New Genomic Assays May Help Individualize Breast Cancer Treatment
Two new genomic assays may provide prognostic and predictive information for individual patients with breast cancer, thereby helping to guide treatment decisions, according to data from a pair of studies presented at SABCS.
Two new genomic assays may provide prognostic and predictive information for individual patients with breast cancer, thereby helping to guide treatment decisions, according to data from a pair of studies presented at SABCS.
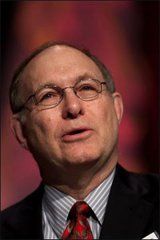
Joe W. Gray, PhD
Photo Courtesy SABCS/Todd Buchanan 2007
In the first study (abstract 31), Joe W. Gray, PhD, of the University of California, San Francisco, and colleagues identified six genes whose levels of transcription were associated with a response to lapatinib (Tykerb) in vitro. Expression of the genes can be easily measured in a single paraffin section with a technique called the branch capture assay, he said. The investigators assessed the 6-gene signature clinically using tissue and data from the EGF30001 randomized trial. Among HER2-positive patients, the risk of breast cancer progression was marginally reduced with paclitaxel-lapatinib therapy for patients predicted to be sensitive to lapatinib by the signature, compared with their counterparts predicted to not be sensitive (hazard ratio, 0.58). In contrast, the signature was not useful for risk stratification among HER2-negative patients treated with paclitaxel-lapatinib.
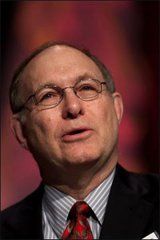
John Foekens, PhD
Photo Courtesy SABCS/Todd Buchanan 2007
"This [branch capture] assay ... is a multiwell assay, and it's actually quite possible to run literally hundreds of thousands of samples fairly conveniently in a few weeks," Dr. Gray said. "So it's an assay that can be propagated pretty broadly." He estimated that if offered clinically, the assay would cost less than $100. In the second study (abstract 32), John A. Foekens, PhD, of the Erasmus Medical Center in Rotterdam, the Netherlands, and coinvestigators assessed genomic predictors of distant recurrence in 313 patients with primary, lymph-node-negative breast cancer who did not receive any neoadjuvant or adjuvant systemic therapy. Median follow-up was 8.5 years. Among the 200 patients in the training set, analyses identified an 81-gene copy number signature (CNS) predictive of distant recurrence, much like a previously identified 76-gene gene expression signature (GES), according to Dr. Foekens. Among the 113 patients in the validation set, when compared with patients who had a good CNS, those with a poor CNS were significantly more likely to develop metastases (hazard ratio, 2.8). Moreover, 5-year metastasis-free survival was 90% with both good CNS and good GES, 63% with good CNS but poor GES, and 33% with poor CNS and poor GES. In multivariate analyses including conventional risk factors, patients with a poor CNS-GES combination versus a good one had a significantly higher risk of metastasis (hazard ratio, 4.9). Finally, using data from separate studies testing different chemotherapy regimens, the investigators found that poor prognosis as predicted by the two signatures appeared to be associated with greater sensitivity to doxorubicin, topotecan (Hycamtin), and etoposide, but greater resistance to cyclophosphamide, paclitaxel, and 5-fluorouracil. "Our copy number signature provides prognostic information additional to our gene expression signature," Dr. Foekens said. "And based on published predictive gene expression signatures, the patients in the different risk groups defined by the gene expression and the copy number signatures may be sensitive to specific drugs while being resistant to others."
Disclosures:
The author(s) have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.