New Small Molecule TKI Active in Thyroid Cancer
Axitinib (AG-013736), an oral small molecule tyrosine kinase inhibitor (TKI), yielded a 30% response rate in a phase II study of patients with metastatic or unresectable thyroid cancer unresponsive to or not suitable for standard treatment with radioactive iodine.
ASCO-Axitinib (AG-013736), an oral small molecule tyrosine kinase inhibitor (TKI), yielded a 30% response rate in a phase II study of patients with metastatic or unresectable thyroid cancer unresponsive to or not suitable for standard treatment with radioactive iodine. Ezra E.W. Cohen, MD, reported the results of the 60-patient single-arm multicenter trial at the 2007 meeting of the American Society of Clinical Oncology (abstract 6008). Dr. Cohen is director, Head and Neck Oncology Program, University of Chicago.
Referring to axitinib as a "potent and selective inhibitor of VEGF receptors 1, 2, and 3," he pointed out that the IC50's for inhibition of these three receptors by axitinib "are in the subnanomolar range."
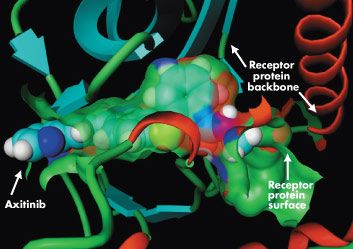
Used with permission from Pfizer.
Malignant thyroid tissue has been found to contain elevated levels of VEGF, compared with normal tissue. Axitinib, in development by Pfizer, has activity not only against VEGFR 1, 2, and 3 (picomolar potency), but also against PDGF-beta receptor and KIT (nanomolar potency).
All study patients had failed treatment with radioactive iodine or were unsuitable for this therapy (ie, those with medullary thyroid cancer). All histologic subtypes of thyroid cancer were allowed. Most patients had undergone prior surgery (88%) and prior treatment with radioactive iodine (70%). Nearly half had received prior external beam radiotherapy. A few had received prior chemotherapy (15%).
Patients received axitinib at a starting dose of 5 mg orally twice a day. They were assessed radiographically at baseline and every 8 weeks. A total of 24 patients remained in the trial as of May 2007, and 36 patients had discontinued therapy, 18 because of disease progression. The most common treatment-related adverse events included hypertension, fatigue, diarrhea/nausea, stomatitis/mucositis, and proteinuria. There was a low incidence of grade 3-4 adverse events, and there were no treatment-related deaths.
At a median follow-up of just over 1 year, the partial response rate was 30% (18 patients), 42% (25 patients) had stable disease lasting 16 weeks or longer. Patients with the greatest degree of tumor shrinkage, he said, had the greatest decrease in levels of soluble VEGFR2. Median progression-free survival was 18.6 months. A pivotal trial of axitinib in patients with doxorubicin-refractory thyroid cancer is actively accruing patients, he said.