABP-R04. The 825-mg/m2 dose level of capecitabine combined with a similar oxaliplatin/RT regimen is clearly tolerable and feasible in Europe.
Irinotecan/5-FU Plus RT
TABLE 4

Selected Studies Evaluating Irinotecan/5-FU With Radiation in the Neoadjuvant Treatment of Rectal Cancer
Irinotecan (Camptosar), a topoisomerase I inhibitor, is an active agent in the treatment of metastatic colorectal cancer, whether used as monotherapy or in combination with other agents.[62-68] Given its systemic and radiosensitizing activities, irinotecan has been incorporated in the neoadjuvant treatment of rectal cancer (Table 4).[69-73]
In a phase I/II study, Mitchell et al evaluated a weekly irinotecan regimen in combination with 5-FU and concurrent pelvic radiation.[69] Patients with primary or recurrent clinical stage T3/4 adenocarcinoma of the rectum received escalating doses of weekly irinotecan (30 to 50 mg/m2) in combination with continuous-infusion 5-FU and concurrent RT (50.4 Gy). Surgery was performed 8 to 10 weeks after the completion of therapy. The maximum tolerated dose in this study was identified as irinotecan at 50 mg/ m2 in combination with 5-FU at 225 mg/ m2/d on radiation days.[69] Of 46 patients undergoing surgery, 11 (24%) demonstrated a complete pathologic response.[69]
In another irinotecan-based neoadjuvant trial, 37 patients were treated with irinotecan at 50 mg/m2/wk and continuous-infusion 5-FU (250 mg/ m2/ d, days 1–43) concurrently with RT (50.4 Gy in 28 fractions). The pCR rate was 22%, tumor-downstaging rate was 75%, and disease-free survival at 40 months was 73%.[70]
The high pCR rate was in line with another phase II trial by Mohiuddin et al.[71] This study evaluated 5-FU plus hyperfractionated RT in comparison with standard RT combined with infusional 5-FU and weekly irinotecan. The irinotecan arm consisted of 5-FU (225 mg/m2/d Mondays through Fridays) plus irinotecan (50 mg/m2/wk) and conventional RT (50.4 Gy for T3 and 54 Gy for T4). The tumor-downstaging rate was 78% and pCR rate was 28%.[71]
A modest pCR rate was described in another study of continuous-infusion 5-FU, irinotecan, and RT.[72] A total of 74 patients with resectable T3/4 rectal cancers received irinotecan (50 mg/ m2/wk) and continuous-infusion 5-FU (225 mg/m2/d) with concurrent RT (45 Gy). Grade 3 neutropenia (7%) and diarrhea (14%) were the main severe toxicities. The pCR rate was 14%, with 49% tumor downstaging.[72]
Irinotecan was also investigated on a daily × 5 schedule in combination with a standard-bolus 5-FU/LV-plus-RT regimen.[23,24] A total of 59 patients were treated with RT (45 Gy), 5-FU/LV (350/20 mg/m2/d) on days 1 to 5 and 29 to 33, and escalating doses of irinotecan (6, 8, 10, 12, 14, 16, 18, and 20 mg/m2/d) on days 1 to 5 and 29 to 33. Irinotecan at 18 mg/m2 was selected as the recommended dose for future studies.[73] A pCR was observed in 12/49 patients (24%) and tumor downstaging in 20/49 patients (41%).
The above studies incorporating irinotecan with 5-FU and radiation appear to show promising results, as seen in the pCR rate and the number of patients who eventually had successful surgery. Nonetheless, toxicity-mainly the occurrence of diarrhea-is of concern.
Irinotecan/Capecitabine Plus RT
The combination of irinotecan, capecitabine, and radiation therapy has been investigated in the neoadjuvant treatment of rectal cancer.
In a phase I study, Hofheinz et al evaluated a weekly regimen of irinotecan in combination with twice-daily capecitabine and radiation therapy. The recommended regimen from this study consisted of capecitabine at 500 mg/m2 twice daily in combination with weekly irinotecan at 50 mg/m2/ wk plus RT (50.4 Gy in 28 fractions). An interesting pCR rate of 4/19 (21%) was seen.[74]
A phase II study further evaluated the safety and efficacy of these dose levels in 36 patients.[75] A pCR was seen in 5 of 34 evaluable patients (15%) and tumor downstaging was confirmed in 18 of 33 patients (55%). Grade 3/4 diarrhea was seen 11% of patients.[75] In another phase I/II study, Klautke et al investigated a regimen of weekly irinotecan at 40 mg/m2 in combination with escalating doses of capecitabine twice daily and concurrent RT (50.4 Gy).[76] The maximum tolerated dose was confirmed at the 750-mg/m2 capecitabine dose level. Four patients (15%) achieved a pCR, while pathologic downstaging was seen in 62%.[76]
TABLE 5

Selected Studies Evaluating Irinotecan/Capecitabine With Radiation in the Neoadjuvant Treatment of Rectal Cancer
Selected studies investigating the combination of preoperative capecitabine and irinotecan concurrent with radiotherapy are summarized in Table 5.[74-79] The average dose of irinotecan during radiotherapy was about 240 to 250 mg/m2. Doses of capecitabine have ranged from 500 mg/m2 twice daily to 750 mg/m2 twice daily.[76] The pCR rate (15%) seems to be comparable among various studies.
No powered head-to-head studies have compared irinotecan- or oxaliplatin-based neoadjuvant chemoradiation studies. In a small neoadjuvant randomized phase II study, similar downstaging was seen for both capecitabine/oxaliplatin– and capecitabine/irinotecan–based neoadjuvant radiation.[80] The irinotecan-based combination was associated with increased diarrhea and chemoradiation-induced fibrosis.[80]
Bevacizumab-Based Chemoradiation
Vascular endothelial growth factor (VEGF) mRNA and protein expression is markedly upregulated in metastatic colon and rectal cancer and is associated with disease progression and inferior survival.[81-83] Bevacizumab (Avastin) increases the response and survival rates in metastatic colorectal cancer when combined with 5-FU/LV–based regimens.[84-88] Based on the improved outcome with the addition of bevacizumab in the metastatic setting and the synergy with radiation therapy in preclinical models, there is a strong rationale for combining antiangiogenic therapy with neoadjuvant chemoradiation therapy in patients with rectal cancer.[89]
The safety of bevacizumab in the neoadjuvant chemoradiation setting was established in a phase I/II study conducted by Willett et al. A total of 22 patients received bevacizumab (5 or 10 mg/kg) every 2 weeks, continuous-infusion 5-FU (225 mg/m2/24 h), and RT (50.4 Gy), followed by surgery in 7 to 9 weeks. Two of the five patients in the cohort receiving bevacizumab at 10 mg/kg with 5-FU plus RT experienced grade 3/4 dose-limiting diarrhea and colitis during treatment. This regimen showed significant downstaging (55%) with a 22% pCR rate. Bevacizumab at 5 mg/kg every 2 weeks in combination with RT plus 5-FU yielded promising results and did not show any dose-limiting toxicity or perioperative morbidity/mortality.[90]
Bevacizumab was also evaluated with capecitabine and either oxaliplatin or irinotecan in a pilot feasibility study.[91] A total of 11 patients with advanced rectal cancer received bevacizumab (5 mg/kg) every 2 weeks with capecitabine (1,000 mg/m2 twice daily on days 1 to 14 before the chemoradiation phase and then 825 mg/m2 twice daily during RT on days 22 to 55) plus irinotecan at 180 mg/m2 (XELIRI) or oxaliplatin at 130 mg/m2 (XELOX) on days 1, 22, 43, and concurrent radiotherapy (54 Gy). Surgery was carried out 8 weeks after the completion of chemoradiation. Only one patient had grade 3 diarrhea and was unable to complete the planned chemotherapy. In combination with XELIRI/XELOX plus RT, bevacizumab neither increased the treatment toxicity profile nor provoked any surgical delay or modifications.[91]
Another phase I trial from Duke University evaluated the combination of concurrent capecitabine, oxaliplatin, and bevacizumab in patients with stage II–IV rectal cancer.[92] A total of 11 patients were treated with escalating doses of capecitabine, oxaliplatin, and a fixed dose of bevacizumab (15 mg/kg on day 1 and 10 mg/kg on days 8 and 22). At dose level 1, patients were treated with oxaliplatin at 50 mg/m2 weekly, capecitabine at 625 mg/m2 twice daily, and concurrent RT (50.4 Gy) without dose-limiting toxicity. At dose level 2 (capecitabine, 825 mg/m2 twice a day), two patients had dose-limiting toxicities of diarrhea and tenesmus-type symptoms. The recommended phase II dose was bevacizumab at 15 mg/kg on day 1 and 10 mg/kg on days 8 and 22, oxaliplatin at 50 mg/m2 weekly, and capecitabine at 625 mg/m2 twice a day on radiation days.[92]
Crane et al reported the preliminary results of a phase II trial in patients with T3/T4 or node-positive rectal cancer receiving preoperative RT (50.4 Gy), every-other-week bevacizumab (5 mg/kg for three doses starting concurrently with RT ), and capecitabine (900 mg/m2 orally twice a day on RT days only), followed by surgery. Among 17 evaluable patients, no grade 3 toxicity was observed. Five patients (29%) achieved a pCR.[93]
These studies suggest that the addition of bevacizumab to chemoradiation is safe and feasible in the neoadjuvant treatment of rectal cancer. Larger studies are needed to investigate whether the addition of this agent results in additional benefits in terms of tumor downstaging or disease-free survival.
Cetuximab Plus Chemoradiation
Cetuximab (Erbitux) is a chimeric monoclonal antibody targeting the epidermal growth factor receptor (EGFR). This agent has significant clinical activity in metastatic colorectal cancer, both as monotherapy or in combination with irinotecan.[94-97]
A pilot study conducted at Memorial Sloan-Kettering Cancer Center investigated the safety of cetuximab in combination with standard neoadjuvant 5-FU and RT in patients with locally advanced or locally recurrent rectal cancer.[98] A total of 20 patients received cetuximab at 400 mg/m2 on day 1 followed by 250 mg/m2/wk × 4, continuous-infusion 5-FU at 225 mg/m2/d over 5.5 weeks, and concurrent pelvic radiation (50.4 Gy). Of the 20 patients enrolled, 18 completed RT and 17 underwent surgery at the time of data-reporting. Approximately 12% of patients had a pCR. Grade 3 diarrhea was seen in 10% of patients.[98]
A Belgian phase I/II trial evaluated a regimen of cetuximab, capecitabine, and RT in 40 patients with endoscopically staged locally advanced rectal cancer. Patients were treated with a loading dose of cetuximab at 400 mg/ m2 the first week followed by 250 mg/m2/wk × 5, escalating doses of capecitabine twice daily, and concurrent RT (45 Gy in 25 fractions). The recommended regimen consisted of capecitabine, 825 mg/m2 twice daily, in combination with cetuximab and RT. This dose level was investigated in 30 patients. Only 2 patients (5%) experienced a pCR. Grade 3 diarrhea occurred in 15% of patients.[99]
Cetuximab has been similarly investigated in irinotecan-based neoadjuvant rectal cancer trials. A German phase I trial investigated a combination of cetuximab, irinotecan, and capecitabine in 20 patients with rectal cancer. Cetuximab was given weekly (400 mg/m2 loading dose followed by 250 mg/m2 on days 8, 15, 22, and 29) and escalating doses of irinotecan and capecitabine with pelvic RT (50.4 Gy). Irinotecan at 40 mg/m2 and capecitabine at 500 mg/m2 twice daily were determined as the recommended doses for future studies. All 20 patients underwent surgery. About 7% of patients (1/14) with T3 disease and 80% (4/5) with T2 disease achieved a pCR.[100]
TABLE 6

Selected Studies Evaluating Cetuximab With Chemoradiation in the Neoadjuvant Treatment of Rectal Cancer
Cetuximab was also investigated in combination with oxaliplatin, capecitabine, and concurrent RT. Rodel et al conducted a phase I/II trial of cetuximab (400 mg/m2 loading dose followed by 250 mg/m2/wk × 5), oxaliplatin 50 mg/m2 weekly, escalating doses of capecitabine (days 1 to 14 and days 22 to 35), and RT (50.4 Gy). The phase II dose was identified at a capecitabine dose level of 1,650 mg/ m2/d on days 1 to 14 and 22 to 35. A total of 48 patients were enrolled on the phase II trial. Tumor downstaging was observed in 21 (47%) patients with pCR in 9% patients. Grade 3-4 diarrhea was seen in 19% patients.[101] Selected cetuximab-based chemoradiation studies are listed in Table 6.[98-101]
Discussion
Neoadjuvant chemoradiation has established itself as the clear preferable standard of care in the management of stage II/III rectal cancer. Infusional 5-FU plus radiation results in improved local relapse rates and decreased toxicity when administered in the preoperative vs postoperative settings.[1] 5-FU plus radiation is the standard established chemoradiation regimen; it is the only combination with a mature efficacy outcome that has been compared to a standard adjuvant regimen.[1] Variations on the 96-hour infusional regimen on weeks 1 and 5 of radiation include protracted continuous-infusion 5-FU or 5-FU/LV bolus and have been extrapolated from prior large adequately powered phase III adjuvant trials.[1,18,19]
The alternative use of capecitabine plus radiation therapy has not yet been proven to be of equal efficacy in large randomized clinical trials. However, two retrospective studies comparing 5-FU– to capecitabine-based RT suggest equal efficacy based on pathologic downstaging and complete pathologic response data.[38,39] This has prompted the National Comprehensive Cancer Network to consider capecitabine/RT as an acceptable neoadjuvant treatment of rectal cancer.[102]
The combination of a fluoropyrimidine plus oxaliplatin and radiation in neoadjuvant treatment has gained considerable interest during the current decade. This combination has the advantage of improving local tumor response and improving systemic targeting of micrometastases. Whether the improved pCR rate seen in numerous oxaliplatin-based phase II trials will translate into improvements in local and distant disease-free survival or sphincter-saving surgeries has yet to be determined. It is hoped that NSABP-R04 will definitively answer these questions in the near future. While clinically attractive, this combination cannot be considered a standard treatment for stage II/III rectal cancer at this time.
The combination of irinotecan, fluoropyrimidine, and radiation has similarly been associated with improved local tumor responses in phase I/II trials. However, this combination may be associated with increased gastrointestinal toxicities. Furthermore, the interest in incorporating irinotecan in colorectal adjuvant studies has diminished, given the negative adjuvant studies incorporating this agent in stage II/III colon cancer.[103,104]
The investigation of bevacizumab and cetuximab in the neoadjuvant treatment of rectal cancer is in its infancy. The combination of these agents with chemotherapy and radiation is clearly feasible. However, there are no strong signals of increased efficacy based on early phase II trials. The addition of bevacizumab to chemoradiation for rectal cancer would definitely carry concerns of increased perforation risk. The addition of anti-EGFR targeted agents would likely increase the risks of diarrhea. The incorporation of these agents and other novel agents in future studies should target populations that are likely to benefit. For example, the recent establishment of monoclonal anti-EGFR resistance in patients with K-ras mutations suggests that these patients should be excluded from future neoadjuvant studies incorporating anti-EGFR agents.[105]
Questions for Future Studies
REFERENCE GUIDE
Therapeutic Agents
Mentioned in This Article
Bevacizumab (Avastin)
Capecitabine (Xeloda)
Cetuximab (Erbitux)
Fluorouracil (5-FU)
Irinotecan (Camptosar)
Leucovorin
Oxaliplatin (Eloxatin)
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
The complexity of neoadjuvant therapy in rectal cancer goes beyond schedule and dosing, and several other issues need to be answered. What is the optimal adjuvant therapy and for how long should it be administered after surgery? Should adjuvant chemotherapy be individualized based on chemoradiation response? Is there a role for neoadjuvant chemotherapy prior to or without neoadjuvant chemoradiation?[106]
While a detailed discussion of these questions is beyond the scope of this article, it is important to stress that neoadjuvant chemoradiation is not a substitute for adjuvant chemotherapy. It is now recognized that even patients with excellent pathologic responses will benefit from postoperative chemotherapy.[107] Patients with pathologic downstaging to yT0–2 were the ones who benefited most from adjuvant 5-FU chemotherapy based on post hoc analysis of a recent phase III study.[107]
The optimal duration of adjuvant treatment following neoadjuvant chemoradiation and surgery is also unclear at this time. Based on extrapolation from other adjuvant trials, 4 months of further adjuvant therapy has been the accepted standard.[19,21] However, the recent incorporation of adjuvant FOLFOX (oxaliplatin, 5-FU, and leucovorin) in the adjuvant treatment of rectal cancer has complicated this issue further.[108] While it may be reasonable to extrapolate to 4 months of postoperative FOLFOX, some have advocated a total of 6 months of oxaliplatin-based adjuvant therapy. The ECOG adjuvant rectal study E5202 has endorsed 6 months of adjuvant treatment.
Future neoadjuvant chemoradiation trials should transition beyond pCR or downstaging and focus on clinically relevant endpoints, namely, relapse, survival, sphincter-saving, and toxicity. After all, more is not always better!
Disclosures:
Financial Disclosure: Dr. Fakih has received honoraria for lecturing/educational activities from Sanofi-Aventis and ImClone.
References:
References
1. Sauer R, Becker H, Hohenberger W, et al: Preoperative vs postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:1731-1740, 2004.
2. Balslev I, Pedersen M, Teglbjaerg PS, et al: Postoperative radiotherapy in Dukes’ B and C carcinoma of the rectum and rectosigmoid. A randomized multicenter study. Cancer 58:22-28, 1986.
3. Fisher B, Wolmark N, Rockette H, et al: Postoperative adjuvant chemotherapy or radiation therapy for rectal cancer: Results from NSABP protocol R-01. J Natl Cancer Inst 80:21-29, 1988.
4. Gastrointestinal Tumor Study Group: Prolongation of the disease-free interval in surgically treated rectal carcinoma. N Engl J Med 312:1465-1472, 1985.
5. Frykholm GJ, Glimelius B, Pahlman L: Preoperative or postoperative irradiation in adenocarcinoma of the rectum: Final treatment results of a randomized trial and an evaluation of late secondary effects. Dis Colon Rectum 36:564-572, 1993.
6. Improved survival with preoperative radiotherapy in resectable rectal cancer. Swedish Rectal Cancer Trial. N Engl J Med 336:980-987, 1997.
7. Folkesson J, Birgisson H, Pahlman L, et al: Swedish Rectal Cancer Trial: Long lasting benefits from radiotherapy on survival and local recurrence rate. J Clin Oncol 23:5644-5650, 2005.
8. Camma C, Giunta M, Fiorica F, et al: Preoperative radiotherapy for resectable rectal cancer: A meta-analysis. JAMA 284:1008-1015, 2000.
9. Adjuvant radiotherapy for rectal cancer: A systematic overview of 8,507 patients from 22 randomised trials. Lancet 358:1291-1304, 2001.
10. Krook JE, Moertel CG, Gunderson LL, et al: Effective surgical adjuvant therapy for high-risk rectal carcinoma. N Engl J Med 324:709-715, 1991.
11. MacFarlane JK, Ryall RD, Heald RJ: Mesorectal excision for rectal cancer. Lancet 341:457-460, 1993.
12. Tocchi A, Mazzoni G, Lepre L, et al: Total mesorectal excision and low rectal anastomosis for the treatment of rectal cancer and prevention of pelvic recurrences. Arch Surg 136:216-220, 2001.
13. Bolognese A, Cardi M, Muttillo IA, et al: Total mesorectal excision for surgical treatment of rectal cancer. J Surg Oncol 74:21-23, 2000.
14. Heald RJ, Moran BJ, Ryall RD, et al: Rectal cancer: The Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg 133:894-899, 1998.
15. McAnena OJ, Heald RJ, Lockhart-Mummery HE: Operative and functional results of total mesorectal excision with ultra-low anterior resection in the management of carcinoma of the lower one-third of the rectum. Surg Gynecol Obstet 170:517-521, 1990.
16. Kapiteijn E, Marijnen CA, Nagtegaal ID, et al: Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345:638-646, 2001.
17. Sebag-Montefiore D, Steele R, Quirke P, et al: Routine short course pre-op radiotherapy or selective post-op chemoradiotherapy for resectable rectal cancer? Preliminary results of the MRC CR07 randomised trial (abstract 3511). J Clin Oncol 24(18S):148s, 2006.
18. O’Connell MJ, Martenson JA, Wieand HS, et al: Improving adjuvant therapy for rectal cancer by combining protracted-infusion fluorouracil with radiation therapy after curative surgery. N Engl J Med 331:502-507, 1994.
19. Smalley SR, Benedetti JK, Williamson SK, et al: Phase III trial of fluorouracil-based chemotherapy regimens plus radiotherapy in postoperative adjuvant rectal cancer: GI INT 0144. J Clin Oncol 24:3542-3547, 2006.
20. Janjan NA, Crane CN, Feig BW, et al: Prospective trial of preoperative concomitant boost radiotherapy with continuous infusion 5-fluorouracil for locally advanced rectal cancer. Int J Radiat Oncol Biol Phys 47:713-718, 2000.
21. Tepper JE, O’Connell M, Niedzwiecki D, et al: Adjuvant therapy in rectal cancer: analysis of stage, sex, and local control-final report of intergroup 0114. J Clin Oncol 20:1744-1750, 2002.
22. Minsky BD, Cohen AM, Enker WE, et al: Preoperative 5-FU, low-dose leucovorin, and radiation therapy for locally advanced and unresectable rectal cancer. Int J Radiat Oncol Biol Phys 37:289-295, 1997.
23. Gerard JP, Conroy T, Bonnetain F, et al: Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3-4 rectal cancers: Results of FFCD 9203. J Clin Oncol 24:4620-4625, 2006.
24. Bosset JF, Calais G, Mineur L, et al: Enhanced tumorocidal effect of chemotherapy with preoperative radiotherapy for rectal cancer: preliminary results-EORTC 22921. J Clin Oncol 23:5620-5627, 2005.
25. Miwa M, Ura M, Nishida M, et al: Design of a novel oral fluoropyrimidine carbamate, capecitabine, which generates 5-fluorouracil selectively in tumours by enzymes concentrated in human liver and cancer tissue. Eur J Cancer 34:1274-1281, 1998.
26. Schuller J, Cassidy J, Dumont E, et al: Preferential activation of capecitabine in tumor following oral administration to colorectal cancer patients. Cancer Chemother Pharmacol 45:291-297, 2000.
27. Van Cutsem E, Hoff PM, Harper P, et al: Oral capecitabine vs intravenous 5-fluorouracil and leucovorin: Integrated efficacy data and novel analyses from two large, randomised, phase III trials. Br J Cancer 90:1190-1197, 2004.
28. Cassidy J, Twelves C, Van Cutsem E, et al: First-line oral capecitabine therapy in metastatic colorectal cancer: A favorable safety profile compared with intravenous 5-fluorouracil/leucovorin. Ann Oncol 13:566-575, 2002.
29. Scheithauer W, Kornek GV, Raderer M, et al: Randomized multicenter phase II trial of two different schedules of capecitabine plus oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol 21:1307-1312, 2003.
30. Twelves C, Wong A, Nowacki MP, et al: Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med 352:2696-2704, 2005.
31. Hoff PM, Ansari R, Batist G, et al: Comparison of oral capecitabine vs intravenous fluorouracil plus leucovorin as first-line treatment in 605 patients with metastatic colorectal cancer: Results of a randomized phase III study. J Clin Oncol 19:2282-2292, 2001.
32. Van Cutsem E, Twelves C, Cassidy J, et al: Oral capecitabine compared with intravenous fluorouracil plus leucovorin in patients with metastatic colorectal cancer: Results of a large phase III study. J Clin Oncol 19:4097-4106, 2001.
33. Dunst J, Reese T, Sutter T, et al: Phase I trial evaluating the concurrent combination of radiotherapy and capecitabine in rectal cancer. J Clin Oncol 20:3983-3991, 2002.
34. Korkolis DP, Boskos CS, Plataniotis GD, et al: Pre-operative chemoradiotherapy with oral capecitabine in locally advanced, resectable rectal cancer. Anticancer Res 27:541-545, 2007.
35. De Paoli A, Chiara S, Luppi G, et al: Capecitabine in combination with preoperative radiation therapy in locally advanced, resectable, rectal cancer: a multicentric phase II study. Ann Oncol 17:246-251, 2006.
36. Krishnan S, Janjan NA, Skibber JM, et al: Phase II study of capecitabine (Xeloda) and concomitant boost radiotherapy in patients with locally advanced rectal cancer. Int J Radiat Oncol Biol Phys 66:762-771, 2006.
37. Kim JS, Cho MJ, Yoon WH, et al: Comparison of the efficacy of oral capecitabine vs bolus 5-FU in preoperative radiotherapy of locally advanced rectal cancer. J Korean Med Sci 21:52-57, 2006.
38. Kim DY, Jung KH, Kim TH, et al: Comparison of 5-fluorouracil/leucovorin and capecitabine in preoperative chemoradiotherapy for locally advanced rectal cancer. Int J Radiat Oncol Biol Phys 67:378-384, 2007.
39. Das P, Lin EH, Bhatia S, et al: Preoperative chemoradiotherapy with capecitabine vs protracted infusion 5-fluorouracil for rectal cancer: A matched-pair analysis. Int J Radiat Oncol Biol Phys 66:1378-1383, 2006.
40. de Gramont A, Figer A, Seymour M, et al: Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol 18:2938-2947, 2000.
41. Goldberg RM, Sargent DJ, Morton RF, et al: A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol 22:23-30, 2004.
42. Ryan DP, Niedzwiecki D, Hollis D, et al: Phase I/II study of preoperative oxaliplatin, fluorouracil, and external-beam radiation therapy in patients with locally advanced rectal cancer: Cancer and Leukemia Group B 89901. J Clin Oncol 24:2557-2562, 2006.
43. Aschele C, Friso ML, Pucciarelli S, et al: A phase I-II study of weekly oxaliplatin, 5-fluorouracil continuous infusion and preoperative radiotherapy in locally advanced rectal cancer. Ann Oncol 16:1140-1146, 2005.
44. Gerard JP, Chapet O, Nemoz C, et al: Preoperative concurrent chemoradiotherapy in locally advanced rectal cancer with high-dose radiation and oxaliplatin-containing regimen: The Lyon R0-04 phase II trial. J Clin Oncol 21:1119-1124, 2003.
45. Sebag-Montefiore D, Glynne-Jones R, Falk S, et al: A phase I/II study of oxaliplatin when added to 5-fluorouracil and leucovorin and pelvic radiation in locally advanced rectal cancer: A Colorectal Clinical Oncology Group (CCOG) study. Br J Cancer 93:993-998, 2005.
46. de Gramont A, Boni C, Navarro M, et al: Oxaliplatin/5FU/LV in adjuvant colon cancer: Updated efficacy results of the MOSAIC trial, including survival, with a median follow-up of six years (abstract 4007). J Clin Oncol 25(18S):165s, 2007.
47. Giacchetti S, Perpoint B, Zidani R, et al: Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil-leucovorin as first-line treatment of metastatic colorectal cancer. J Clin Oncol 18:136-147, 2000.
48. Sebag-Montefiore D, Glynne-Jones R, Falk S, et al: . Preoperative radiation and oxaliplatin in combination with 5-fluorouracil (5-FU) and low-dose leucovorin (LV) in locally advanced rectal cancer (abstract 580). Proc Am Soc Clin Oncol 21:146a, 2002.
49. Cassidy J, Tabernero J, Twelves C, et al: XELOX (capecitabine plus oxaliplatin): Active first-line therapy for patients with metastatic colorectal cancer. J Clin Oncol 22:2084-2091, 2004.
50. Glynne-Jones R, Sebag-Montefiore D, Maughan TS, et al: A phase I dose escalation study of continuous oral capecitabine in combination with oxaliplatin and pelvic radiation (XELOX-RT) in patients with locally advanced rectal cancer. Ann Oncol 17:50-56, 2006.
51. Roedel C, Arnold D, Hipp M, et al, for the German Rectal Cancer Study Group. Multicenter phase II trial of preoperative radiotherapy with concurrent and adjuvant capecitabine and oxaliplatin in locally advanced rectal cancer (abstract 349). Presented at the 2006 Gastrointestinal Cancers Symposium; San Francisco, Calif; Jan 26-28, 2006.
52. Rutten H, Sebag-Montefiore D, Glynne-Jones R, et al: Capecitabine, oxaliplatin, radiotherapy, and excision (CORE) in patients with MRI-defined locally advanced rectal adenocarcinoma: Results of an international multicenter phase II study (abstract 3528). J Clin Oncol 24(18S):153s, 2006.
53. Machiels JP, Duck L, Honhon B, et al: Phase II study of preoperative oxaliplatin, capecitabine and external beam radiotherapy in patients with rectal cancer: The RadiOxCape study. Ann Oncol 16:1898-1905, 2005.
54. Alonso V, Lambea J, Salud A, et al: Preoperative chemoradiotherapy with capecitabine and oxaliplatin in locally advanced rectal carcinoma: A phase II trial (abstract 4044). J Clin Oncol 25(18S):174s, 2007.
55. Ofner D, de Vries A, Thaler J, et al: Preoperative oxaliplatin (O), capecitabine (X), and external beam radiotherapy (RT) in patients (pts) with newly diagnosed, primary operable, locally advanced rectal cancer (LARC) (abstract 14527). J Clin Oncol 25(18S):627s, 2007.
56. Carlomagno C, Ferrante A, Solla R, et al: Preoperative chemoradiation therapy with capecitabine (CAP) and oxaliplatin (OX) in locally advanced rectal cancer (LARC): A phase II study (abstract 301). Presented at the 2007 Gastrointestinal Cancers Symposium; Orlando, Fla; Jan 19-21, 2007.
57. Salimichokami M, Vafai M, Derakhshani S, et al: Phase-2 study of neoadjuvant chemoradiation in locally advanced rectal adenocarcinoma: The Radio-Xelox study (abstract 13549). J Clin Oncol 24(18S):620s, 2006.
58. Rodel C, Grabenbauer GG, Papadopoulos T, et al: Phase I/II trial of capecitabine, oxaliplatin, and radiation for rectal cancer. J Clin Oncol 21:3098-3104, 2003.
59. Fakih MG: A phase I study of weekly intravenous oxaliplatin in combination with oral daily capecitabine and radiation therapy in the neoadjuvant treatment of rectal adenocarcinoma. Int J Radiat Oncol Biol Phys 65:1462-1470, 2006.
60. Fakih MG, Puthillath A, Yang G, et al: A phase II study of weekly intravenous oxaliplatin in combination with oral daily capecitabine and radiation therapy with biological correlates in the neoadjuvant treatment of rectal adenocarcinoma. Int J Radiat Oncol Biol Phys. In press.
61. Haller DG, Cassidy J, Clarke S, et al: Tolerability of fluoropyrimidines appears to differ by region (abstract 3514). J Clin Oncol 24(18S):149s, 2006.
62. Conti JA, Kemeny NE, Saltz LB, et al: Irinotecan is an active agent in untreated patients with metastatic colorectal cancer. J Clin Oncol 14:709-715, 1996.
63. Pitot HC, Wender DB, O’Connell MJ, et al: Phase II trial of irinotecan in patients with metastatic colorectal carcinoma. J Clin Oncol 15:2910-2919, 1997.
64. Rougier P, Bugat R, Douillard JY, et al: Phase II study of irinotecan in the treatment of advanced colorectal cancer in chemotherapy-naive patients and patients pretreated with fluorouracil-based chemotherapy. J Clin Oncol 15:251-260, 1997.
65. Rougier P, Van Cutsem E, Bajetta E, et al: Randomised trial of irinotecan vs fluorouracil by continuous infusion after fluorouracil failure in patients with metastatic colorectal cancer. Lancet 352:1407-1412, 1998.
66. Rothenberg ML, Eckardt JR, Kuhn JG, et al: Phase II trial of irinotecan in patients with progressive or rapidly recurrent colorectal cancer. J Clin Oncol 14:1128-1135, 1996.
67. Rothenberg ML, Cox JV, DeVore RF, et al: A multicenter, phase II trial of weekly irinotecan (CPT-11) in patients with previously treated colorectal carcinoma. Cancer 85:786-795, 1999.
68. Saltz LB, Cox JV, Blanke C, et al: Irinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. Irinotecan Study Group. N Engl J Med 343:905-914, 2000.
69. Mitchell EP: Irinotecan in preoperative combined-modality therapy for locally advanced rectal cancer. Oncology (Williston Park) 14:56-59, 2000.
70. Klautke G, Feyerherd P, Ludwig K, et al: Intensified concurrent chemoradiotherapy with 5-fluorouracil and irinotecan as neoadjuvant treatment in patients with locally advanced rectal cancer. Br J Cancer 92:1215-1220, 2005.
71. Mohiuddin M, Winter K, Mitchell E, et al: Randomized phase II study of neoadjuvant combined-modality chemoradiation for distal rectal cancer: Radiation Therapy Oncology Group Trial 0012. J Clin Oncol 24:650-655, 2006.
72. Navarro M, Dotor E, Rivera F, et al: A Phase II study of preoperative radiotherapy and concomitant weekly irinotecan in combination with protracted venous infusion 5-fluorouracil, for resectable locally advanced rectal cancer. Int J Radiat Oncol Biol Phys 66:201-205, 2006.
73. Glynne-Jones R, Falk S, Maughan TS, et al: A phase I/II study of irinotecan when added to 5-fluorouracil and leucovorin and pelvic radiation in locally advanced rectal cancer: A Colorectal Clinical Oncology Group Study. Br J Cancer 96:551-558, 2007.
74. Hofheinz R-D, von Gerstenberg-Helldorf B, Wenz F, et al: Phase I trial of capecitabine and weekly irinotecan in combination with radiotherapy for neoadjuvant therapy of rectal cancer. J Clin Oncol 23:1350-1357, 2005.
75. Willeke F, Horisberger K, Kraus-Tiefenbacher U, et al: A phase II study of capecitabine and irinotecan in combination with concurrent pelvic radiotherapy (CapIri-RT) as neoadjuvant treatment of locally advanced rectal cancer. Br J Cancer 96:912-917, 2007.
76. Klautke G, Kuchenmeister U, Foitzik T, et al: Concurrent chemoradiation with capecitabine and weekly irinotecan as preoperative treatment for rectal cancer: Results from a phase I/II study. Br J Cancer 94:976-981, 2006.
77. Becerra CR, Cho L, Gregorcyk S, et al: A phase I study with irinotecan, capecitabine and radiation therapy for patients with locally advanced or metastatic rectal cancer (abstract 212). Presented at the 2005 Gastrointestinal Cancers Symposium; Hollywood, Fla; Jan 27-29, 2005.
78. Gollins SW, Myint S, Levine E, et al: Radiotherapy plus concurrent irinotecan (CPT-11) and capecitabine (CAP) as preoperative downstaging treatment for locally advanced inoperable rectal cancer: A phase I/II study (abstract 13519). J Clin Oncol 24(18S):617s, 2006.
79. Mitchell EP, Anne P, Goldstein S, et al: Combined modality therapy of locally advanced adenocarcinoma of the rectum: Update of a phase I trial of preoperative radiation (RT) with concurrent capecitabine (Cap) and irinotecan (Ir) (abstract 13547). J Clin Oncol 24(18S):619s, 2006.
80. Privitera G, Spatola C, Acquaviva G, et al: Neoadjuvant XELOX vs XELIRI in combination with concomitant boost 3D-conformal radiotherapy in locally advanced rectal cancer (LARC) (abstract 3570). J Clin Oncol 24(18S):163s, 2006.
81. Chin KF, Greenman J, Gardiner E, et al: Pre-operative serum vascular endothelial growth factor can select patients for adjuvant treatment after curative resection in colorectal cancer. Br J Cancer 83:1425-1431, 2000.
82. Hyodo I, Doi T, Endo H, et al: Clinical significance of plasma vascular endothelial growth factor in gastrointestinal cancer. Eur J Cancer 34:2041-2045, 1998.
83. Nanashima A, Ito M, Sekine I, et al: Significance of angiogenic factors in liver metastatic tumors originating from colorectal cancers. Dig Dis Sci 43:2634-2640, 1998.
84. Hurwitz H, Fehrenbacher L, Novotny W, et al: Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350:2335-2342, 2004.
85. Giantonio BJ, Levy DE, O’Dwyer PJ, et al: A phase II study of high-dose bevacizumab in combination with irinotecan, 5-fluorouracil, leucovorin, as initial therapy for advanced colorectal cancer: results from the Eastern Cooperative Oncology Group study E2200. Ann Oncol 17:1399-1403, 2006.
86. Giantonio BJ, Catalano PJ, Meropol NJ, et al: Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: Results from the Eastern Cooperative Oncology Group study E3200. J Clin Oncol 25:1539-1544, 2007.
87. Hochster HS, Hart LL, Ramanathan RK, et al: Safety and efficacy of oxaliplatin/fluoropyrimidine regimens with or without bevacizumab as first-line treatment of metastatic colorectal cancer (mCRC): Final analysis of the TREE-study (abstract 3510). J Clin Oncol 24(18S):148s, 2006.
88. Hochster HS, Welles L, Hart L, et al: Safety and efficacy of bevacizumab (Bev) when added to oxaliplatin/fluoropyrimidine (O/F) regimens as first-line treatment of metastatic colorectal cancer (mCRC): TREE 1 & 2 studies (abstract 3515). J Clin Oncol 23(16S):249s, 2005.
89. Mauceri HJ, Hanna NN, Beckett MA, et al: Combined effects of angiostatin and ionizing radiation in antitumour therapy. Nature 394:287-291, 1998.
90. Willett C, Duda D, Boucher Y, et al: Phase I/II study of neoadjuvant bevacizumab with radiation therapy and 5-fluorouracil in patients with rectal cancer: initial results (abstract 4041). J Clin Oncol 25(18S):173s, 2007.
91. Privitera G, Spatola C, Acquaviva G, et al: Addition of bevacizumab (beva) to xeliri/xelox chemoradiotherapy in neoadjuvant setting for patients (pts) with locally advanced rectal cancer (LARC): A feasibility study (abstract 14583). J Clin Oncol 25(18S):631s, 2007.
92. Czito BG, Bendell JC, Willett CG, et al: Bevacizumab, oxaliplatin, and capecitabine with radiation therapy in rectal cancer: Phase I trial results. Int J Radiat Oncol Biol Phys 68:472-478, 2007.
93. Crane C, Eng C, Chang G, et al: Preliminary results of a phase II trial concurrent bevacizumab with neoadjuvant capecitabine based chemoradiation for locally advanced rectal cancer (abstract SS-10). Oncology 5(suppl 2):4, 2007.
94. Saltz LB, Meropol NJ, Loehrer PJ Sr, et al: Phase II trial of cetuximab in patients with refractory colorectal cancer that expresses the epidermal growth factor receptor. J Clin Oncol 22:1201-1208, 2004.
95. Lenz H-J, Van Cutsem E, Khambata-Ford S, et al: Multicenter phase II and translational study of cetuximab in metastatic colorectal carcinoma refractory to irinotecan, oxaliplatin, and fluoropyrimidines. J Clin Oncol 24:4914-4921, 2006.
96. Eng C, Maurel J, Scheithauer W, et al: Impact on quality of life of adding cetuximab to irinotecan in patients who have failed prior oxaliplatin-based therapy: The EPIC trial (abstract 4003). J Clin Oncol 25(18S):164s, 2007.
97. Cunningham D, Humblet Y, Siena S, et al: Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med 351:337-345, 2004.
98. Chung KY, Minsky B, Schrag D, et al: Phase I trial of preoperative cetuximab with concurrent continuous infusion 5-fluorouracil and pelvic radiation in patients with local-regionally advanced rectal cancer (abstract 3560). J Clin Oncol 24(18S):161s, 2006.
99. Machiels JP, Sempoux C, Scalliet P, et al: Phase I/II study of preoperative cetuximab, capecitabine, and external beam radiotherapy in patients with rectal cancer. Ann Oncol 18:738-744, 2007.
100. Hofheinz RD, Horisberger K, Woernle C, et al: Phase I trial of cetuximab in combination with capecitabine, weekly irinotecan, and radiotherapy as neoadjuvant therapy for rectal cancer. Int J Radiat Oncol Biol Phys 66:1384-1390, 2006.
101. Rödel C, Arnold D, Hipp M, et al: Phase I-II Trial of cetuximab, capecitabine, oxaliplatin, and radiotherapy as preoperative treatment in rectal cancer. Int J Radiat Oncol Biol Phys 70:1081-1086, 2007.
102. Engstrom PF, Arnoletti JP, Benson AB 3rd, et al: Rectal cancer. J Natl Compr Canc Netw 5:940-981, 2007.
103. Saltz LB, Niedzwiecki D, Hollis D, et al: Irinotecan fluorouracil plus leucovorin is not superior to fluorouracil plus leucovorin alone as adjuvant treatment for stage III colon cancer: Results of CALGB 89803. J Clin Oncol 25:3456-3461, 2007.
104. Van Cutsem E, Labianca R, Hossfeld D, et al: Randomized phase III trial comparing infused irinotecan/5-fluorouracil (5-FU)/folinic acid (IF) vs 5-FU/FA (F) in stage III colon cancer patients (pts) (PETACC 3) (abstract LBA8). J Clin Oncol 23(16S):3s, 2005.
105. Lievre A, Bachet JB, Boige V, et al: KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol 26:374-379, 2008.
106. Glynne-Jones R, Sebag-Montefiore D, Samuel L, et al: Socrates phase II study results: Capecitabine (CAP) combined with oxaliplatin (OX) and preoperative radiation (RT) in patients (pts) with locally advanced rectal cancer (LARC) (abstract 3527). J Clin Oncol 23:252s, 2005.
107. Collette L, Bosset JF, den Dulk M, et al: Patients with curative resection of cT3-4 rectal cancer after preoperative radiotherapy or radiochemotherapy: Does anybody benefit from adjuvant fluorouracil-based chemotherapy? A trial of the European Organisation for Research and Treatment of Cancer Radiation Oncology Group. J Clin Oncol 25:4379-4386, 2007.
108. Andre T, Boni C, Mounedji-Boudiaf L, et al: Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 350:2343-2351, 2004.